Difference between revisions of "Mental disorder" - New World Encyclopedia
| Line 62: | Line 62: | ||
===Nineteenth century=== | ===Nineteenth century=== | ||
| − | Industrialization and population growth led to a massive expansion of the number and size of insane asylums in every Western country in the | + | [[Industrialization]] and population growth led to a massive expansion of the number and size of insane asylums in every Western country in the nineteenth century. Numerous different classification schemes and diagnostic terms were developed by different authorities. The term [[psychiatry]] was coined in 1808, though medical superintendents were still known as "alienists." |
===Twentieth century=== | ===Twentieth century=== | ||
Revision as of 22:32, 2 June 2021
Currently working on —Jennifer Tanabe March 2021.
| Mental disorder | |
| |
| Other names | Psychiatric disorder, psychological disorder, mental illness, mental disease, mental breakdown, nervous breakdown, mental health conditions[1] |
|---|---|
| Symptoms | Agitation, anxiety, depression, mania, paranoia, psychosis |
| Complications | Cognitive impairment, social problems, suicide |
| Types | Anxiety disorders, eating disorders, mood disorders, personality disorders, psychotic disorders, substance use disorders |
| Causes | Genetic and environmental factors |
| Treatment | Psychotherapy, medications |
| Medication | Antidepressants, antipsychotics, anxiolytics, mood stabilizers, stimulants |
A mental disorder, also called a mental illness or psychiatric disorder, is a behavioral or mental pattern that causes significant distress or impairment of personal functioning. Such features may be persistent, relapsing and remitting, or occur as a single episode. Many disorders have been described, with signs and symptoms that vary widely between specific disorders. Such disorders may be diagnosed by a mental health professional.
The causes of mental disorders are often unclear. Theories may incorporate findings from a range of fields. Mental disorders are usually defined by a combination of how a person behaves, feels, perceives, or thinks. This may be associated with particular regions or functions of the brain, often in a social context. A mental disorder is one aspect of mental health. Cultural and religious beliefs, as well as social norms, should be taken into account when making a diagnosis.
Services are based in psychiatric hospitals or in the community, and assessments are carried out by mental health professionals such as psychiatrists, psychologists, psychiatric nurses and clinical social workers, using various methods such as psychometric tests but often relying on observation and questioning. Treatments are provided by various mental health professionals. Psychotherapy and psychiatric medication are two major treatment options. Other treatments include lifestyle changes, social interventions, peer support, and self-help. In a minority of cases, there might be involuntary detention or treatment. Prevention programs have been shown to reduce depression.
Definition
A mental disorder (mental illness or psychiatric disorder) is a behavioral or mental pattern that causes significant distress or impairment of personal functioning.[2] Such features may be persistent, relapsing and remitting, or occur as a single episode. For a mental state to classify as a disorder, it generally needs to cause dysfunction.[3] Such disorders may be diagnosed by a mental health professional.
According to the Diagnostic and Statistical Manual of Mental Disorders DSM-IV edition, a mental disorder was defined as psychological syndrome or pattern which is associated with distress (e.g. via a painful symptom), disability (impairment in one or more important areas of functioning), increased risk of death, or causes a significant loss of autonomy. In 2013, the American Psychiatric Association (APA) redefined mental disorders in the DSM-5 as "a syndrome characterized by clinically significant disturbance in an individual's cognition, emotion regulation, or behavior that reflects a dysfunction in the psychological, biological, or developmental processes underlying mental functioning."[4] The final draft of ICD-11 contains a very similar definition.[5]
The terms "mental breakdown" or "nervous breakdown" have not been formally defined through a medical diagnostic system. However, they are often used by the general population to mean a mental disorder.[6] Although "nervous breakdown" is not rigorously defined, surveys of laypersons suggest that the term refers to a specific acute time-limited reactive disorder, involving symptoms such as anxiety or depression, usually precipitated by external stressors.[7] Many health experts today refer to a nervous breakdown as a "mental-health crisis."[8]
History
Historically, mental disorders have had three major explanations: the supernatural, biological, and psychological.[9] For much of recorded history, deviant behavior has been considered supernatural and a reflection of the battle between good and evil. When confronted with unexplainable, irrational behavior, people have perceived evil. In fact, in the Persian Empire from 550 to 330 B.C.E., all physical and mental disorders were considered the work of the devil.[9]
Physical causes of mental disorders have been sought in history. Hippocrates was important in this tradition as he identified syphilis as a disease and was therefore an early proponent of the idea that psychological disorders are biologically caused.[9] This was a precursor to modern psycho-social treatment approaches to the causation of psychopathology, with the focus on psychological, social, and cultural factors. Well known philosophers like Plato, Aristotle, and others, wrote about the importance of fantasies and dreams, and thus anticipated, to some extent, the fields of psychoanalytic thought and cognitive science. They were also some of the first to advocate for humane and responsible care for individuals with psychological disturbances.[9]
Ancient civilizations
Ancient civilizations described and treated a number of mental disorders. Mental illnesses were well known in ancient Mesopotamia, the royal family of Elam being notorious for its members frequently suffering from insanity, and Mesopotamian doctors kept detailed record of their patients' hallucinations and assigned spiritual meanings to them.[10] Diseases and mental disorders were believed to be caused by specific deities.[11] Because hands symbolized control over a person, mental illnesses were known as "hands" of certain deities. One psychological illness was known as Qāt Ištar, meaning "Hand of Ishtar," while others were known as "Hand of Shamash," "Hand of the Ghost," and "Hand of the God."[11] Descriptions of these illnesses, however, are so vague that it is usually impossible to determine which illnesses they correspond to in modern terminology.
