Chagas disease
| Chagas disease Classification and external resources | |
| An acute Chagas' disease infection with swelling of the right eye (Romaña's sign). Source: CDC. | |
| ICD-10 | B57 |
| ICD-9 | 086 |
| DiseasesDB | 13415 |
| MedlinePlus | 001372 |
| eMedicine | med/327 |
| MeSH | D014355 |
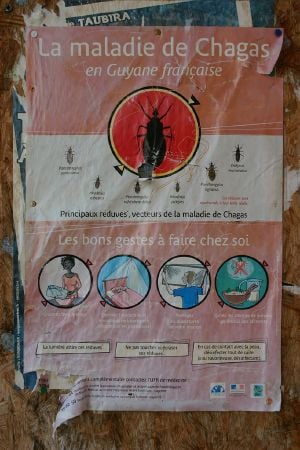
Chagas' disease, or American trypanosomiasis, is a tropical acute and chronic parasitic disease of the Americas caused by the flagellate protozoan Trypanosoma cruzi. T. cruzi is commonly transmitted to humans and other mammals by an insect vector, the blood-sucking assassin bugs of the subfamily Triatominae (family Reduviidae). The disease may also be spread through blood transfusion, ingestion of food contaminated with parasites, and from a mother to her fetus.
Chagas' disease kills about 50,000 people each year and affects about 15 million people or more.[1] There are three phases related to the infection, beginning with an acute phase that lasts a few weeks or months with only mild symptoms, an intermediate phase that lasts perhaps ten to twenty years without symptoms, and a chronic phase when serious symptoms can appear, such as heart disease and malformation of the intestines.[1] Acute cases are treated with nifurtimox and benznidazole, but there is currently no effective therapy for chronic cases.
Chagas' disease occurs exclusively in the Americas, particularly in poor, rural areas of Mexico, Central America, and South America. Very rarely, the disease has originated in the southern United States.
The ineffectiveness of drug treatment makes prevention all that more important. Control strategies have mostly focused on eliminating the triatomine vector and preventing transmission from blood transfusion, organ transplantation, and from mother to child.[2] Improving housing and sanitary conditions are likewise valued strategies, as is the use of mosquito nets and the proper cooking of food, since uncooked, contaminated food is another route for the infection.
Causal agent
The causal agent of Chagas' disease is Trypanosoma cruzi, a species of parasitic euglenoid trypanosomes. In the disease in humans, the T. cruzi exhibits two forms, a trypomastigote found in blood and an amastigote found in tissues.
Trypanosoma cruzi's life cycle starts in an animal reservoir. These reservoirs are usually mammals, wild or domestic, and include humans. A triatomine bug serves as the vector. While taking a blood meal, the triatomine sucks up the T. cruzi. In the triatomine bug, they go into the epimastigote stage. This makes it possible to reproduce. After reproducing through mitosis, the epimastigotes move onto the rectal cell wall. There, they become infectious.
Infectious T. cruzi are called trypomastigotes. While the triatomine bug is taking a blood meal from a human, it defecates. The trypomastigotes are in the feces, and can enter the human host through the bite wound or by crossing mucous membranes.
When they enter a human cell, they become amastigotes. This is another reproductive stage. After reproducing through mitosis until a large amount of amastigotes are in a cell, pseudocysts are formed in infected cells. The amastigotes then turn back into trypomastigotes, and the cell bursts. The typomastigotes swim along to either infect other cells or get sucked up by other triatomine bugs.
Transmission
In Chagas'-endemic areas, the main mode of transmission of the parasite is through a insect vector called a triatomine bug. This is an insect of the subfamily Triatominae (family Reduviidae). Most of the 130 or more species of this subfamily are haematophagous, i.e. feed on vertebrate blood. Transmission of T. cruzi most commonly involves species belonging to the Triatoma, Rhodnius, and Panstrongylus genera. The insects that spread the disease are known by various local names, including vinchuca in Argentina, barbeiro (the barber) in Brazil, "Pito" in Colombia, chipo, chupança, chinchorro, and the kissing bug.
