Difference between revisions of "Allergy" - New World Encyclopedia
Katya Swarts (talk | contribs) (Added article and credit tags) |
Rick Swarts (talk | contribs) (added most recent Wikipedia article) |
||
| Line 1: | Line 1: | ||
{{dablink|This article deals specifically with [[IgE]]-mediated hypersensitivity. For other types of allergic or hypersensitive reactions see the main article: [[Hypersensitivity]]}} | {{dablink|This article deals specifically with [[IgE]]-mediated hypersensitivity. For other types of allergic or hypersensitive reactions see the main article: [[Hypersensitivity]]}} | ||
| − | An '''allergy''' can refer to several kinds of immune reactions including '''Type I hypersensitivity''' in which | + | An '''allergy''' can refer to several kinds of immune reactions including '''Type I hypersensitivity''' in which the person's body is hypersensitised and develops [[immunoglobulin E]] (IgE) a certain type of antibodies to typical proteins. When a person is hypersensitised, these substances are known as [[allergen]]s. The word allergy derives from the [[Greek language|Greek]] words ''allos'' meaning "other" and ''ergon'' meaning "work". Type I hypersensitivity is characterised by excessive activation of [[mast cell]]s and basophils by immunoglobulin E resulting in a systemic [[Inflammation|inflammatory response]] that can result in symptoms as benign as a [[rhinorrhea|runny nose]], to life-threatening [[anaphylaxis|anaphylactic shock]] and [[death]]. |
| − | Allergy is a very common disorder and more than 50 million Americans suffer from allergic diseases. Allergies are the | + | Allergy is a very common disorder and more than 50 million Americans suffer from allergic diseases. Allergies are the sixth leading cause of chronic disease in the United States, costing the health care system $18 billion annually. |
== History == | == History == | ||
| − | The term and concept of | + | The term and concept of "allergy" was coined by a [[Vienna|Viennese]] [[pediatrician]] named [[Clemens von Pirquet]] in [[1906]].<ref>Clemens Peter Pirquet von Cesenatico {{WhoNamedIt|Doctor|2382}}</ref> He observed that the [[symptom]]s of some of his patients might have been a response to outside allergens such as [[dust]], [[pollen]], or certain [[foods]]. For a long time all [[hypersensitivities]] were thought to stem from the improper action of [[inflammatory]] [[immunoglobulin]] class IgE, however it soon became clear that several different mechanisms utilizing different effector molecules were responsible for the myriad of disorders previously classified as "allergies". A new four-class (now five) classification scheme was designed by P. G. H. Gell and R. R. A. Coombs. Allergy has since been kept as the name for Type I Hypersensitivity, characterised by classical IgE mediation of effects. |
==Signs and symptoms== | ==Signs and symptoms== | ||
Allergy is characterised by a local or systemic [[inflammation|inflammatory]] response to allergens. Local symptoms are: | Allergy is characterised by a local or systemic [[inflammation|inflammatory]] response to allergens. Local symptoms are: | ||
* [[Nose]]: swelling of the nasal mucosa ([[allergic rhinitis]]) | * [[Nose]]: swelling of the nasal mucosa ([[allergic rhinitis]]) | ||
| − | |||
* [[Eye]]s: redness and [[itch]]ing of the [[conjunctiva]] ([[allergic conjunctivitis]]) | * [[Eye]]s: redness and [[itch]]ing of the [[conjunctiva]] ([[allergic conjunctivitis]]) | ||
* [[Airway]]s: [[bronchoconstriction]], wheezing and dyspnoea, sometimes outright attacks of [[asthma]] | * [[Airway]]s: [[bronchoconstriction]], wheezing and dyspnoea, sometimes outright attacks of [[asthma]] | ||
| − | *[[Ear]]s: feeling of fullness, possibly pain, and impaired hearing due to the lack of [[eustachian tube]] drainage. | + | * [[Ear]]s: feeling of fullness, possibly pain, and impaired hearing due to the lack of [[eustachian tube]] drainage. |
* [[Skin]]: various [[rash]]es, such as [[eczema]], [[hives]] ([[urticaria]]) and [[contact dermatitis]]. | * [[Skin]]: various [[rash]]es, such as [[eczema]], [[hives]] ([[urticaria]]) and [[contact dermatitis]]. | ||
| + | * [[Head]]: while not as common, headaches are seen in some with environmental or chemical allergies. | ||
Systemic allergic response is also called [[anaphylaxis]]. Depending of the rate of severity, it can cause [[cutaneous]] reactions, bronchoconstriction, [[edema]], [[hypotension]], [[coma]] and even [[death]]. | Systemic allergic response is also called [[anaphylaxis]]. Depending of the rate of severity, it can cause [[cutaneous]] reactions, bronchoconstriction, [[edema]], [[hypotension]], [[coma]] and even [[death]]. | ||
| − | [[Hay fever]] is one example of an exceedingly common minor allergy | + | [[Hay fever]] is one example of an exceedingly common minor allergy — large percentages of the population suffer from hayfever symptoms in response to [[wiktionary:airborne|airborne]] [[pollen]]. [[Asthma]]tics are often allergic to [[house dust mite|dust mites]]. Apart from ambient allergens, allergic reactions can be due to [[medication]]s. |
==Diagnosis== | ==Diagnosis== | ||
| Line 30: | Line 30: | ||
===Problems with skin test=== | ===Problems with skin test=== | ||