The Greeks coined terms for melancholy, hysteria and phobia and developed the humorism theory. Mental disorders were described, and treatments developed, in Persia, Arabia and in the medieval Islamic world.
Middle Ages
Conceptions of madness in the Middle Ages in Christian Europe were a mixture of the divine, diabolical, magical, and humoral and transcendental.[12] Some people with mental disorders may have been victims of the witch-hunts. While not every witch and sorcerer accused were mentally ill, all mentally ill were considered to be witches or sorcerers.[13]
Eighteenth century
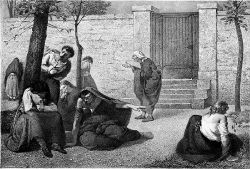
By the end of the seventeenth century and into the Age of Enlightenment, madness was increasingly seen as an organic physical phenomenon with no connection to the soul or moral responsibility. Asylum care was often harsh and treated people like wild animals, but towards the end of the eighteenth century a moral treatment movement gradually developed.
Nineteenth century
Industrialization and population growth led to a massive expansion of the number and size of insane asylums in every Western country in the nineteenth century. Numerous different classification schemes and diagnostic terms were developed by different authorities. The term psychiatry was coined in 1808, though medical superintendents were still known as "alienists."
Twentieth century
The turn of the twentieth century saw the development of psychoanalysis, which would later come to the fore, along with Kraepelin's classification scheme, the most significant aspect of which is the classification of what was previously considered to be a unitary concept of psychosis into two distinct forms (known as the Kraepelinian dichotomy):
- manic depression (now seen as comprising a range of mood disorders such as recurrent major depression and bipolar disorder), and
- dementia praecox, later renamed schizophrenia
Asylum "inmates" were increasingly referred to as "patients," and asylums renamed as hospitals.
- Deinstitutionalization and transinstitutionalization
When state hospitals were accused of violating human rights, advocates pushed for deinstitutionalization: the replacement of federal mental hospitals for community mental health services. The closure of state-provisioned psychiatric hospitals was enforced by the Community Mental Health Centers Act in 1963 that laid out terms in which only patients who posed an imminent danger to others or themselves could be admitted into state facilities.[14] This was seen as an improvement from previous conditions, however, there remains a debate on the conditions of these community resources. It has been proven that this transition was beneficial for many patients: there was an increase in overall satisfaction, a better quality of life, more friendships between patients, and not too costly. This proved to be true only in the circumstance that treatment facilities that had enough funding for staff and equipment as well as proper management.[15] However, this idea is a polarizing issue. Critics of deinstitutionalization argue that poor living conditions prevailed, patients were lonely, and they did not acquire proper medical care in these treatment homes.[16] Additionally, patients that were moved from state psychiatric care to nursing and residential homes had deficits in crucial aspects of their treatment. Some cases result in the shift of care from health workers to patients’ families, where they do not have the proper funding or medical expertise to give proper care.[16] On the other hand, patients that are treated in community mental health centers lack sufficient cancer testing, vaccinations, or otherwise regular medical check-ups.[16]
Other critics of state deinstitutionalization argue that this was simply a transition to “transinstitutionalization”, or the idea that prisons and state-provisioned hospitals are interdependent. In other words, patients become inmates. This draws on the Penrose Hypothesis of 1939, which theorized that there was an inverse relationship between prisons’ population size and the number of psychiatric hospital beds.[17] This means that populations that require psychiatric mental care will transition between institutions, which in this case, includes state psychiatric hospitals and criminal justice systems. Thus, a decrease in available psychiatric hospital beds occurred at the same time as an increase in inmates.[17] Although some are skeptical that this is due to other external factors, others will reason this conclusion to a lack of empathy for the mentally ill. There is no argument in the social stigmatization of those with mental illnesses, they have been widely marginalized and discriminated against in society.[18] In this source, researchers analyze how most compensation prisoners (detainees who are unable or unwilling to pay a fine for petty crimes) are unemployed, homeless, and with an extraordinarily high degree of mental illnesses and substance abuse.[17] Compensation prisoners then lose prospective job opportunities, face social marginalization, and lack access to resocialization programs, which ultimately facilitate reoffending.[17] The research sheds light on how the mentally ill — and in this case, the poor— are further punished for certain circumstances that are beyond their control, and that this is a vicious cycle that repeats itself. Thus, prisons embody another state-provisioned mental hospital.
Families of patients, advocates, and mental health professionals still call for the increase in more well-structured community facilities and treatment programs with a higher quality of long-term inpatient resources and care. With this more structured environment, the United States will continue with more access to mental health care and an increase in the overall treatment of the mentally ill.
However, there is still a lack of studies for MHCs( mental Health conditions) to raise awareness, knowledge development, and attitude of seeking medical treatment for MHCs in Bangladesh. People in rural areas often seek treatment from the traditional healers and these MHCs sometimes considered as a spiritual matters.[19]
Early in the 20th century in the United States, a mental hygiene movement developed, aiming to prevent mental disorders. Clinical psychology and social work developed as professions. World War I saw a massive increase of conditions that came to be termed "shell shock".
World War II saw the development in the U.S. of a new psychiatric manual for categorizing mental disorders, which along with existing systems for collecting census and hospital statistics led to the first Diagnostic and Statistical Manual of Mental Disorders (DSM). The International Classification of Diseases (ICD) also developed a section on mental disorders. The term stress, having emerged from endocrinology work in the 1930s, was increasingly applied to mental disorders.