Transmission typically occurs when the reduviid bug deposits feces on the skin surface and subsequently bites; the human host then scratches the bite area and facilitates penetration of the infected feces. The insects are very common in Central and South America and inhabit poorly constructed huts and houses.[1]
A triatomine first becomes infected with T. cruzi by feeding on the blood of an infected person or animal. During the day, triatomine hide in crevices in the walls and roofs. The bugs emerge at night, when the inhabitants are sleeping. Because they tend to feed on people’s faces, triatomine bugs are also known as “kissing bugs.” After they bite and ingest blood, they defecate on the person. Triatomine pass T. cruzi parasites (called trypomastigotes) in feces left near the site of the bite wound. Scratching the site of the bite causes the trypomastigotes to enter the host through the wound, or through intact mucous membranes, such as the conjunctiva. Once inside the host. the trypomastigotes invade cells, where they differentiate into intracellular amastigotes. The amastigotes multiply by binary fission and differentiate into trypomastigotes, which are then are released into the bloodstream. This cycle is repeated in each newly infected cell. Replication resumes only when the parasites enter another cell or are ingested by another vector.
T. cruzi can also be transmitted through blood transfusions, organ transplantation, breast milk,[3] and by accidental laboratory exposure. Chagas' disease can also be spread congenitally (from a pregnant woman to her baby) through the placenta, and accounts for approximately 13 percent of stillborn deaths in parts of Brazil.[4]
There have been other means of transmission reported, including through eating uncooked, contaminated food.[1] In 1991, farm workers in the state of Paraíba, Brazil, were infected by eating contaminated food; transmission has also occurred via contaminated acai palm fruit juice and sugar cane juice.[5][6][7] Despite many warnings in the press and by health authorities, this source of infection continues unabated.
Symptoms
There are three phases related to the disease:[1]
- Acute phase. An acute stage occurs shortly after an initial infection and lasts for the first few weeks or months of infection. In the early, acute stage, symptoms are mild and usually produce no more than local swelling at the site of infection. There may be low grade fever, fatigue, headache, and enlarged liver and spleen.
- Indeterminate phase. This phase lasts perhaps ten to 20 years and lack symptoms, although the parasites are reproducing in various parts of the body.
- Chronic phase. This stage develops after many years and has serious symptoms involving damage to major organs, such as the heart, esophagus, and colon.
The acute phase usually occurs unnoticed because it is symptom free or exhibits only mild symptoms and signs that are not unique to Chagas disease. The symptoms noted by the patient can include fever, fatigue, body aches, headache, rash, loss of appetite, diarrhea, and vomiting. The signs on physical examination can include mild enlargement of the liver or spleen, swollen glands, and local swelling (a chagoma) where the parasite entered the body. The most recognized marker of acute Chagas disease is called Romaña's sign, which includes swelling of the eyelids on the side of the face near the bite wound or where the bug feces were deposited or accidentally rubbed into the eye. Even if symptoms develop during the acute phase, they usually resolve spontaneously within three to eight weeks in approximately 90 percent of individuals.[8] Although the symptoms resolve, the infection, if untreated, persists. Rarely, young children (<5 percent) die from severe inflammation/infection of the heart muscle (myocarditis) or brain (meningoencephalitis). The acute phase also can be severe in people with weakened immune systems.[2]
In about 10 percent of infections, the symptoms do not completely resolve and result in a so-called chronic latent or indeterminate asymptomatic phase of the disease.
