Interferon
Interferon (IFN) is any of a class of proteins naturally produced by the cells of the vertebrate immune system (leucocytes, T cells), fibroblasts) in response to challenges by foreign agents (antigens) such as viruses, bacteria, and parasites and their products, as well as in response to tumor cells. Interferons belong to the large class of glycoproteins known as cytokines. A very important defense against viruses, interferons assist the immune response by inhibiting viral replication within other cells of the body; they also can also combat bacterial and parasitic infections, and moderate specific cellular functions, such as inhibit cell division and cell differentiation or foster cell differentiation.
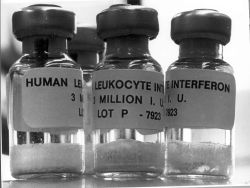
While interferons are naturally produced by the cells of the immune system, they also can be synthetically produced. Mass production of interferons, utilizing recombinant DNA technology, has allowed various interferons to be used for combating such diseases as hepatitis B, hepatitis C, Kaposi's sarcoma, multiple sclerosis, and human papillomavirus.
The interferon system is not only complex and remarkably coordinated with other parts of the immune system, but allows a very rapid response to viral invaders.
Overview
Interferons are glycoproteins. Glycoproteins are proteins that contain oligosaccharide chains (glycans) covalently attached to their polypeptide backbones. Basically, glycoprotein is a biomolecule composed of a protein and a carbohydrate (an oligosaccharide). The carbohydrate is attached to the protein in a cotranslational or posttranslational modification.
Interferons are a related group of glycoproteins that are classified as a type of cytokine. Cytokines are a group of proteins and peptides that are used in organisms as signaling compounds. These chemical signals are similar to hormones and neurotransmitters and are used to allow one cell to communicate with another. The cytokine family consists mainly of smaller water-soluble proteins and glycoproteins (proteins with an added sugar chain) with a mass of between 8 and 30 kDa. While hormones are released from specific organs into the blood and neurotransmitters are released by nerves, cytokines are released by many types of cells. They are particularly important in both innate and adaptive immune responses. Due to their central role in the immune system, cytokines are involved in a variety of immunological, inflammatory, and infectious diseases. However, not all their functions are limited to the immune system, as they are also involved in several developmental processes during embryogenesis.
Interferons are produced by leucocytes, T lymphocytes (T cells), and fibroblasts in response to infection. The body utilizes interferons to activate specific T cells to destroy invaders, such as viruses. T cells are lymphocytes (a class of white blood cells) that play a central role in the adaptive immune system, and specifically in the cell-mediated immune system. The cell-mediated immune system involves intricate pathways to produce and activate T cells, such that the T cells produced are specific in mobilizing against a particular threat to the body, including microorganisms and infected cells. Interferons do not attack invaders themselves, but activate specific T cells to help defeat foreign cells.
When the immune system is fighting pathogens, interferons signal immune cells, such as T-cells and macrophages, to travel to the site of infection. In addition, interferons activate those cells, stimulating them to produce more interferons.
Types of interferons
There are many different types of interferons, listed as alpha, beta, gamma, tau, omega, and so forth. Furthermore, these can be placed in classes (I, II, III) according to the receptor they bind. For example, the fibroblast or beta interferon (IFN-ÎČ) and the leukocyte or alpha family of interferons (IFN-α) are placed together as two major subtypes in type I IFNs. The only known interferon of type II is IFN-Îł, which is produced exclusively by lymphocytes.
There are three major classes of interferons that have been described for humans according to the type of receptor through which they signal:
- Interferon type I. All type I IFNs bind to a specific cell surface receptor complex known as the IFN-α receptor (IFNAR) that consists of IFNAR1 and IFNAR2 chains. Homologous molecules to type I IFNs are found in many species, including most mammals, and some have been identified in birds, reptiles, amphibians, and fish species.[1] In humans, the types are designated IFN-α (alpha), IFN-ÎČ (beta), IFN-Îș (kappa), IFN-ÎŽ (delta), IFN-Δ (epsilon), IFN-Ï (tau), IFN-Ï (omega) and IFN-ζ (zeta, also known as limitin).[2] There are also subtypes of even these, such as The IFN-α proteins come in 13 subtypes such as IFNA1, IFNA2, and so forth. These genes for these IFN-α molecules are found together in a cluster on chromosome 9.