Electroconvulsive therapy, insulin shock therapy, lobotomies and the "neuroleptic" chlorpromazine came to be used by mid-century.[20] In the 1960s there were many challenges to the concept of mental illness itself. These challenges came from psychiatrists like Thomas Szasz who argued that mental illness was a myth used to disguise moral conflicts; from sociologists such as Erving Goffman who said that mental illness was merely another example of how society labels and controls non-conformists; from behavioral psychologists who challenged psychiatry's fundamental reliance on unobservable phenomena; and from gay rights activists who criticised the APA's listing of homosexuality as a mental disorder. A study published in Science by Rosenhan received much publicity and was viewed as an attack on the efficacy of psychiatric diagnosis.[21]
Deinstitutionalization gradually occurred in the West, with isolated psychiatric hospitals being closed down in favor of community mental health services. A consumer/survivor movement gained momentum. Other kinds of psychiatric medication gradually came into use, such as "psychic energizers" (later antidepressants) and lithium. Benzodiazepines gained widespread use in the 1970s for anxiety and depression, until dependency problems curtailed their popularity.
Advances in neuroscience, genetics and psychology led to new research agendas. Cognitive behavioral therapy and other psychotherapies developed. The DSM and then ICD adopted new criteria-based classifications, and the number of "official" diagnoses saw a large expansion. Through the 1990s, new SSRI-type antidepressants became some of the most widely prescribed drugs in the world, as later did antipsychotics. Also during the 1990s, a recovery approach developed.
Additionally to the concept of mental disorder, some people have argued for a return to the old-fashioned concept of nervous illness. In How Everyone Became Depressed: The Rise and Fall of the Nervous Breakdown (2013), Edward Shorter, a professor of psychiatry and the history of medicine, says:
About half of them are depressed. Or at least that is the diagnosis that they got when they were put on antidepressants. ... They go to work but they are unhappy and uncomfortable; they are somewhat anxious; they are tired; they have various physical pains—and they tend to obsess about the whole business. There is a term for what they have, and it is a good old-fashioned term that has gone out of use. They have nerves or a nervous illness. It is an illness not just of mind or brain, but a disorder of the entire body. ... We have a package here of five symptoms—mild depression, some anxiety, fatigue, somatic pains, and obsessive thinking. ... We have had nervous illness for centuries. When you are too nervous to function ... it is a nervous breakdown. But that term has vanished from medicine, although not from the way we speak.... The nervous patients of yesteryear are the depressives of today. That is the bad news.... There is a deeper illness that drives depression and the symptoms of mood. We can call this deeper illness something else, or invent a neologism, but we need to get the discussion off depression and onto this deeper disorder in the brain and body. That is the point.
Edward Shorter, Faculty of Medicine, University of Toronto[22]
In eliminating the nervous breakdown, psychiatry has come close to having its own nervous breakdown.
David Healy, MD, FRCPsych, Professor of Psychiatry, University of Cardiff, Wales[23]
Nerves stand at the core of common mental illness, no matter how much we try to forget them.
Peter J. Tyrer, FMedSci, Professor of Community Psychiatry, Imperial College, London[24]
"Nervous breakdown" is a pseudo-medical term to describe a wealth of stress-related feelings and they are often made worse by the belief that there is a real phenomenon called "nervous breakdown".
Richard E. Vatz, co-author of explication of views of Thomas Szasz in "Thomas Szasz: Primary Values and Major Contentions"
Mental health policies
The mental health policies in the United States have experienced four major reforms: the American asylum movement led by Dorothea Dix in 1843; the "mental hygiene" movement inspired by Clifford Beers in 1908; the deinstitutionalization started by Action for Mental Health in 1961; and the community support movement called for by The CMCH Act Amendments of 1975.[25]
In 1843, Dorothea Dix submitted a Memorial to the Legislature of Massachusetts, describing the abusive treatment and horrible conditions received by the mentally ill patients in jails, cages, and almshouses. She revealed in her Memorial: "I proceed, gentlemen, briefly to call your attention to the present state of insane persons confined within this Commonwealth, in cages, closets, cellars, stalls, pens! Chained, naked, beaten with rods, and lashed into obedience...."[26] Many asylums were built in that period, with high fences or walls separating the patients from other community members and strict rules regarding the entrance and exit. In those asylums, traditional treatments were well implemented: drugs were not used as a cure for a disease, but a way to reset equilibrium in a person's body, along with other essential elements such as healthy diets, fresh air, middle class culture, and the visits by their neighboring residents.[citation needed] In 1866, a recommendation came to the New York State Legislature to establish a separate asylum for chronic mentally ill patients. Some hospitals placed the chronic patients into separate wings or wards, or different buildings.[27]
In A Mind That Found Itself (1908) Clifford Whittingham Beers described the humiliating treatment he received and the deplorable conditions in the mental hospital.[28] One year later, the National Committee for Mental Hygiene (NCMH) was founded by a small group of reform-minded scholars and scientists – including Beers himself – which marked the beginning of the "mental hygiene" movement. The movement emphasized the importance of childhood prevention. World War I catalyzed this idea with an additional emphasis on the impact of maladjustment, which convinced the hygienists that prevention was the only practical approach to handle mental health issues.[29] However, prevention was not successful, especially for chronic illness; the condemnable conditions in the hospitals were even more prevalent, especially under the pressure of the increasing number of chronically ill and the influence of the depression.[25]