| − | + | While the skin test is probably the most preferred means of testing because of its simplicity and economics, it is not without complications. Some people may display a delayed-type hypersensitivity (DTH) reaction which can occur as far as 6 hours after application of the allergen and last up to 24 hours. This can also cause serious long-lasting tissue damage to the affected area. These types of serious reactions are quite rare. | |
| − | While the skin test is probably the most preferred means of testing because of its simplicity and economics, it is not without complications. Some people may display a delayed-type hypersensitivity (DTH) reaction which can occur as far as 6 hours after application of the allergen and last up to 24 hours. This can also cause serious long-lasting tissue damage to the affected area. | ||
Additionally, the application of previously unencountered allergens can actually sensitize certain individuals to the allergen, causing the inception of a new allergy in susceptible individuals. | Additionally, the application of previously unencountered allergens can actually sensitize certain individuals to the allergen, causing the inception of a new allergy in susceptible individuals. | ||
| Line 38: | Line 37: | ||
===Total IgE count=== | ===Total IgE count=== | ||
| − | Another method used to qualify type I hypersensitivity is measuring the amount of serum IgE contained within the patient's [[serum]]. This can be determined through the use of radiometric and colormetric [[immunoassay]]s. Even the levels the amount of IgE specific to certain allergens can be measured through use of the radioallergosorbent test (RAST). | + | Another method used to qualify type I hypersensitivity is measuring the amount of serum IgE contained within the patient's [[blood plasma|serum]]. This can be determined through the use of radiometric and colormetric [[immunoassay]]s. Even the levels the amount of IgE specific to certain allergens can be measured through use of the [[RAST test|radioallergosorbent test]] (RAST). |
==Treatment== | ==Treatment== | ||
| Line 44: | Line 43: | ||
===Immunotherapy=== | ===Immunotherapy=== | ||
| − | [[Hyposensitization]] | + | [[Hyposensitization]] is a form of [[immunotherapy]] where the patient is gradually [[vaccination|vaccinated]] against progressively larger doses of the allergen in question. This can either reduce the severity or eliminate hypersensitivity altogether. It relies on the progressive skewing of [[IgG]] ("the blocking antibody") production, as opposed to the excessive IgE production seen in hypersensitivity type I cases. Delivery can occur via allergy injection, or [[sublingual immunotherapy]], allergy drops taken under the tongue. Though not commonly offered in the U.S., sublingual immunotherapy is gaining attention internationally and is very common in Europe. |
| − | + | A second form of immunotherapy involves the intravenous injection of [[monoclonal antibody|monoclonal]] anti-IgE antibodies. These bind to free and B-cell IgE signalling such sources for destruction. They do not bind to IgE already bound to the Fc receptor on [[basophil]]s and mast cells as this would stimulate the allergic inflammatory response. The first agent in this class is [[omalizumab]]. | |
| − | + | An experimental treatment form, [[enzyme potentiated desensitization]], has been tried with some success but is not in widespread use. EPD uses dilutions of allergen and an enzyme, [[beta-glucuronidase]], to which T-regulatory lymphocytes respond by favouring desensitization, or down-regulation, rather than sensitization. EPD is also under development for the treatment of [[autoimmune diseases]]. | |
===Chemotherapy=== | ===Chemotherapy=== | ||
| − | Several [[antagonism|antagonistic]] drugs are used to block the action of allergic mediators, preventing activation of cells and degranulation processes. They include [[antihistamine]]s, [[cortisone]], [[epinephrine]] (adrenalin), [[theophylline]] and [[Cromolyn sodium]]. These drugs help alleviate the symptoms of allergy but play little role in chronic alleviation of the disorder. They can play an imperative role in the acute recovery of someone suffering from anaphylaxis | + | Several [[antagonism|antagonistic]] drugs are used to block the action of allergic mediators, preventing activation of cells and degranulation processes. They include [[antihistamine]]s, [[cortisone]], [[epinephrine]] (adrenalin), [[theophylline]] and [[Cromolyn sodium]]. These drugs help alleviate the symptoms of allergy but play little role in chronic alleviation of the disorder. They can play an imperative role in the acute recovery of someone suffering from anaphylaxis, which is why those allergic to [[bee]] stings, [[peanut]]s, [[nut (fruit)|nuts]], and [[shellfish]] often carry an adrenalin needle with them at all times. |
===Alternative therapies=== | ===Alternative therapies=== | ||
| − | In [[alternative medicine]], a number of treatment modalities are considered effective by its practitioners in the treatment of allergies, particularly [[herbal medicine]], [[homeopathy]], [[traditional Chinese medicine]] and [[kinesiology]]. However, these claims lack | + | In [[alternative medicine]], a number of treatment modalities are considered effective by its practitioners in the treatment of allergies, particularly [[naturopathic]], [[herbal medicine]], [[homeopathy]], [[traditional Chinese medicine]] and [[kinesiology]]. These modalities are frequently offered as treatment for those seeking additional help when mainstream medicine has failed to provide adequate relief from allergy symptoms. However, mainstream physicians maintain that these claims lack a scientific basis and warn that the efficacy of such treatments is only supported by anecdotal evidence. |