Several years or even decades after initial infection, an estimated 30 percent of infected people will develop medical problems from Chagas' disease over the course of their lives. The symptomatic chronic stage affects the nervous system, digestive system, and heart. About two-thirds of people with chronic symptoms have cardiac damage, including cardiomyopathy, which causes heart rhythm abnormalities and may result in sudden death. About one-third of patients go on to develop digestive system damage, resulting in dilation of the digestive tract (megacolon and megaesophagus), accompanied by severe weight loss. Swallowing difficulties may be the first symptom of digestive disturbances and may lead to malnutrition. Problems with the esophagus can lead to food regurgitating into the lungs, causing cough, bronchitis, and pneumonia.[1] Problems with the colon can lead to constipation, distention, and abdominal pain.[1] Twenty to fifty percent of individuals with intestinal involvement also exhibit cardiac involvement.[8] A small percentage of individuals develop various neurological disorders, including dementia.
The clinical manifestations of Chagas' disease are due to cell death in the target tissues that occurs during the infective cycle, by sequentially inducing an inflammatory response, cellular lesions, and fibrosis. For example, intracellular amastigotes destroy the intramural neurons of the autonomic nervous system in the intestine and heart, leading to megaintestine and heart aneurysms, respectively. If left untreated, Chagas' disease can be fatal, in most cases due to heart muscle damage.[8]
Diagnosis

The presence of T. cruzi is diagnostic of Chagas disease. It can be detected by Microscopic examination of fresh anti-coagulated blood, or its buffy coat, for motile parasites; or by preparation of thin and thick blood smears stained with Giemsa, for direct visualization of parasites. Microscopically, T. cruzi can be confused with Trypanosoma rangeli, which is not known to be pathogenic in humans. Isolation of T. cruzi can occur by inoculation into mice, by culture in specialized media (e.g., NNN, LIT); and by xenodiagnosis, where uninfected Reduviidae bugs are fed on the patient's blood, and their gut contents examined for parasites.
Various immunoassays for T. cruzi are available and can be used to distinguish among strains (zymodemes of T.cruzi with divergent pathogenicities). These tests include: detecting complement fixation, indirect hemagglutination, indirect fluorescence assays, radioimmunoassays, and ELISA. Alternatively diagnosis and strain identification can be made using polymerase chain reaction (PCR).
Antibody levels can be measured in the chronic phase as a diagnostic tool.[1]
Treatment
There are two approaches to treating Chagas disease, antiparasitic treatment, to kill the parasite; and symptomatic treatment, to manage the symptoms and signs of infection.
Current drug treatments are generally unsatisfactory, with the available drugs being highly toxic and often ineffective, particularly those used to treat the chronic stage of the disease. The duration and severity of an acute infections can be reduced, but only about 50 percent of medications are effective in eliminating the organisms.[1]
Antiparasitic treatment is most effective early in the course of infection but is not limited to cases in the acute phase. Drugs of choice include azole or nitro derivatives such as benznidazole[9] or nifurtimox. However, resistance to these drugs has been reported.[10] Moreover, 10-year study of chronic administration of antiparasitic drugs in Brazil has revealed that current drug treatment regimens do not fully remove parasitemia.[11] The anti-fungal agent Amphotericin B has been proposed as a second-line drug, but the high cost and relatively high toxicity of the drug have limited its use.
In the chronic stage, treatment involves managing the clinical manifestations of the disease. For example, pacemakers and medications for irregular heartbeats may be life saving for some patients with chronic cardiac disease, while surgery may be required for megaintestine. The disease cannot be cured in this phase, however. Chronic heart disease caused by Chagas' disease is now a common reason for heart transplantation surgery. Until recently, however, Chagas' disease was considered a contraindication for the procedure, since the heart damage could recur as the parasite was expected to seize the opportunity provided by the immunosuppression that follows surgery.[12] It was noted that survival rates in Chagas' patients could be significantly improved by using lower dosages of the immunosuppressant drug cyclosporin. Recently, direct stem cell therapy of the heart muscle using bone marrow cell transplantation has been shown to dramatically reduce risks of heart failure in Chagas patients.[13]
Several experimental treatments have shown promise in animal models. These include oxidosqualene cyclase inhibitors and cysteine protease inhibitors,[14] dermaseptins collected from Phyllomedusa (frog) species (Phyllomedusa oreades and P. distincta),[15] the sesquiterpene lactone dehydroleucodine (DhL), which affects the growth of cultured epimastigotes of Trypanosoma cruzi,[16] and inhibitors of enzymes involved in trypanothione metabolism.[17] It is hoped that new drug targets may be revealed following the sequencing of the T. cruzi genome.[18]
Prevention
Prevention of Chagas disease is generally focused on fighting the vector Triatoma by using sprays and paints containing insecticides (synthetic pyrethroids), and improving housing and sanitary conditions in rural areas. For urban dwellers, spending vacations and camping out in the wilderness or sleeping at hostels or mud houses in endemic areas can be dangerous; a mosquito net is recommended.