In 1961, the Joint Commission on Mental Health published a report called Action for Mental Health, whose goal was for community clinic care to take on the burden of prevention and early intervention of the mental illness, therefore to leave space in the hospitals for severe and chronic patients. The court started to rule in favor of the patients' will on whether they should be forced to treatment. By 1977, 650 community mental health centers were built to cover 43 percent of the population and serve 1.9 million individuals a year, and the lengths of treatment decreased from 6 months to only 23 days.[30] However, issues still existed. Due to inflation, especially in the 1970s, the community nursing homes received less money to support the care and treatment provided. Fewer than half of the planned centers were created, and new methods did not fully replace the old approaches to carry out its full capacity of treating power.[30] Besides, the community helping system was not fully established to support the patients' housing, vocational opportunities, income supports, and other benefits.[25] Many patients returned to welfare and criminal justice institutions, and more became homeless. The movement of deinstitutionalization was facing great challenges.[31]
After realizing that simply changing the location of mental health care from the state hospitals to nursing houses was insufficient to implement the idea of deinstitutionalization, the National Institute of Mental Health in 1975 created the Community Support Program (CSP) to provide funds for communities to set up a comprehensive mental health service and supports to help the mentally ill patients integrate successfully in the society. The program stressed the importance of other supports in addition to medical care, including housing, living expenses, employment, transportation, and education; and set up new national priority for people with serious mental disorders. In addition, the Congress enacted the Mental Health Systems Act of 1980 to prioritize the service to the mentally ill and emphasize the expansion of services beyond just clinical care alone.[32] Later in the 1980s, under the influence from the Congress and the Supreme Court, many programs started to help the patients regain their benefits. A new Medicaid service was also established to serve people who were diagnosed with a "chronic mental illness." People who were temporally hospitalized were also provided aid and care and a pre-release program was created to enable people to apply for reinstatement prior to discharge.[30] Not until 1990, around 35 years after the start of the deinstitutionalization, did the first state hospital begin to close. The number of hospitals dropped from around 300 by over 40 in the 1990s, and finally a Report on Mental Health showed the efficacy of mental health treatment, giving a range of treatments available for patients to choose.[32]
However, several critics maintain that deinstitutionalization has, from a mental health point of view, been a thoroughgoing failure. The seriously mentally ill are either homeless, or in prison; in either case (especially the latter), they are getting little or no mental health care. This failure is attributed to a number of reasons over which there is some degree of contention, although there is general agreement that community support programs have been ineffective at best, due to a lack of funding.[31]
Diagnosis
The causes of mental disorders are often unclear. Theories may incorporate findings from a range of fields. Mental disorders are usually defined by a combination of how a person behaves, feels, perceives, or thinks.[33] This may be associated with particular regions or functions of the brain, often in a social context. A mental disorder is one aspect of mental health. Cultural and religious beliefs, as well as social norms, should be taken into account when making a diagnosis.[34]
Psychiatrists seek to provide a medical diagnosis of individuals by an assessment of symptoms, signs and impairment associated with particular types of mental disorder. Other mental health professionals, such as clinical psychologists, may or may not apply the same diagnostic categories to their clinical formulation of a client's difficulties and circumstances.[35] The majority of mental health problems are, at least initially, assessed and treated by family physicians (in the UK general practitioners) during consultations, who may refer a patient on for more specialist diagnosis in acute or chronic cases.
Routine diagnostic practice in mental health services typically involves an interview known as a mental status examination, where evaluations are made of appearance and behavior, self-reported symptoms, mental health history, and current life circumstances. The views of other professionals, relatives or other third parties may be taken into account. A physical examination to check for ill health or the effects of medications or other drugs may be conducted. Psychological testing is sometimes used via paper-and-pen or computerized questionnaires, which may include algorithms based on ticking off standardized diagnostic criteria, and in rare specialist cases neuroimaging tests may be requested, but such methods are more commonly found in research studies than routine clinical practice.[36][37]
Time and budgetary constraints often limit practicing psychiatrists from conducting more thorough diagnostic evaluations.[38] It has been found that most clinicians evaluate patients using an unstructured, open-ended approach, with limited training in evidence-based assessment methods, and that inaccurate diagnosis may be common in routine practice.[39] In addition, comorbidity is very common in psychiatric diagnosis, where the same person meets the criteria for more than one disorder. On the other hand, a person may have several different difficulties only some of which meet the criteria for being diagnosed. There may be specific problems with accurate diagnosis in developing countries.
More structured approaches are being increasingly used to measure levels of mental illness.