==Pathophysiology== | ==Pathophysiology== | ||
| Line 62: | Line 61: | ||
The difference between a type I hypersensitivity reaction against an allergen to the normal [[humoral response]] against a foreign body is that [[plasma cell]]s secrete IgE as opposed to either IgM (against novel antigens) or IgG (against immunized antigens). IgE binds to Fc receptors on the surface of mast cells and basophils, both involved in the acute inflammatory response. | The difference between a type I hypersensitivity reaction against an allergen to the normal [[humoral response]] against a foreign body is that [[plasma cell]]s secrete IgE as opposed to either IgM (against novel antigens) or IgG (against immunized antigens). IgE binds to Fc receptors on the surface of mast cells and basophils, both involved in the acute inflammatory response. | ||
| − | When IgE is first secreted it binds to the Fc receptors on a mast cell or basophil, and such | + | When IgE is first secreted it binds to the Fc receptors on a mast cell or basophil, and such an IgE-coated cell is said to be sensitized to the allergen in question. A later exposure by the same allergen causes reactivation of these IgE, which then signals for the [[degranulation]] of the sensitized mast cell or basophil. There is now strong evidence that mast cells and basophils require costimulatory signals for degranulation in vivo, derived from GPCRs such as chemokine receptors. These granules release [[histamine]] and other inflammatory chemical mediators ([[cytokine]]s, [[interleukin]]s, [[leukotriene]]s, and [[prostaglandin]]s) into the surrounding tissue causing several systemic effects, such as [[vasodilation]], [[mucous]] secretion, [[nerve]] stimulation and [[smooth muscle]] contraction. This results in the previously described symptoms of rhinorrhea, itchiness, dyspnea, and [[anaphylaxis]]. Depending on the individual, allergen, and mode of introduction, the symptoms can be system-wide (calliscal anaphylaxis), or localised to particular body systems (for example, asthma to the respiratory system; eczema to the dermis). |
===Late-phase response=== | ===Late-phase response=== | ||
| Line 72: | Line 71: | ||
===Relationship with parasites=== | ===Relationship with parasites=== | ||
| − | Some recent research has also begun to show that some kinds of common parasites, such as intestinal worms (e.g. [[hookworm]]s), secrete [[immunosuppressant]] chemicals into the gut wall and hence the bloodstream which prevent the body from attacking the parasite. This gives rise to a new slant on the "[[hygiene hypothesis]]" | + | Some recent research has also begun to show that some kinds of common parasites, such as intestinal worms (e.g. [[hookworm]]s), secrete [[immunosuppressant]] chemicals into the gut wall and hence the bloodstream which prevent the body from attacking the parasite. This gives rise to a new slant on the "[[hygiene hypothesis]]" — that co-evolution of man and parasites has in the past led to an immune system that only functions correctly in the presence of the parasites. Without them, the immune system becomes unbalanced and oversensitive. Gutworms and similar parasites are present in untreated drinking water in undeveloped countries, and in developed countries until the routine chlorination and purification of drinking water supplies. This also coincides with the time period in which a significant rise in allergies has been observed.{{fact}} So far, there is only sporadic evidence to support this hypothesis — one scientist who suffered from seasonal allergic rhinitis (hayfever) infected himself with gutworms and was immediately 'cured' of his allergy with no other ill effects.{{fact}} Full clinical trials have yet to be performed however. It may be that the term 'parasite' could turn out to be inappropriate, and in fact a hitherto unsuspected [[symbiosis]] is at work.{{fact}} |
| − | immediately 'cured' of his allergy with no other ill effects.{{fact}} Full clinical trials have yet to be performed however. It may be that the term 'parasite' could turn out to be inappropriate, and in fact a hitherto unsuspected [[symbiosis]] is at work.{{fact}} | ||
==Basis of increasing prevalence== | ==Basis of increasing prevalence== | ||
| Line 83: | Line 81: | ||