- Interferon type II. A sole member makes up interferon type II and is called IFN-Îł (gamma). Mature IFN-Îł is an anti-parallel homodimer, which binds to the IFN-Îł receptor (IFNGR) complex to elicit a signal within its target cell. IFNGR is made up of two subunits each of molecules designated IFNGR1 and IFNGR2. IFN-Îł is involved in the regulation of the immune and inflammatory responses; in humans, there is only one type of interferon-gamma. It is produced in activated T-cells and natural killer cells. IFN-Îł has some anti-viral and anti-tumor effects, but these are generally weak. However, this cytokine potentiates the effects of the type I IFNs. IFN-Îł released by Th1 cells recruits leukocytes to a site of infection, resulting in increased inflammation. It also stimulates macrophages to kill bacteria that have been engulfed.
- Interferon type III. The recently classified type Interferon type III group consists of three IFN-λ (lambda) molecules called IFN-λ1, IFN-λ2 and IFN-λ3 (also called IL29, IL28A, and IL28B respectively).[3] These IFNs signal through a receptor complex consisting of IL10R2 (also called CRF2-4) and IFNLR1 (also called CRF2-12).[4]
History
While aiming to develop an improved vaccine for smallpox, two Japanese virologists, Yasu-ichi Nagano and Yasuhiko Kojima, working at the the Institute for Infectious Diseases at the University of Tokyo, noticed that rabbit-skin or testis previously inoculated with UV-inactivated virus exhibited inhibition of viral growth when re-infected at the same site with live virus. They hypothesized that this was due to some inhibitory factor, and began to characterize it by fractionation of the UV-irradiated viral homogenates using an ultracentrifuge. They published these findings in 1954, in the French journal now known as âJournal de la SociĂ©tĂ© de Biologie.â[5]
While these findings demonstrated that the activity could be separated from the virus particles, it could not reconcile the antiviral activity, demonstrated in the rabbit skin experiments, with the observation that the same supernatant led to the production of antiviral antibodies in mice. A further paper in 1958, involving triple-ultracentrifugation of the homogenate, demonstrated that the inhibitory factor was distinct from the virus particles, leading to trace contamination being ascribed to the 1954 observations.[6]
Meanwhile, the British virologist Alick Isaacs and the Swiss researcher Jean Lindenmann, at the National Institute for Medical Research in London, noticed an interference effect caused by heat-inactivated influenza virus on the growth of live influenza virus in chicken egg membranes in a nutritive solution chorioallantoic membrane. They published their results in 1957;[7] in this paper, they coined the term "interferon," and today that specific interfering agent is known as a "Type I interferon."
Naganoâs work was never fully appreciated in the scientific community, possibly because it was printed in French, but also because his in vivo system was perhaps too complex to provide clear results in the characterization and purification of interferon. As time passed, Nagano became aware that his work had not been widely recognized, yet did not actively seek revaluation of his status in field of interferon research. As such, the majority of the credit for discovery of the interferon goes to Isaacs and Lindenmann.[8]
Interferon was scarce and expensive until 1980 when the interferon gene was inserted into bacteria using recombinant DNA technology, allowing mass cultivation and purification from bacterial cultures.[9] Recombinant DNA technology has provide a large supply of interferons for treatment of disease and for research into its therapeutic properties.
Natural function and synthesis
Interferons in general have several effects in common. They are antiviral and possess antioncogenic properties, macrophage and natural killer lymphocyte activation, and enhancement of major histocompatibility complex glycoprotein classes I and II, and thus presentation of foreign (microbial) peptides to T cells.
In a majority of cases, the production of interferons is induced in response to microbes such as viruses and bacteria and their products (viral glycoproteins, viral RNA, bacterial endotoxin, bacterial flagella, CpG sites), as well as mitogens and other cytokines, for example interleukin 1, interleukin 2, interleukin-12, tumor necrosis factor, and colony-stimulating factor, which are synthesized in the response to the appearance of various antigens in the body. Their metabolism and excretion take place mainly in the liver and kidneys. They rarely pass the placenta, but they can cross the blood-brain barrier.