- HoNOS is the most widely used measure in English mental health services, being used by at least 61 trusts.[40] In HoNOS a score of 0–4 is given for each of 12 factors, based on functional living capacity.[41] Research has been supportive of HoNOS,[42] although some questions have been asked about whether it provides adequate coverage of the range and complexity of mental illness problems, and whether the fact that often only 3 of the 12 scales vary over time gives enough subtlety to accurately measure outcomes of treatment.[43]
Criticism
Since the 1980s, Paula Caplan has been concerned about the subjectivity of psychiatric diagnosis, and people being arbitrarily "slapped with a psychiatric label." Caplan says because psychiatric diagnosis is unregulated, doctors are not required to spend much time interviewing patients or to seek a second opinion. The Diagnostic and Statistical Manual of Mental Disorders can lead a psychiatrist to focus on narrow checklists of symptoms, with little consideration of what is actually causing the person's problems. So, according to Caplan, getting a psychiatric diagnosis and label often stands in the way of recovery.[44]Template:Unreliable medical source
In 2013, psychiatrist Allen Frances wrote a paper entitled "The New Crisis of Confidence in Psychiatric Diagnosis", which said that "psychiatric diagnosis... still relies exclusively on fallible subjective judgments rather than objective biological tests." Frances was also concerned about "unpredictable overdiagnosis."[45] For many years, marginalized psychiatrists (such as Peter Breggin, Thomas Szasz) and outside critics (such as Stuart A. Kirk) have "been accusing psychiatry of engaging in the systematic medicalization of normality." More recently these concerns have come from insiders who have worked for and promoted the American Psychiatric Association (e.g., Robert Spitzer, Allen Frances).[46] A 2002 editorial in the British Medical Journal warned of inappropriate medicalization leading to disease mongering, where the boundaries of the definition of illnesses are expanded to include personal problems as medical problems or risks of diseases are emphasized to broaden the market for medications.[47]
Signs and symptoms
Course
The onset of psychiatric disorders usually occurs from childhood to early adulthood.[48] Impulse-control disorders and a few anxiety disorders tend to appear in childhood. Some other anxiety disorders, substance disorders and mood disorders emerge later in the mid-teens.[49] Symptoms of schizophrenia typically manifest from late adolescence to early twenties.[50]
The likely course and outcome of mental disorders vary and are dependent on numerous factors related to the disorder itself, the individual as a whole, and the social environment. Some disorders may last a brief period of time, while others may be long term in nature.
All disorders can have a varied course. Long-term international studies of schizophrenia have found that over a half of individuals recover in terms of symptoms, and around a fifth to a third in terms of symptoms and functioning, with many requiring no medication. While some have serious difficulties and support needs for many years, "late" recovery is still plausible. The World Health Organization concluded that the long-term studies' findings converged with others in "relieving patients, carers and clinicians of the chronicity paradigm which dominated thinking throughout much of the 20th century."[51]Template:Primary source inline[52]
Around half of people initially diagnosed with bipolar disorder achieve symptomatic recovery (no longer meeting criteria for the diagnosis) within six weeks, and nearly all achieve it within two years, with nearly half regaining their prior occupational and residential status in that period. Less than half go on to experience a new episode of mania or major depression within the next two years.[53]Template:Primary source inline
Disability
| Disorder | Disability-adjusted life years[54] |
|---|---|
| Major depressive disorder | 65.5 million |
| Alcohol-use disorder | 23.7 million |
| Schizophrenia | 16.8 million |
| Bipolar disorder | 14.4 million |
| Other drug-use disorders | 8.4 million |
| Panic disorder | 7.0 million |
| Obsessive-compulsive disorder | 5.1 million |
| Primary insomnia | 3.6 million |
| Post-traumatic stress disorder | 3.5 million |
Some disorders may be very limited in their functional effects, while others may involve substantial disability and support needs. The degree of ability or disability may vary over time and across different life domains. Furthermore, continued disability has been linked to institutionalization, discrimination and social exclusion as well as to the inherent effects of disorders. Alternatively, functioning may be affected by the stress of having to hide a condition in work or school etc., by adverse effects of medications or other substances, or by mismatches between illness-related variations and demands for regularity.[55]
It is also the case that, while often being characterized in purely negative terms, some mental traits or states labeled as disorders can also involve above-average creativity, non-conformity, goal-striving, meticulousness, or empathy.[56] In addition, the public perception of the level of disability associated with mental disorders can change.[57]
Nevertheless, internationally, people report equal or greater disability from commonly occurring mental conditions than from commonly occurring physical conditions, particularly in their social roles and personal relationships. The proportion with access to professional help for mental disorders is far lower, however, even among those assessed as having a severely disabling condition.[58] Disability in this context may or may not involve such things as:
- Basic activities of daily living. Including looking after the self (health care, grooming, dressing, shopping, cooking etc.) or looking after accommodation (chores, DIY tasks, etc.)
- Interpersonal relationships. Including communication skills, ability to form relationships and sustain them, ability to leave the home or mix in crowds or particular settings
- Occupational functioning. Ability to acquire an employment and hold it, cognitive and social skills required for the job, dealing with workplace culture, or studying as a student.
In terms of total disability-adjusted life years (DALYs), which is an estimate of how many years of life are lost due to premature death or to being in a state of poor health and disability, mental disorders rank amongst the most disabling conditions. Unipolar (also known as Major) depressive disorder is the third leading cause of disability worldwide, of any condition mental or physical, accounting for 65.5 million years lost. The first systematic description of global disability arising in youth, in 2011, found that among 10- to 24-year-olds nearly half of all disability (current and as estimated to continue) was due to mental and neurological conditions, including substance use disorders and conditions involving self-harm. Second to this were accidental injuries (mainly traffic collisions) accounting for 12 percent of disability, followed by communicable diseases at 10 percent. The disorders associated with most disability in high income countries were unipolar major depression (20%) and alcohol use disorder (11%). In the eastern Mediterranean region, it was unipolar major depression (12%) and schizophrenia (7%), and in Africa it was unipolar major depression (7%) and bipolar disorder (5%).[59]
Suicide, which is often attributed to some underlying mental disorder, is a leading cause of death among teenagers and adults under 35.[60][61] There are an estimated 10 to 20 million non-fatal attempted suicides every year worldwide.[62]
Classifications
There are currently two widely established systems that classify mental disorders:
- ICD-10 Chapter V: Mental and behavioural disorders, since 1949 part of the International Classification of Diseases produced by the WHO,
- the Diagnostic and Statistical Manual of Mental Disorders produced by the American Psychiatric Association (APA) since 1952, latest edition DSM-5 published in 2013.