Many common allergies such as asthma have seen huge increases in the years since the second world war, and many studies appear to show a correlation between this and the increasingly affluent and clean lifestyles in the [[Western world|West]]. This is supported by studies in less developed countries that do not enjoy western levels of cleanliness, and similarly do not show western levels of incidences of asthma and other allergies. During this same period, air quality, at one time considered the "obvious" cause of asthma, has shown a considerable improvement. This has led some researchers to conclude that it is our "too clean" upbringing that is to blame for the lack of immune system stimulation in early childhood. | Many common allergies such as asthma have seen huge increases in the years since the second world war, and many studies appear to show a correlation between this and the increasingly affluent and clean lifestyles in the [[Western world|West]]. This is supported by studies in less developed countries that do not enjoy western levels of cleanliness, and similarly do not show western levels of incidences of asthma and other allergies. During this same period, air quality, at one time considered the "obvious" cause of asthma, has shown a considerable improvement. This has led some researchers to conclude that it is our "too clean" upbringing that is to blame for the lack of immune system stimulation in early childhood. | ||
| − | So far the evidence to support this theory is limited. One supporting fact is that many [[Chinese]] will develop [[hay fever]] after moving into [[USA]] for three or more years. However, contradictory examples also exist. | + | So far the evidence to support this theory is limited. One supporting fact is that many [[Han Chinese|Chinese]] will develop [[hay fever]] after moving into [[USA]] for three or more years. However, contradictory examples also exist. |
===Increasing use of chemicals=== | ===Increasing use of chemicals=== | ||
Another theory is the exponential use and abuse of chemicals in affluent nations since the second world war. Vast numbers of chemicals are introduced into our indoor and outdoor environments with little or no testing regarding their toxicity to living beings. Many believe that air quality is getting worse rather than better, particularly if one considers indoor air quality as well as outdoor. (Indoor air quality has become significantly worse since building codes changed in the [[1970s]] to make buildings more air-tight to conserve energy. This affects buildings built since that time.) Adverse reactions to toxins vary considerably from one person to another, and can involve extremes in symptoms including the [[nervous system|neurological]] and [[endocrine system]]s as well as the more commonly recognized allergy symptoms listed above. | Another theory is the exponential use and abuse of chemicals in affluent nations since the second world war. Vast numbers of chemicals are introduced into our indoor and outdoor environments with little or no testing regarding their toxicity to living beings. Many believe that air quality is getting worse rather than better, particularly if one considers indoor air quality as well as outdoor. (Indoor air quality has become significantly worse since building codes changed in the [[1970s]] to make buildings more air-tight to conserve energy. This affects buildings built since that time.) Adverse reactions to toxins vary considerably from one person to another, and can involve extremes in symptoms including the [[nervous system|neurological]] and [[endocrine system]]s as well as the more commonly recognized allergy symptoms listed above. | ||
| − | In 2004, a joint Swedish-Danish research team | + | In 2004, a joint Swedish-Danish research team found a very strong link between allergies in children and the [[phthalates]] DEHP and BBzP, commonly used in [[polyvinyl chloride|PVC]].<!-- |
| + | —><ref>{{cite journal | author = Bornehag C, Sundell J, Weschler C, Sigsgaard T, Lundgren B, Hasselgren M, Hägerhed-Engman L | title = The association between asthma and allergic symptoms in children and phthalates in house dust: a nested case-control study. | journal = Environ Health Perspect | volume = 112 | issue = 14 | pages = 1393-7 | year = 2004 | id = PMID 15471731 | url=http://ehp.niehs.nih.gov/members/2004/7187/7187.html}}</ref> | ||
| − | Allergies are also viewed by some medical practitioners as a negative consequence of the use and abuse of [[antibiotics]] and [[vaccination]]s. This mainstream Western approach to treatment and prevention of infectious disease has been used in the more affluent world for a longer period of time than in the rest of the world, hence the much greater commonality of allergies there. It is hypothesized that use of antibiotics and vaccination affect the [[immune system]], and that allergies are a dysfunctional immune response | + | Allergies are also viewed by some medical practitioners as a negative consequence of the use and abuse of [[antibiotics]] and [[vaccination]]s. This mainstream Western approach to treatment and prevention of infectious disease has been used in the more affluent world for a longer period of time than in the rest of the world, hence the much greater commonality of allergies there. It is hypothesized that use of antibiotics and vaccination affect the [[immune system]], and that allergies are a dysfunctional immune response. |
==Common allergens== | ==Common allergens== | ||
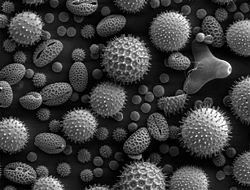
[[Image:Misc pollen.jpg|thumb|250px|right|[[Scanning electron microscope|SEM]] of miscellaneous plant pollens. Pollens are very common allergens.]] | [[Image:Misc pollen.jpg|thumb|250px|right|[[Scanning electron microscope|SEM]] of miscellaneous plant pollens. Pollens are very common allergens.]] | ||