Viral induction of interferons
All classes of interferon are very important in fighting RNA virus infections. However, their presence also accounts for some of the host symptoms, such as sore muscles and fever. Interferons are secreted when abnormally large amounts of dsRNA are found in a cell. dsRNA is normally present in very low quantities. The dsRNA acts like a trigger for the production of interferon (via Toll Like Receptor 3 (TLR 3) a pattern recognition receptor of the innate immune system, which leads to activation of the transcription factor IRF3 and late phase NF kappa Beta). The gene that codes for this cytokine is switched on in an infected cell, and the interferon synthesized and secreted to surrounding cells.
As the original cell dies from the cytolytic RNA virus, these thousands of viruses will infect nearby cells. However, these cells have received interferon, which essentially warns these other cells that there's a wolf in the pack of sheep. They then start producing large amounts of a protein known as protein kinase R (or PKR). If a virus infects a cell that has been âpre-warnedâ by interferon, it is like charging into a hail of bullets for the virus. The PKR is indirectly activated by the dsRNA (actually by 2'-5' oligoadenylate produced by the 2'-5' oligoadenylate-synthetase which is produced due to TLR3 activation), and begins transferring phosphate groups (phosphorylating) to a protein known as eIF-2, a eukaryotic translation initiation factor. After phosphorylation, eIF2 has a reduced ability to initiate translation, the production of proteins coded by cellular mRNA. This prevents viral replication and inhibits normal cell ribosome function, killing both the virus and the host cell if the response is active for a sufficient amount of time. All RNA within the cell is also degraded, preventing the mRNA from being translated by eIF2 if some of the eIF2 failed to be phosphorylated.
Furthermore, interferon leads to upregulation of MHC I and therefore to increased presentation of viral peptides to cytotoxic CD8 T cells, as well as to a change in the proteasome (exchange of some beta subunits by b1i, b2i, b5iâthen known as the immunoproteasome), which leads to increased production of MHC I compatible peptides.
Interferon can cause increased p53 activity in virus-infected cells. It acts as an inducer and causes increased production of the p53 gene product. This promotes apoptosis, limiting the ability of the virus to spread. Increased levels of transcription are observed even in cells that are not infected, but only infected cells show increased apoptosis. This increased transcription may serve to prepare susceptible cells so they can respond quickly in the case of infection. When p53 is induced by viral presence, it behaves differently than it usually does. Some p53 target genes are expressed under viral load, but others, especially those that respond to DNA damage, are not. One of the genes that is not activated is p21, which can promote cell survival. Leaving this gene inactive would help promote the apoptotic effect. Interferon enhances the apoptotic effects of p53, but it is not strictly required. Normal cells exhibit a stronger apoptotic response than cells without p53.[10]
Additionally, interferons have been shown to have therapeutic effect against certain cancers. It is probable that one mechanism of this effect is p53 induction. This could be useful clinically: Interferons could supplement or replace chemotherapy drugs that activate p53 but also cause unwanted side effects. Some of these side effects can be serious, severe, and permanent.
Virus resistance to interferons
In a study of the blocking of interferon (IFN) by the Japanese Encephalitis Virus (JEV), a group of researchers infected human recombinant IFN-alpha with JEV, DEN-2, and PL406, which are all viruses, and found that some viruses have manifested methods that give them a way around the IFN-alpha/beta response. By mastering these methods, the viruses have the ability to carry on viral replication and production of new viruses.[11] The ways that viruses find a way around the IFN response is through the inhibition of interferon signaling, production, and the blocking of the functions of IFN-induced proteins.