Both of these list categories of disorder and provide standardized criteria for diagnosis. They have deliberately converged their codes in recent revisions so that the manuals are often broadly comparable, although significant differences remain. Other classification schemes may be used in non-western cultures, for example the Chinese Classification of Mental Disorders, and other manuals may be used by those of alternative theoretical persuasions, for example the Psychodynamic Diagnostic Manual. In general, mental disorders are classified separately from neurological disorders, learning disabilities or intellectual disability.
Unlike the DSM and ICD, some approaches are not based on identifying distinct categories of disorder using dichotomous symptom profiles intended to separate the abnormal from the normal. There is significant scientific debate about the relative merits of categorical versus such non-categorical (or hybrid) schemes, also known as continuum or dimensional models. A spectrum approach may incorporate elements of both.
In the scientific and academic literature on the definition or classification of mental disorder, one extreme argues that it is entirely a matter of value judgements (including of what is normal) while another proposes that it is or could be entirely objective and scientific (including by reference to statistical norms).[63] Common hybrid views argue that the concept of mental disorder is objective even if only a "fuzzy prototype" that can never be precisely defined, or conversely that the concept always involves a mixture of scientific facts and subjective value judgments.[64] Although the diagnostic categories are referred to as 'disorders', they are presented as medical diseases, but are not validated in the same way as most medical diagnoses. Some neurologists argue that classification will only be reliable and valid when based on neurobiological features rather than clinical interview, while others suggest that the differing ideological and practical perspectives need to be better integrated.[65][66]
The DSM and ICD approach remains under attack both because of the implied causality model[67] and because some researchers believe it better to aim at underlying brain differences which can precede symptoms by many years.[68]
Dimensional models
The high degree of comorbidity between disorders in categorical models such as the DSM and ICD have led some to propose dimensional models. Studying comorbidity between disorders have demonstrated two latent (unobserved) factors or dimensions in the structure of mental disorders that are thought to possibly reflect etiological processes. These two dimensions reflect a distinction between internalizing disorders, such as mood or anxiety symptoms, and externalizing disorders such as behavioral or substance abuse symptoms.[69] A single general factor of psychopathology, similar to the g factor for intelligence, has been empirically supported. The p factor model supports the internalizing-externalizing distinction, but also supports the formation of a third dimension of thought disorders such as schizophrenia.[70] Biological evidence also supports the validity of the internalizing-externalizing structure of mental disorders, with twin and adoption studies supporting heritable factors for externalizing and internalizing disorders.[71][72][73]
Disorders
Many disorders have been described, with signs and symptoms that vary widely between specific disorders.[74][75] There are many different categories of mental disorder, and many different facets of human behavior and personality that can become disordered.[76][77][78][79]
Anxiety disorder
Anxiety disorder: Anxiety or fear that interferes with normal functioning may be classified as an anxiety disorder.[77] Commonly recognized categories include specific phobias, generalized anxiety disorder, social anxiety disorder, panic disorder, agoraphobia, obsessive-compulsive disorder and post-traumatic stress disorder.
Mood disorder
Mood disorder: Other affective (emotion/mood) processes can also become disordered. Mood disorder involving unusually intense and sustained sadness, melancholia, or despair is known as major depression (also known as unipolar or clinical depression). Milder but still prolonged depression can be diagnosed as dysthymia. Bipolar disorder (also known as manic depression) involves abnormally "high" or pressured mood states, known as mania or hypomania, alternating with normal or depressed moods. The extent to which unipolar and bipolar mood phenomena represent distinct categories of disorder, or mix and merge along a dimension or spectrum of mood, is subject to some scientific debate.[80][81]
Psychotic disorder
Psychotic disorder: Patterns of belief, language use and perception of reality can become dysregulated (e.g., delusions, thought disorder, hallucinations). Psychotic disorders in this domain include schizophrenia, and delusional disorder. Schizoaffective disorder is a category used for individuals showing aspects of both schizophrenia and affective disorders. Schizotypy is a category used for individuals showing some of the characteristics associated with schizophrenia but without meeting cutoff criteria.
Personality disorder
Personality disorder: Personality—the fundamental characteristics of a person that influence thoughts and behaviors across situations and time—may be considered disordered if judged to be abnormally rigid and maladaptive. Although treated separately by some, the commonly used categorical schemes include them as mental disorders, albeit on a separate "axis II" in the case of the DSM-IV. A number of different personality disorders are listed, including those sometimes classed as "eccentric", such as paranoid, schizoid and schizotypal personality disorders; types that have described as "dramatic" or "emotional", such as antisocial, borderline, histrionic or narcissistic personality disorders; and those sometimes classed as fear-related, such as anxious-avoidant, dependent, or obsessive-compulsive personality disorders. The personality disorders, in general, are defined as emerging in childhood, or at least by adolescence or early adulthood. The ICD also has a category for enduring personality change after a catastrophic experience or psychiatric illness. If an inability to sufficiently adjust to life circumstances begins within three months of a particular event or situation, and ends within six months after the stressor stops or is eliminated, it may instead be classed as an adjustment disorder. There is an emerging consensus that so-called "personality disorders", like personality traits in general, actually incorporate a mixture of acute dysfunctional behaviors that may resolve in short periods, and maladaptive temperamental traits that are more enduring.[82] Furthermore, there are also non-categorical schemes that rate all individuals via a profile of different dimensions of personality without a symptom-based cutoff from normal personality variation, for example through schemes based on dimensional models.[83]Template:Primary source inline
Eating disorder
Eating disorder: These disorders involve disproportionate concern in matters of food and weight.[77] Categories of disorder in this area include anorexia nervosa, bulimia nervosa, exercise bulimia or binge eating disorder.[84][85]
Sleep disorder
Sleep disorder: These conditions are associated with disruption to normal sleep patterns. A common sleep disorder is insomnia, which is described as difficulty falling and/or staying asleep.