| − | [[Image:House Dust Mite.jpg|thumb|250px|right|The house [[dust mite]] | + | [[Image:House Dust Mite.jpg|thumb|250px|right|The house [[dust mite]]; its feces and [[chitin]] are common allergens around the home]] |
In addition to foreign proteins found in foreign serum (from [[blood transfusion]]s) and [[vaccine]]s, common allergens include: | In addition to foreign proteins found in foreign serum (from [[blood transfusion]]s) and [[vaccine]]s, common allergens include: | ||
| − | *[[Plant]] [[pollen]]s ([[Hay fever]]) | + | *[[Plant]] [[pollen]]s ([[Hay fever]]): |
| − | **[[Ryegrass | rye grass]] | + | **[[Ryegrass|rye grass]] |
**[[ragweed]] | **[[ragweed]] | ||
| − | **[[timothy-grass | timothy grass]] | + | **[[timothy-grass|timothy grass]] |
**[[birch]] trees | **[[birch]] trees | ||
*[[Mold]] [[spore]]s | *[[Mold]] [[spore]]s | ||
| − | *[[Medication|Drugs]] | + | *[[Medication|Drugs]]: |
**[[penicillin]]s | **[[penicillin]]s | ||
**[[sulfonamides]] | **[[sulfonamides]] | ||
**[[salicylate]]s (also found naturally in numerous [[fruit]]s) | **[[salicylate]]s (also found naturally in numerous [[fruit]]s) | ||
**[[local anaesthetic]]s | **[[local anaesthetic]]s | ||
| − | * Foods ([[food allergy]]) | + | * Foods ([[food allergy]]): |
| − | **[[nut (fruit)|nut]]s | + | **[[nut (fruit)|nut]]s (2 separate cases) |
| + | ***[[peanut]]s | ||
| + | ***[[Nut (fruit)|nut]]s | ||
**[[sesame]] | **[[sesame]] | ||
**[[seafood]] | **[[seafood]] | ||
| Line 119: | Line 120: | ||
**[[wheat]] | **[[wheat]] | ||
**[[maize|corn]] or [[maize]] | **[[maize|corn]] or [[maize]] | ||
| − | *[[Insect]] stings | + | *[[Insect]] stings: |
**[[bee]] sting [[venom (poison)|venom]] | **[[bee]] sting [[venom (poison)|venom]] | ||
**[[wasp]] sting venom | **[[wasp]] sting venom | ||
| − | * Animal products (animal allergy) | + | * Animal products (animal allergy): |
**[[fur|Animal hair]] and [[dander]] | **[[fur|Animal hair]] and [[dander]] | ||
**[[cockroach]] calyx | **[[cockroach]] calyx | ||
**[[dust mite]] excretion | **[[dust mite]] excretion | ||
| + | * Other | ||
| + | **[[Latex]] | ||
== See also == | == See also == | ||
| + | * [[Allergic Inflammation|Allergic inflammation]] | ||
| + | * [[Anaphylaxis]] | ||
* [[Atopy]] | * [[Atopy]] | ||
| − | |||
| − | |||
* [[Food allergy]] | * [[Food allergy]] | ||
| + | * [[Hay fever]] | ||
* [[Hypoallergenic]] | * [[Hypoallergenic]] | ||
| − | * [[ | + | * [[Multiple chemical sensitivity]] (MCS). |
* [[Soy allergy]] | * [[Soy allergy]] | ||
| − | |||
==References== | ==References== | ||
| + | |||
| + | <references/> | ||
* Goldsby RA, Kindt TK, Osborne BA and Kuby J (2003) '''Immunology''', 5th Edition, W.H. Freeman and Company, New York, New York, ISBN 0-7167-4947-5 | * Goldsby RA, Kindt TK, Osborne BA and Kuby J (2003) '''Immunology''', 5th Edition, W.H. Freeman and Company, New York, New York, ISBN 0-7167-4947-5 | ||
* Bornehag CG, Sundell J, Weschler CJ, Sigsgaard T, Lundgren B, Hasselgren M, Hagerhed-Engman L. '''The association between asthma and allergic symptoms in children and phthalates in house dust: a nested case-control study.''' Environ Health Perspect 2004;112:1393-7. [http://ehp.niehs.nih.gov/members/2004/7187/7187.html Fulltext]. PMID 15471731. | * Bornehag CG, Sundell J, Weschler CJ, Sigsgaard T, Lundgren B, Hasselgren M, Hagerhed-Engman L. '''The association between asthma and allergic symptoms in children and phthalates in house dust: a nested case-control study.''' Environ Health Perspect 2004;112:1393-7. [http://ehp.niehs.nih.gov/members/2004/7187/7187.html Fulltext]. PMID 15471731. | ||
| Line 144: | Line 149: | ||
==External links== | ==External links== | ||
* [http://www.aaaai.org American Academy of Allergy, Asthma & Immunology] | * [http://www.aaaai.org American Academy of Allergy, Asthma & Immunology] | ||
| − | * [http://www. | + | * [http://www.aafa.org Asthma and Allergy Foundation of America] – patient advocacy organization |
* [http://www.atsdr.cdc.gov/HEC/CSEM/asthma/ Case Studies in Environmental Medicine (CSEM): Environmental Triggers of Asthma] – Agency for Toxic Substances and Disease Registry, U.S. Department of Health and Human Services. | * [http://www.atsdr.cdc.gov/HEC/CSEM/asthma/ Case Studies in Environmental Medicine (CSEM): Environmental Triggers of Asthma] – Agency for Toxic Substances and Disease Registry, U.S. Department of Health and Human Services. | ||
| − | {{credit| | + | |
| + | {{credit|94489534}} | ||
[[Category:Life sciences]] | [[Category:Life sciences]] | ||
Revision as of 19:04, 15 December 2006
- This article deals specifically with IgE-mediated hypersensitivity. For other types of allergic or hypersensitive reactions see the main article: Hypersensitivity
An allergy can refer to several kinds of immune reactions including Type I hypersensitivity in which the person's body is hypersensitised and develops immunoglobulin E (IgE) a certain type of antibodies to typical proteins. When a person is hypersensitised, these substances are known as allergens. The word allergy derives from the Greek words allos meaning "other" and ergon meaning "work". Type I hypersensitivity is characterised by excessive activation of mast cells and basophils by immunoglobulin E resulting in a systemic inflammatory response that can result in symptoms as benign as a runny nose, to life-threatening anaphylactic shock and death.