A reasonably effective vaccine was developed in Ribeirão Preto in the 1970s, using cellular and subcellular fractions of the parasite, but it was found economically unfeasible. More recently, the potential of DNA vaccines for immunotherapy of acute and chronic Chagas' disease is being tested by several research groups.[19]
According to the World Health Organization, the infection rate in Latin American blood banks varies between 3 percent and 53 percent, a figure higher than of HIV infection and hepatitis B and C.[20] In most countries where Chagas' disease is endemic, testing of blood donors is already mandatory, since this can be an important route of transmission. The United States FDA has recently licensed a test for antibodies against T. cruzi for use on blood donors but has not yet mandated its use. The American Association of Blood Banks recommends that past recipients of blood components from donors found to be infected be notified and themselves tested.[21] In the past, donated blood was mixed with 0.25g/L of gentian violet, which kills T. cruzi parasites.[22]
Prevalence and distribution
Chagas' disease currently affects 16–18 million people, with some 100 million (25 percent of the Latin American population) at risk of acquiring the disease,[20] killing around 50,000 people annually.[23]
The disease is distributed in the Americas, ranging from the southern United States to southern Argentina, mostly in poor, rural areas of Central and South America.[2] It is almost exclusively found in rural areas, where triatomine breed and feed on the natural reservoirs of T.cruzi. Recently, large-scale population movements from rural to urban areas of Latin America and to other regions of the world have increased the geographic distribution of Chagas' disease.
Depending on the special local interactions of the vectors and their hosts, other infected humans, domestic animals like cats, dogs, guinea pigs and wild animals like rodents, monkeys, ground squirrels (Spermophilus beecheyi) and many others could also serve as important parasite reservoirs. Though Triatominae bugs feed on birds, these seem to be immune against infection and therefore are not considered to be a T. cruzi reservoir; but there remain suspicions of them being a feeding resource for the vectors near human habitations. Even when colonies of insects are eradicated from a house and surrounding domestic animal shelters, they can arrive again (e.g., by flying) from plants or animals that are part of the ancient, natural sylvatic infection cycle. This can happen especially in zones with mixed open savannah, clumps of trees, and such interspersed by human habitation.
Dense vegetation, like in tropical rain forests, and urban habitats, are not ideal for the establishment of the human transmission cycle. However, in regions where the sylvatic habitat and its fauna are thinned out by economical exploitation and human habitation, such as in newly deforested, piassava palm (Leopoldinia piassaba) culture areas, and some parts of the Amazon region, this may occur, when the insects are searching for new prey.[24]
The primary wildlife reservoirs for Trypanosoma cruzi in the United States include opossums, raccoons, armadillos, squirrels, woodrats, and mice.[25] Opossums are particularly important as reservoirs because the parasite can complete its life cycle in the anal glands of the animal without having to re-enter the insect vector.[25] Recorded prevalence of the disease in opossums in the United States ranges from 8.3 percent[25] up to 37.5 percent.[26] Studies on raccoons in the Southeast have yielded infection rates ranging from 47 percent[27] to as low as 15.5 percent.[25] Armadillo prevalence studies have been described in Louisiana and range from a low of 1.1 percent[26] up to 28.8 percent.[28] Additionally small rodents including squirrels, mice, and rats are important in the sylvatic transmission cycle because of their importance as bloodmeal sources for the insect vectors. A Texas study revealed 17.3 percent percent T. cruzi prevalence in 75 specimens comprised of four separate small rodent species[29]
Chronic Chagas' disease remains a major health problem in many Latin American countries, despite the effectiveness of hygienic and preventive measures, such as eliminating the transmitting insects, which have reduced to zero new infections in at least two countries of the region. With increased population movements, however, the possibility of transmission by blood transfusion has become more substantial in the United States.[30] Approximately 500,000 infected people live in the US, which is likely the result of immigration from Latin American countries.[31]
Several landmarks have been achieved in the fight against Chagas' disease in Latin America including a reduction by 72 percent of the incidence of human infection in children and young adults in the countries of the Initiative of the Southern Cone, and at least two countries (Uruguay, in 1997, and Chile, in 1999), were certified free of vectorial and transfusional transmission. In Brazil, with the largest population at risk, 10 out of the 12 endemic states were also certified free.