Sexual disorders and gender dysphoria: These disorders include dyspareunia and various kinds of paraphilia (sexual arousal to objects, situations, or individuals that are considered abnormal or harmful to the person or others).
Other
Impulse control disorder: People who are abnormally unable to resist certain urges or impulses that could be harmful to themselves or others, may be classified as having an impulse control disorder, and disorders such as kleptomania (stealing) or pyromania (fire-setting). Various behavioral addictions, such as gambling addiction, may be classed as a disorder. Obsessive-compulsive disorder can sometimes involve an inability to resist certain acts but is classed separately as being primarily an anxiety disorder.
Substance use disorder: This disorder refers to the use of drugs (legal or illegal, including alcohol) that persists despite significant problems or harm related to its use. Substance dependence and substance abuse fall under this umbrella category in the DSM. Substance use disorder may be due to a pattern of compulsive and repetitive use of a drug that results in tolerance to its effects and withdrawal symptoms when use is reduced or stopped.
Dissociative disorder: People who suffer severe disturbances of their self-identity, memory and general awareness of themselves and their surroundings may be classified as having these types of disorders, including depersonalization disorder or dissociative identity disorder (which was previously referred to as multiple personality disorder or "split personality").
Cognitive disorder: These affect cognitive abilities, including learning and memory. This category includes delirium and mild and major neurocognitive disorder (previously termed dementia).
Developmental disorder: These disorders initially occur in childhood. Some examples include autism spectrum disorders, oppositional defiant disorder and conduct disorder, and attention deficit hyperactivity disorder (ADHD), which may continue into adulthood. Conduct disorder, if continuing into adulthood, may be diagnosed as antisocial personality disorder (dissocial personality disorder in the ICD). Popularist labels such as psychopath (or sociopath) do not appear in the DSM or ICD but are linked by some to these diagnoses.
Somatoform disorders may be diagnosed when there are problems that appear to originate in the body that are thought to be manifestations of a mental disorder. This includes somatization disorder and conversion disorder. There are also disorders of how a person perceives their body, such as body dysmorphic disorder. Neurasthenia is an old diagnosis involving somatic complaints as well as fatigue and low spirits/depression, which is officially recognized by the ICD-10 but no longer by the DSM-IV.[86]Template:Primary source inline
Factitious disorders, such as Munchausen syndrome, are diagnosed where symptoms are thought to be experienced (deliberately produced) and/or reported (feigned) for personal gain.
There are attempts to introduce a category of relational disorder, where the diagnosis is of a relationship rather than on any one individual in that relationship. The relationship may be between children and their parents, between couples, or others. There already exists, under the category of psychosis, a diagnosis of shared psychotic disorder where two or more individuals share a particular delusion because of their close relationship with each other.
There are a number of uncommon psychiatric syndromes, which are often named after the person who first described them, such as Capgras syndrome, De Clerambault syndrome, Othello syndrome, Ganser syndrome, Cotard delusion, and Ekbom syndrome, and additional disorders such as the Couvade syndrome and Geschwind syndrome.[87]
Various new types of mental disorder diagnosis are occasionally proposed. Among those controversially considered by the official committees of the diagnostic manuals include self-defeating personality disorder, sadistic personality disorder, passive-aggressive personality disorder and premenstrual dysphoric disorder.
Risk factors
The predominant view as of 2018 is that genetic, psychological, and environmental factors all contribute to the development or progression of mental disorders.[88] Different risk factors may be present at different ages, with risk occurring as early as during prenatal period.[89]
Genetics
A number of psychiatric disorders are linked to a family history (including depression, narcissistic personality disorder[90][91] and anxiety).[92] Twin studies have also revealed a very high heritability for many mental disorders (especially autism and schizophrenia).[93] Although researchers have been looking for decades for clear linkages between genetics and mental disorders, that work has not yielded specific genetic biomarkers yet that might lead to better diagnosis and better treatments.[94]
Statistical research looking at eleven disorders found widespread assortative mating between people with mental illness. That means that individuals with one of these disorders were two to three times more likely than the general population to have a partner with a mental disorder. Sometimes people seemed to have preferred partners with the same mental illness. Thus, people with schizophrenia or ADHD are seven times more likely to have affected partners with the same disorder. This is even more pronounced for people with Autism spectrum disorders who are 10 times more likely to have a spouse with the same disorder.[95]
Environment
During the prenatal stage, factors like unwanted pregnancy, lack of adaptation to pregnancy or substance abuse during pregnancy increases the risk of developing a mental disorder.[89] Maternal stress and birth complications including prematurity and infections have also been implicated in increasing susceptibility for mental illness.[96] Infants neglected or not provided optimal nutrition have a higher risk of developing cognitive impairment.[89]
Social influences have also been found to be important,[97] including abuse, neglect, bullying, social stress, traumatic events, and other negative or overwhelming life experiences. Aspects of the wider community have also been implicated,[98] including employment problems, socioeconomic inequality, lack of social cohesion, problems linked to migration, and features of particular societies and cultures. The specific risks and pathways to particular disorders are less clear, however.