Allergy is a very common disorder and more than 50 million Americans suffer from allergic diseases. Allergies are the sixth leading cause of chronic disease in the United States, costing the health care system $18 billion annually.
History
The term and concept of "allergy" was coined by a Viennese pediatrician named Clemens von Pirquet in 1906.[1] He observed that the symptoms of some of his patients might have been a response to outside allergens such as dust, pollen, or certain foods. For a long time all hypersensitivities were thought to stem from the improper action of inflammatory immunoglobulin class IgE, however it soon became clear that several different mechanisms utilizing different effector molecules were responsible for the myriad of disorders previously classified as "allergies". A new four-class (now five) classification scheme was designed by P. G. H. Gell and R. R. A. Coombs. Allergy has since been kept as the name for Type I Hypersensitivity, characterised by classical IgE mediation of effects.
Signs and symptoms
Allergy is characterised by a local or systemic inflammatory response to allergens. Local symptoms are:
- Nose: swelling of the nasal mucosa (allergic rhinitis)
- Eyes: redness and itching of the conjunctiva (allergic conjunctivitis)
- Airways: bronchoconstriction, wheezing and dyspnoea, sometimes outright attacks of asthma
- Ears: feeling of fullness, possibly pain, and impaired hearing due to the lack of eustachian tube drainage.
- Skin: various rashes, such as eczema, hives (urticaria) and contact dermatitis.
- Head: while not as common, headaches are seen in some with environmental or chemical allergies.
Systemic allergic response is also called anaphylaxis. Depending of the rate of severity, it can cause cutaneous reactions, bronchoconstriction, edema, hypotension, coma and even death.
Hay fever is one example of an exceedingly common minor allergy — large percentages of the population suffer from hayfever symptoms in response to airborne pollen. Asthmatics are often allergic to dust mites. Apart from ambient allergens, allergic reactions can be due to medications.
Diagnosis
There are several methods for the diagnosis and assessment of allergies.
Skin test
The typical and most simple method of diagnosis and monitoring of Type I Hypersensitivity is by skin testing, also known as prick testing due to the series of pricks made into the patient's skin. Small amounts of suspected allergens and/or their extracts (pollen, grass, mite proteins, peanut extract, etc.) are introduced to sites on the skin marked with pen or dye (the ink/dye should be carefully selected, lest it cause an allergic response itself). The allergens are either injected intradermally or into small scratchings made into the patient's skin, often with a lancet. Common areas for testing include the inside forearm and back. If the patient is allergic to the substance, then a visible inflammatory reaction will usually occur within 30 minutes. This response will range from slight reddening of the skin to full-blown hives in extremely sensitive patients.
After performing the skin test and receiving results, the doctor may apply a steroid cream to the test area to reduce discomfort (such as itching and inflammation).
Problems with skin test
While the skin test is probably the most preferred means of testing because of its simplicity and economics, it is not without complications. Some people may display a delayed-type hypersensitivity (DTH) reaction which can occur as far as 6 hours after application of the allergen and last up to 24 hours. This can also cause serious long-lasting tissue damage to the affected area. These types of serious reactions are quite rare.
Additionally, the application of previously unencountered allergens can actually sensitize certain individuals to the allergen, causing the inception of a new allergy in susceptible individuals.
Skins tests also are not always able to pinpoint a patient's specific allergies if the patient has an allergy but does not react to the skin test allergen.
Total IgE count
Another method used to qualify type I hypersensitivity is measuring the amount of serum IgE contained within the patient's serum. This can be determined through the use of radiometric and colormetric immunoassays. Even the levels the amount of IgE specific to certain allergens can be measured through use of the radioallergosorbent test (RAST).
Treatment
There are limited mainstream medical treatments for allergies. Probably the most important factor in rehabilitation is the removal of sources of allergens from the home environment, and avoiding environments in which contact with allergens is likely.
Immunotherapy
Hyposensitization is a form of immunotherapy where the patient is gradually vaccinated against progressively larger doses of the allergen in question. This can either reduce the severity or eliminate hypersensitivity altogether. It relies on the progressive skewing of IgG ("the blocking antibody") production, as opposed to the excessive IgE production seen in hypersensitivity type I cases. Delivery can occur via allergy injection, or sublingual immunotherapy, allergy drops taken under the tongue. Though not commonly offered in the U.S., sublingual immunotherapy is gaining attention internationally and is very common in Europe.