Some stepstones of vector control include testing of a yeast trap for monitoring infestations of certain species of the bugs: Triatoma sordida, Triatoma brasiliensis, Triatoma pseudomaculata, and Panstrongylus megistus in laboratory assays.[32]. There also ahve been promising results with the treatment of vector habitats with the fungus Beauveria bassiana, (which is also in discussion for malaria- prevention).[33].
History
Chagas' disease is named after the Brazilian physician and infectologist Carlos Chagas, who first described it in 1909,[34][35][20] but the disease was not seen as a major public health problem in humans until the 1960s (the outbreak of Chagas' disease in Brazil in the 1920s went widely ignored[36]). He discovered that the intestines of Triatomidae harbored a flagellate protozoan, a new species of the Trypanosoma genus, and was able to prove experimentally that it could be transmitted to marmoset monkeys that were bitten by the infected bug. Later studies showed that squirrel monkeys were also vulnerable to infection.[37]
Chagas named the pathogenic parasite that causes the disease Trypanosoma cruzi[34] and later that year as Schizotrypanum cruzi,[38] both honoring Oswaldo Cruz, the noted Brazilian physician and epidemiologist who fought successfully epidemics of yellow fever, smallpox, and bubonic plague in Rio de Janeiro and other cities in the beginning of the twentieth century. Chagas’ work is unique in the history of medicine because he was the only researcher so far to describe solely and completely a new infectious disease: its pathogen, vector, host, clinical manifestations, and epidemiology. Nevertheless, he believed (falsely) until 1925 that the main infection route is by the bite of the insect, and not by its feces, as was proposed by his colleague Emile Brumpt in 1915 and supported by Silveira Dias in 1932, Cardoso in 1938, and Brumpt himself in 1939. Chagas was also the first to unknowingly discover and illustrate the parasitic fungal genus Pneumocystis, later infamously to be linked to PCP (Pneumocystis pneumonia in AIDS victims).[35] Confusion between the two pathogens' life cycles led him to briefly recognize the genus as Schizotrypanum, but following the description of Pneumocystis by others as an independent genus, Chagas returned to the use of the name Trypanosoma cruzi.
It has been hypothesized that Charles Darwin might have suffered from Chagas' disease as a result of a bite of the so-called Great Black Bug of the Pampas (vinchuca). The episode was reported by Darwin in his diaries of the Voyage of the Beagle as occurring in March 1835 to the east of the Andes near Mendoza. Darwin was young and generally in good health, though six months previously he had been ill for a month near Valparaiso, but in 1837, almost a year after he returned to England, he began to suffer intermittently from a strange group of symptoms, becoming incapacitated for much of the rest of his life. Attempts to test Darwin's remains at the Westminster Abbey by using modern PCR techniques were met with a refusal by the Abbey's curator.[39]
ReferencesISBN links support NWE through referral fees
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 D. Kaminstein, "Chagas' disease," pages 727-728 in J. L. Longe, The Gale Encyclopedia of Medicine, 2nd edition (Detroit: Gale Group/Thomson Learning, 2004). ISBN 0787654914.