It is not unusual to find viruses encoding for a multiple number of mechanisms to allow them to elude the IFN response at many different levels. While doing the study with JEV, Lin and his coworkers found that with IFN-alpha's inability to block JEV means that JEV may be able to block IFN-alpha signaling which in turn would prevent IFN from having STAT1, STAT2, ISGF3, and IRF-9 signaling. DEN-2 also significantly reduces interferon ability to active JAK-STAT. Some other viral gene products that have been found to have an effect on IFN signaling include EBNA-2, polyomavirus large T antigen, EBV EBNA1, HPV E7, HCMV, and HHV8.[12] "Several poxviruses encode a soluble IFN receptor homologue that acts as a decoy to inhibit the biological activity of IFN," and that activity is for IFN to "bind to their cognate receptors on the cell surface to initiate a signaling cascade, known as the Janus kinase(JAK)-signal transducer and activation of transcription(Stat) pathways." For example, in a study done by a groups of researchers, they found that the B18R protein, which acts as a type 1 IFN receptor and is produced by the vaccinia virus, it was found that the B18R protein inhibited IFN's ability to begin the phosphorylation of JAK1, which reduced the antiviral effect of IFN.[13]
Some viruses can encode proteins that bind to dsRNA. In a study where the researchers infected human U cells with reovirus-sigma3 protein and then, utilized the Western blot test, they found that reaovirus-sigma3 protein does bind to dsRNA.[14] Along with that, another study in which the researchers infected mouse L cells with vaccinia virus E3L found that E3L encodes the p25 protein that binds to dsRNA.[15] Without double stranded RNA (dsRNA), because it is bound to by the proteins, it is not able to create IFN-induced PKR and 2'-5' oligoadenylate-synthetase making IFN ineffective.[16] It was also found that JEV was able to inhibit IFN-alpha's ability to activate or create ISGs such as PKR. PKR was not able to be found in the JEV infected cells and PKR RNA levels were found to be lower in those same infected cells, and this disruption of PKR can occur, for example, in cells infected with flavaviruses.
The H5N1 influenza virus, also known as bird flu, has been shown to have resistance to interferon and other anti-viral cytokines. This is part of the reason for its high mortality rates in humans. It is resistant due to a single amino acid mutation in non-structural protein 1 (NS1). The precise mechanism of how this confers immunity is unclear.
Pharmaceutical uses
Uses
Just as their natural function, interferons have antiviral, antiseptic, and antioncogenic properties when administered as drugs. Alpha interferons are used to treat such cancers as hairy cell leukemia, Kaposi's sarcoma, and malignant melanoma, among others, and are commercially produced and sold under various brand names. Interferon therapy is used (in combination with chemotherapy and radiation) as a treatment for many cancers.
More than half of hepatitis C patients treated with interferon respond with better blood tests and better liver biopsies. There is some evidence that giving interferon immediately following infection can prevent hepatitis C; however, people infected by hepatitis C often do not display symptoms of HCV until months or years later.
Interferon is also used in the treatment and control of the neurological disorder multiple sclerosis, an autoimmune disorder. Interferon-beta (Interferon beta-1a and Interferon beta-1b) is used in the treatment and control of multiple sclerosis. For example, Betaseron (interferon beta-1b) is approved for use by people with MS. By an as-yet-unknown mechanism, interferon-beta inhibits the production of Th1 cytokines and the activation of monocytes.
Administered intranasally in very low doses, interferon is extensively used in Eastern Europe and Russia as a method to prevent and treat viral respiratory diseases such as cold and flu. However, mechanisms of such action of interferon are not well understood; it is thought that doses must be larger by several orders of magnitude to have any effect on the virus. Consequently, most Western scientists are skeptical of any claims of good efficacy.
Route of administration
When used in the systemic therapy, IFN-α and IFN-γ are mostly administered by an intramuscular injection. The injection of interferons in the muscle, in the vein, or under skin is generally well tolerated.
Interferon alpha can also be induced with small imidazoquinoline molecules by activation of TLR7 receptor. Aldara (Imiquimod) cream works with this mechanism to induce IFN alpha and IL12 and approved by FDA to treat Actinic Keratosis, Superficial Basal Cell Carcinoma, and External Genital Warts.
Adverse effects
The most frequent adverse effects are flu-like symptoms: Increased body temperature, feeling ill, fatigue, headache, muscle pain, convulsion, dizziness, hair thinning, and depression. Erythema, pain and hardness on the spot of injection are also frequently observed. Interferon therapy causes immunosuppression and can result in some infections manifesting in unusual ways.[17]
All known adverse effects are usually reversible and disappear a few days after the therapy has been finished.
Pharmaceutical forms of interferons in the market
- Rebif, liquid form of Interferon beta 1a
- Avonex, lyophilized form of Interferon beta 1a
- Cinnovex, generic/biosimilar form of Interferon beta 1a (Avonex)
- Betaseron, Interferon beta 1b
- Roferon A. regular Interferon-alpha2a
- Intron-A, regular Interferon-alpha2b
- PEGASYS, Pegylated Interferon alpha 2a
- Berlex, Interferon beta 1b
- PegIntron, Pegylated Interferon alpha 2b
- Reiferon Etard , pegylated Interferon alpha 2a
Notes
- â U. Schultz, B. Kaspers, and P. Staeheli, "The interferon system of non-mammalian vertebrates," Developmental and Comparative Immunology 28(2004): 499-508.