A second form of immunotherapy involves the intravenous injection of monoclonal anti-IgE antibodies. These bind to free and B-cell IgE signalling such sources for destruction. They do not bind to IgE already bound to the Fc receptor on basophils and mast cells as this would stimulate the allergic inflammatory response. The first agent in this class is omalizumab.
An experimental treatment form, enzyme potentiated desensitization, has been tried with some success but is not in widespread use. EPD uses dilutions of allergen and an enzyme, beta-glucuronidase, to which T-regulatory lymphocytes respond by favouring desensitization, or down-regulation, rather than sensitization. EPD is also under development for the treatment of autoimmune diseases.
Chemotherapy
Several antagonistic drugs are used to block the action of allergic mediators, preventing activation of cells and degranulation processes. They include antihistamines, cortisone, epinephrine (adrenalin), theophylline and Cromolyn sodium. These drugs help alleviate the symptoms of allergy but play little role in chronic alleviation of the disorder. They can play an imperative role in the acute recovery of someone suffering from anaphylaxis, which is why those allergic to bee stings, peanuts, nuts, and shellfish often carry an adrenalin needle with them at all times.
Alternative therapies
In alternative medicine, a number of treatment modalities are considered effective by its practitioners in the treatment of allergies, particularly naturopathic, herbal medicine, homeopathy, traditional Chinese medicine and kinesiology. These modalities are frequently offered as treatment for those seeking additional help when mainstream medicine has failed to provide adequate relief from allergy symptoms. However, mainstream physicians maintain that these claims lack a scientific basis and warn that the efficacy of such treatments is only supported by anecdotal evidence.
Pathophysiology
All hypersensitivities result from an aberration somewhere in the normal immune process. The exact cause of such malfunctions is not always apparent, however, and several arguments from genetic-basis, environmental-basis and intermediate proponents exist with varying validity and acceptance.
Acute response
The difference between a type I hypersensitivity reaction against an allergen to the normal humoral response against a foreign body is that plasma cells secrete IgE as opposed to either IgM (against novel antigens) or IgG (against immunized antigens). IgE binds to Fc receptors on the surface of mast cells and basophils, both involved in the acute inflammatory response.
When IgE is first secreted it binds to the Fc receptors on a mast cell or basophil, and such an IgE-coated cell is said to be sensitized to the allergen in question. A later exposure by the same allergen causes reactivation of these IgE, which then signals for the degranulation of the sensitized mast cell or basophil. There is now strong evidence that mast cells and basophils require costimulatory signals for degranulation in vivo, derived from GPCRs such as chemokine receptors. These granules release histamine and other inflammatory chemical mediators (cytokines, interleukins, leukotrienes, and prostaglandins) into the surrounding tissue causing several systemic effects, such as vasodilation, mucous secretion, nerve stimulation and smooth muscle contraction. This results in the previously described symptoms of rhinorrhea, itchiness, dyspnea, and anaphylaxis. Depending on the individual, allergen, and mode of introduction, the symptoms can be system-wide (calliscal anaphylaxis), or localised to particular body systems (for example, asthma to the respiratory system; eczema to the dermis).
Late-phase response
After the chemical mediators of the acute response subside, late phase responses can often occur. This is due to the migration of other leukocytes such as neutrophils, lymphocytes, eosinophils and macrophages to the initial site. The reaction is usually seen 4-6 hours after the original reaction and can last from 1-2 days. Cytokines from mast cells may also play a role in the persitence of long-term effects. Late phase responses seen in asthma are slightly different to those seen in other allergic responses.
Basis of the allergic response
Genetic basis
There is much evidence to support the genetic basis of allergy, as allergic parents are more likely to have allergic children, and their allergies are likely to be stronger than those from non-allergic parents. However some allergies are not consistent along genealogies with parents being allergic to peanuts, but having children allergic to ragweed, or siblings not sharing the same allergens. Ethnicity has also been shown to play a role in some allergies. Interestingly, in regard to asthma, it has been suggested that different genetic loci are responsible for asthma in people of Caucasian, Hispanic, Asian, and African origins. It has also been suggested that there are both general atopy genes and tissue-specific allergy genes that target the allergic response to specific mucosal tissues. Potential disease associated alleles include both coding region variation and SNPs found in gene regulatory elements.
Relationship with parasites
Some recent research has also begun to show that some kinds of common parasites, such as intestinal worms (e.g. hookworms), secrete immunosuppressant chemicals into the gut wall and hence the bloodstream which prevent the body from attacking the parasite. This gives rise to a new slant on the "hygiene hypothesis" — that co-evolution of man and parasites has in the past led to an immune system that only functions correctly in the presence of the parasites. Without them, the immune system becomes unbalanced and oversensitive. Gutworms and similar parasites are present in untreated drinking water in undeveloped countries, and in developed countries until the routine chlorination and purification of drinking water supplies. This also coincides with the time period in which a significant rise in allergies has been observed.[citation needed] So far, there is only sporadic evidence to support this hypothesis — one scientist who suffered from seasonal allergic rhinitis (hayfever) infected himself with gutworms and was immediately 'cured' of his allergy with no other ill effects.[citation needed] Full clinical trials have yet to be performed however. It may be that the term 'parasite' could turn out to be inappropriate, and in fact a hitherto unsuspected symbiosis is at work.[citation needed]
Basis of increasing prevalence
There has been a notable increase in the commonness of allergies in the past decades, and there are multiple hypotheses explaining this phenomenon. This is in part because we know what they are, in contrast to earlier humans who would think that it is a non-important illness.