- ↑ 2.0 2.1 2.2 Centers for Disease Control (CDC), Fact sheet: Trypanosomyasis, American,". Retrieved August 28, 2008.
- ↑ C. Santos Ferreira, V. Amato Neto, E. Gakiya, et al. "Microwave treatment of human milk to prevent transmission of Chagas disease," Rev Inst Med Trop São Paulo 45(2003)(issue 1): 41-2. PMID 12751321. Retrieved August 28, 2008.
- ↑ L. Hudson, and M. J. Turner, "Immunological consequences of infection and vaccination in South American Trypanosomiasis [and discussion,"] Philosophical Transactions of the Royal Society of London 307(1984)(issue 1131): 51-61. PMID 6151688. Retrieved August 28, 2008.
- ↑ UK Health Protection Agency (HPA), Chagas’ disease (American trypanosomiasis) in southern Brazil, CDR Weekly 15(2005)(issue 13).
- ↑ M. A. Shikanai-Yasuda, C. B. Marcondes, L. A. Guedes, et al., "Possible oral transmission of acute Chagas' disease in Brazil," Rev. Inst. Med. Trop. Sao Paulo 33(1991)(issue 5): 351–7. PMID 1844961. Retrieved August 28, 2008.
- ↑ A. S. da Silva Valente, V. de Costa Valente, and H. F. Neto, "Considerations on the epidemiology and transmission of Chagas disease in the Brazilian Amazon," Mem. Inst. Oswaldo Cruz 94(1999)(Suppl 1): 395–8. PMID 10677763. Retrieved August 28, 2008.
- ↑ 8.0 8.1 8.2 Y. Carlier, "Chagas' disease (American Trypanosomiasis)," eMedicine . Retrieved August 28, 2008.
- ↑ S. Garcia, C. O. Ramos, J. F. Senra, et al., "Treatment with benznidazole during the chronic phase of experimental Chagas' disease decreases cardiac alterations, Antimicrob. Agents Chemother. 49(2005)(issue 4): 1521–8. PMID 15793134. Retrieved August 28, 2008.
- ↑ F. S. Buckner, A. J. Wilson, T. C. White, and W. C. Van Voorhis, "Induction of resistance to azole drugs in Trypanosoma cruzi," Antimicrob. Agents Chemother. 42(1998)(12): 3245–50. PMID 9835521. Retrieved August 28, 2008.
- ↑ L. Lauria-Pires, M. S. Braga, A. C. Vexenat, et al., "Progressive chronic Chagas heart disease ten years after treatment with anti-Trypanosoma cruzi nitroderivatives," Am. J. Trop. Med. Hyg. 63(2000)(issue 3-4): 111–8. PMID 11388500. Retrieved August 28, 2008.
- ↑ E. A. Bocchi, G. Bellotti, A. O. Mocelin, et al., "Heart transplantation for chronic Chagas' heart disease," Ann. Thorac. Surg. 61(1996)(issue 6): 1727–33. PMID 8651775. Retrieved August 28, 2008.
- ↑ F. Vilas-Boas, G. S. Feitosa, M. B. Soares, et al. "Early results of bone marrow cell transplantation to the myocardium of patients with heart failure due to Chagas disease," Arq. Bras. Cardiol. 87(2006)(issue 2): 159–66. PMID 16951834. Retrieved August 28, 2008.
- ↑ J. C. Engel, P. S. Doyle, I. Hsieh, and J. H. McKerrow, "Cysteine protease inhibitors cure an experimental Trypanosoma cruzi infection," J. Exp. Med. 188(1998)(issue 4): 725–34. PMID 9705954. Retrieved August 28, 2008.
- ↑ G. D. Brand, J. R. Leite, L. P. Silva, et al., "Dermaseptins from Phyllomedusa oreades and Phyllomedusa distincta. Anti-Trypanosoma cruzi activity without cytotoxicity to mammalian cells," J. Biol. Chem. 277(2002)(issue 51): 49332–40. PMID 12379643. Retrieved August 28, 2008.