- â Oritani and Tomiyama, "Interferon-ζ/limitin: Novel type I Interferon that displays a narrow range of biological activity," International Journal of Hematology 80(2004): 325-331.
- â Vilcek, "Novel interferons, "Nature Immunology 4(2003): 8-9.
- â Bartlett et al., "Murine interferon lambdas (type III interferons) exhibit potent antiviral activity in vivo in a poxvirus infection model," Journal of General Virology 86(2005): 1589â1596.
- â Y. Nagano and Y. Kojima, "Pouvoir immunisant du virus vaccinal inactivĂ© par des rayons ultraviolets," C.R. Seances Soc. Biol. Fil. 148(1954): 1700-1702.
- â Y. Nagano and Y. Kojima, "Inhibition de l'infection vaccinale par un facteur liquide dans le tissu infectĂ© par le virus homologue," C.R. Seances Soc. Biol. Fil. 152(1958): 1627-1629.
- â A. Isaacs and J. Lindenmann, "Virus interference. I. The interferon," Proc. Roy. Soc. Lond. B Biol. Sci. 147(1957): 258-267.
- â Derek Burke, The Discovery of Interferon, the First Cytokine, by Alick Isaacs and Jean Lindenmann in 1957 Brain Immune Trends, February 14, 2009. Retrieved June 19, 2018.
- â S. Nagata, H. Taira, A. Hall, L. Johnstrud, et al., "Synthesis in E. coli of a polypeptide with human leukocyte interferon activity." Nature (London) 284 (1980): 315-321.
- â A. Takaoka, S. Hayakawa, H. Yanai, et al., Integration of interferon-alpha/beta signalling to p53 responses in tumour suppression and antiviral defense, Nature 424(2003)(6948): 516-523. Retrieved June 19, 2018.
- â R.J. Lin, C.L. Liao, E. Lin, and Y.L. Lin, "Blocking of the alpha interferon-induced Jak-Stat signaling pathway by Japanese encephalitis virus infection," J. Virol. 78(2004)(17): 9285-9294.
- â G.C. Sen, "Viruses and interferons," Annual Review Microbiology 55 (2003): 255-281.
- â A. Alcami', et al., "The vaccinia virus soluble alpha/beta interferon (IFN) receptor binds to the cell surface and protects cells from the antiviral effects of IFN," Journal of Virology (September 2000): 11230-11239.
- â J.E. Miller and C.E. Samuel, "Proteolytic cleavage of the reovirus sigma 3 protein results in enhanced double-stranded RNA-binding activity: Identification of a repeated basic amino acid motif within the C-terminal binding region," Journal of Virology 66(1992)(9): 5347-5356.
- â H. Chang, et al., "The E3L gene of vaccinia virus encodes an inhibitor of the interferon-induced, double-stranded RNA-dependent protein kinase," Proceedings of the National Academy of Sciences 89(1992): 4825-4829.
- â M.A. Minks, et al., "Structural requirements of double-stranded RNA for the activation of 2',5'-oligo(A) polymerase and protein kinase of interferon-treated HeLa cells," The Journal of Biological Chemistry 254(1979)(20): 10180-10183.
- â Z. Bhatti and C. S. Berenson, "Adult systemic cat scratch disease associated with therapy for hepatitis C," BMC Infect Dis 7(2007): 8.
ReferencesISBN links support NWE through referral fees
- Cantell, Kari. The Story of Interferon: The Ups and Downs in the Life of a Scientist. World Scientific Pub. Co. Inc., 1998. ISBN 978-9810231484
- Edelhart, Michael. Interferon: The New Hope for Cancer. Addison-Wesley, 1981. ISBN 978-0201039436
- Pieters, Toine. Interferon: The Science and Selling of a Miracle Drug. Routledge2, 2012. ISBN 978-0415648660
- Thomas, Joe H., and Adrian Roberts (eds.). Interferons: Characterization, Mechanism of Action and Clinical Applications. Nova Biomedical, 2012. ISBN 978-1620812983
External links
All links retrieved November 30, 2024.
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
- Interferon history
- Cytokine history
- Glycoprotein history
- Interferon_type_IIÂ history
- Interferon_type_IÂ history
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.