The Hygiene Hypothesis
One theory that has been gaining strength is the "hygiene hypothesis". This theory maintains that since children in more affluent countries are leading a cleaner and cleaner life (less exposure to dirt, extra use of disinfectants, etc), their immune systems have less exposure to parasites and other pathogens than children in other countries or in decades past. Their immune systems may, therefore, have many "loaded guns", cells which might have targeted, say, the intestinal worms that no longer cause trouble in affluent neighbourhoods. Having no reasonable target, these cells inadvertently become activated by environmental antigens that might only cause minor reactions in others. It is the symptoms of this exaggerated response that is seen as the allergic reaction.
Many common allergies such as asthma have seen huge increases in the years since the second world war, and many studies appear to show a correlation between this and the increasingly affluent and clean lifestyles in the West. This is supported by studies in less developed countries that do not enjoy western levels of cleanliness, and similarly do not show western levels of incidences of asthma and other allergies. During this same period, air quality, at one time considered the "obvious" cause of asthma, has shown a considerable improvement. This has led some researchers to conclude that it is our "too clean" upbringing that is to blame for the lack of immune system stimulation in early childhood.
So far the evidence to support this theory is limited. One supporting fact is that many Chinese will develop hay fever after moving into USA for three or more years. However, contradictory examples also exist.
Increasing use of chemicals
Another theory is the exponential use and abuse of chemicals in affluent nations since the second world war. Vast numbers of chemicals are introduced into our indoor and outdoor environments with little or no testing regarding their toxicity to living beings. Many believe that air quality is getting worse rather than better, particularly if one considers indoor air quality as well as outdoor. (Indoor air quality has become significantly worse since building codes changed in the 1970s to make buildings more air-tight to conserve energy. This affects buildings built since that time.) Adverse reactions to toxins vary considerably from one person to another, and can involve extremes in symptoms including the neurological and endocrine systems as well as the more commonly recognized allergy symptoms listed above.
In 2004, a joint Swedish-Danish research team found a very strong link between allergies in children and the phthalates DEHP and BBzP, commonly used in PVC.[2]
Allergies are also viewed by some medical practitioners as a negative consequence of the use and abuse of antibiotics and vaccinations. This mainstream Western approach to treatment and prevention of infectious disease has been used in the more affluent world for a longer period of time than in the rest of the world, hence the much greater commonality of allergies there. It is hypothesized that use of antibiotics and vaccination affect the immune system, and that allergies are a dysfunctional immune response.
Common allergens

In addition to foreign proteins found in foreign serum (from blood transfusions) and vaccines, common allergens include:
- Plant pollens (Hay fever):
- Mold spores
- Drugs:
- penicillins
- sulfonamides
- salicylates (also found naturally in numerous fruits)
- local anaesthetics
- Foods (food allergy):
- Insect stings:
- Animal products (animal allergy):
- Animal hair and dander
- cockroach calyx
- dust mite excretion
- Other
- Latex
See also
- Allergic inflammation
- Anaphylaxis
- Atopy
- Food allergy
- Hay fever
- Hypoallergenic
- Multiple chemical sensitivity (MCS).
- Soy allergy
ReferencesISBN links support NWE through referral fees
- ↑ Clemens Peter Pirquet von Cesenatico Template:WhoNamedIt
- ↑ Bornehag C, Sundell J, Weschler C, Sigsgaard T, Lundgren B, Hasselgren M, Hägerhed-Engman L (2004). The association between asthma and allergic symptoms in children and phthalates in house dust: a nested case-control study.. Environ Health Perspect 112 (14): 1393-7. PMID 15471731.
- Goldsby RA, Kindt TK, Osborne BA and Kuby J (2003) Immunology, 5th Edition, W.H. Freeman and Company, New York, New York, ISBN 0-7167-4947-5
- Bornehag CG, Sundell J, Weschler CJ, Sigsgaard T, Lundgren B, Hasselgren M, Hagerhed-Engman L. The association between asthma and allergic symptoms in children and phthalates in house dust: a nested case-control study. Environ Health Perspect 2004;112:1393-7. Fulltext. PMID 15471731.
- Ono SJ. Molecular genetics of allergic diseases. Annu Rev Immunol. 2000;18:347-66. Review. PMID: 10837062
External links
- American Academy of Allergy, Asthma & Immunology
- Asthma and Allergy Foundation of America – patient advocacy organization
- Case Studies in Environmental Medicine (CSEM): Environmental Triggers of Asthma – Agency for Toxic Substances and Disease Registry, U.S. Department of Health and Human Services.
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.