- ↑ S. D. Brengio, S. A. Belmonte, E. Guerreiro, O. S. Giordano, E. O. Pietrobon, and M. A. Sosa, "The sesquiterpene lactone dehydroleucodine (DhL) affects the growth of cultured epimastigotes of Trypanosoma cruzi, J. Parasitol. 86(2000)(issue 2): 407–12. PMID 10780563. Retrieved August 28, 2008.
- ↑ A. H. Fairlamb, and A. Cerami, "Metabolism and functions of trypanothione in the Kinetoplastida," Annu. Rev. Microbiol. 46(1992): 695–729. PMID 1444271. Retrieved August 28, 2008.
- ↑ N. M. El-Sayed, P. J. Myler, D. C. Bartholomeu, et al., "The genome sequence of Trypanosoma cruzi, etiologic agent of Chagas disease. Science 309(2005)(issue 5733): 409–15. PMID 16020725. Retrieved August 28, 2008.
- ↑ E. Dumonteil, J. Escobedo-Ortegon, N. Reyes-Rodriguez, A. Arjona-Torres, and M. Ramirez-Sierra, "Immunotherapy of Trypanosoma cruzi infection with DNA vaccines in mice," Infect Immun 72(2004)(issue=1): 46–53. PMID 14688079. Retrieved August 28, 2008.
- ↑ 20.0 20.1 20.2 WHO, "Chagas," WHO/TDR (2004). Retrieved August 28, 2008.
- ↑ K. R. Gregory, "Chagas' disease," American Association of Blood Banks (2002). Retrieved August 28, 2008.
- ↑ R. Docampo, S. N. Moreno, R. P. Muniz, F. S. Cruz, and R. P. Mason, "Light-enhanced free radical formation and trypanocidal action of gentian violet (crystal violet)," Science 220(1983)(issue 4603): 1292–5. PMID 6304876. Retrieved August 28, 2008.
- ↑ Carlier, Yves. Chagas Disease (American Trypanosomiasis). eMedicine (27 February 2003).
- ↑ A. R. Teixeira, P. S. Monteiro, J. M. Rebelo, et al., "Emerging Chagas disease: Trophic network and cycle of transmission of Trypanosoma cruzi from palm trees in the Amazon," Emerging Infect. Dis. 7(200)(issue 1): 100–12. PMID 11266300. Retrieved August 28, 2008.
- ↑ 25.0 25.1 25.2 25.3 V. Karsten, C. Davis, and R. Kuhn, "Trypanosoma cruzi in wild raccoons and opossums in North Carolina," J. Parasitol. 78(1992)(issue 3): 547–9. PMID 1597808. Retrieved August 28, 2008.
- ↑ 26.0 26.1 S. C. Barr, C. C. Brown, V. A. Dennis, and T. R. Klei, "The lesions and prevalence of Trypanosoma cruzi in opossums and armadillos from southern Louisiana," J. Parasitol. 77(1991)(issue 4): 624–7. PMID 1907654. Retrieved August 28, 2008.
- ↑ M. M. Yabsley, and G. P. Noblet, "Seroprevalence of Trypanosoma cruzi in raccoons from South Carolina and Georgia," J. Wildl. Dis. 38(2002)(issue 1): 75–83. PMID 11838232. Retrieved August 28, 2008.
- ↑ R. G. Yaeger, "The prevalence of Trypanosoma cruzi infection in armadillos collected at a site near New Orleans, Louisiana," Am. J. Trop. Med. Hyg. 38(1988)(issue 2): 323–6 PMID 3128127. Retrieved August 28, 2008.
- ↑ J. E. Burkholder, T. C. Allison, and V. P. Kelly, "Trypanosoma cruzi (Chagas) (Protozoa: Kinetoplastida) in invertebrate, reservoir, and human hosts of the lower Rio Grande valley of Texas," J. Parasitol. 66(1980)(issue 2): 305–11. PMID 6771371. Retrieved August 28, 2008.
- ↑ L. V. Kirchhoff, "American trypanosomiasis (Chagas' disease)—a tropical disease now in the United States," N. Engl. J. Med. 329(1993)(issue 9): 639–44. PMID 8341339. Retrieved August 28, 2008.
- ↑ National Institutes of Health, Chagras' disease, Medline Plus (2008). Retrieved August 28, 2008.
- ↑ H. H. Pires, C. R. Lazzari, L. Diotaiuti, and M. G. Lorenzo, "Performance of yeast-baited traps with Triatoma sordida, Triatoma brasiliensis, Triatoma pseudomaculata, and Panstrongylus megistus in laboratory assays," Rev. Panam. Salud Publica 7(2000)(issue 6): 384–8. PMID 10949899. Retrieved August 28, 2008.
- ↑ C. Luz, L. F. Rocha, G. V. Nery, B. P. Magalhães, and M. S. Tigano, "Activity of oil-formulated Beauveria bassiana against Triatoma sordida in peridomestic areas in Central Brazil," Mem. Inst. Oswaldo Cruz 99(2004)(issue 2): 211–8. PMID 15250478. Retrieved August 28, 2008.
- ↑ 34.0 34.1 C. Chagas, "Neue Trypanosomen ," Vorläufige Mitteilung. Arch. Schiff. Tropenhyg. 13(1909): 120–122.
- ↑ 35.0 35.1 S. A. Redhead, M. T. Cushion, J. K. Frenkel, and J. R. Stringer, "Pneumocystis and Trypanosoma cruzi: Nomenclature and typifications," J Eukaryot Microbiol 53(2006)(issue 1): 2–11. PMID 16441572. Retrieved August 28, 2008.
- ↑ M. Perleth, "Historical aspects of American Trypanosomiasis (Chagas' disease) ," Isis 90(1999)(issue 2): 397-397.
- ↑ L. H. Hulsebos, L. Choromanski, and R. E. Kuhn, "The effect of interleukin-2 on parasitemia and myocarditis in experimental Chagas' disease," J. Protozool. 36(1989)(issue 3): 293–8. PMID 2499678. Retrieved August 28, 2008.
- ↑ C. Chagas, "Nova tripanozomiase humana: Estudos sobre a morfolojia e o ciclo evolutivo do Schizotrypanum cruzi n. gen., n. sp., ajente etiolojico de nova entidade morbida do homem," Mem Inst Oswaldo Cruz 1(1909)(issue 2): 159–218. (New human trypanosomiasis. Studies about the morphology and life-cycle of Schizotripanum cruzi, etiological agent of a new morbid entity of man.
- ↑ D. Adler, "Darwin's illness," Isr J Med Sci 25(1989)(issue 4): 218–21. PMID 2496051. Retrieved August 28,2008.
Further reading
- Bern. C., S. P. Montgomery, B. L. Herwaldt, et al. 2007. Evaluation and treatment of Chagas' disease in the United States: A systematic review. JAMA 298(18): 2171–81. PMID 18000201. Retrieved August 28, 2008.
- Coutinho, M. 1999. Ninety years of Chagas' disease: A success story at the periphery. Soc Stud Sci 29(4): 519–49. PMID 11623933. Retrieved August 28, 2008.
- Dias, J., A. Silveira, and C. Schofield. 2002. The impact of Chagas disease control in Latin America: A review. Mem Inst Oswaldo Cruz 97(5): 603–12. PMID 12219120. Retrieved August 28, 2008.
- Kropf, S., N.Azevedo, and L. Ferreira. 2003. Biomedical research and public health in Brazil: The case of Chagas' disease (1909–50). Soc Hist Med 16(1): 111–29. PMID 14598820. Retrieved August 28, 2008.
- Franco-Paredes, C. 2007. Chagas disease: An impediment in achieving the Millennium Development Goals in Latin America. BMC International Health and Human Rights 7: 7. PMID 17725836. Retrieved August 28, 2008.
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.