Nutrition also plays a role in mental disorders.[33][99]
In schizophrenia and psychosis, risk factors include migration and discrimination, childhood trauma, bereavement or separation in families, abuse of drugs,[100] and urbanicity.[98]
In anxiety, risk factors may include parenting factors including parental rejection, lack of parental warmth, high hostility, harsh discipline, high maternal negative affect, anxious childrearing, modelling of dysfunctional and drug-abusing behaviour, and child abuse (emotional, physical and sexual).[101] Adults with imbalance work to life are at higher risk for developing anxiety.[89]
For bipolar disorder, stress (such as childhood adversity) is not a specific cause, but does place genetically and biologically vulnerable individuals at risk for a more severe course of illness.[102]
Drug use
Mental disorders are associated with drug use including: cannabis,[103] alcohol[104] and caffeine,[105] use of which appears to promote anxiety.[106] For psychosis and schizophrenia, usage of a number of drugs has been associated with development of the disorder, including cannabis, cocaine, and amphetamines.[107][103] There has been debate regarding the relationship between usage of cannabis and bipolar disorder.[108] Cannabis has also been associated with depression.[103] Adolescents are at increased risk for tobacco, alcohol and drug use; Peer pressure is the main reason why adolescents start using substances. At this age, the use of substances could be detrimental to the development of the brain and place them at higher risk of developing a mental disorder.[89]
Chronic disease
People living with chronic conditions like HIV and diabetes are at higher risk for developing a mental disorder. People living with diabetes experience significant stress from biological impact of the disease, which places them at risk for developing anxiety and depression. Diabetic patients also have to deal with emotional stress trying to manage the disease. Conditions like heart disease, stroke, respiratory conditions, cancer and arthritis increase the risk of developing a mental disorder when compared to the general population.[109]
Personality traits
Risk factors for mental illness include a propensity for high neuroticism[110][111] or "emotional instability". In anxiety, risk factors may include temperament and attitudes (e.g. pessimism).[92]
Causal models
Mental disorders can arise from multiple sources, and in many cases there is no single accepted or consistent cause currently established. An eclectic or pluralistic mix of models may be used to explain particular disorders.[111][112] The primary paradigm of contemporary mainstream Western psychiatry is said to be the biopsychosocial model which incorporates biological, psychological and social factors, although this may not always be applied in practice.
Biological psychiatry follows a biomedical model where many mental disorders are conceptualized as disorders of brain circuits likely caused by developmental processes shaped by a complex interplay of genetics and experience. A common assumption is that disorders may have resulted from genetic and developmental vulnerabilities, exposed by stress in life (for example in a diathesis–stress model), although there are various views on what causes differences between individuals. Some types of mental disorders may be viewed as primarily neurodevelopmental disorders.
Evolutionary psychology may be used as an overall explanatory theory, while attachment theory is another kind of evolutionary-psychological approach sometimes applied in the context of mental disorders. Psychoanalytic theories have continued to evolve alongside and cognitive-behavioral and systemic-family approaches. A distinction is sometimes made between a "medical model" or a "social model" of disorder and disability.
Prevention
The 2004 WHO report "Prevention of Mental Disorders" stated that "Prevention of these disorders is obviously one of the most effective ways to reduce the [disease] burden."[113] The 2011 European Psychiatric Association (EPA) guidance on prevention of mental disorders states "There is considerable evidence that various psychiatric conditions can be prevented through the implementation of effective evidence-based interventions."[114] A 2011 UK Department of Health report on the economic case for mental health promotion and mental illness prevention found that "many interventions are outstandingly good value for money, low in cost and often become self-financing over time, saving public expenditure".[115] In 2016, the National Institute of Mental Health re-affirmed prevention as a research priority area.[116]
Parenting may affect the child's mental health, and evidence suggests that helping parents to be more effective with their children can address mental health needs.[117][118]
Universal prevention (aimed at a population that has no increased risk for developing a mental disorder, such as school programs or mass media campaigns) need very high numbers of people to show effect (sometimes known as the "power" problem). Approaches to overcome this are (1) focus on high-incidence groups (e.g. by targeting groups with high risk factors), (2) use multiple interventions to achieve greater, and thus more statistically valid, effects, (3) use cumulative meta-analyses of many trials, and (4) run very large trials.[119][120]
Management
Services are based in psychiatric hospitals or in the community, and assessments are carried out by mental health professionals such as psychiatrists, psychologists, psychiatric nurses and clinical social workers, using various methods such as psychometric tests but often relying on observation and questioning. Treatments are provided by various mental health professionals. Psychotherapy and psychiatric medication are two major treatment options. Other treatments include lifestyle changes, social interventions, peer support, and self-help. In a minority of cases, there might be involuntary detention or treatment. Prevention programs have been shown to reduce depression.[33][121]
Treatment and support for mental disorders is provided in psychiatric hospitals, clinics or a range of community mental health services. In some countries services are increasingly based on a recovery approach, intended to support individual's personal journey to gain the kind of life they want.
There are a range of different types of treatment and what is most suitable depends on the disorder and the individual. Many things have been found to help at least some people, and a placebo effect may play a role in any intervention or medication. In a minority of cases, individuals may be treated against their will, which can cause particular difficulties depending on how it is carried out and perceived. Compulsory treatment while in the community versus non-compulsory treatment does not appear to make much of a difference except by maybe decreasing victimization.[122]
Lifestyle
Lifestyle strategies, including dietary changes, exercise and quitting smoking may be of benefit.[121][99][123]
Therapy
There is also a wide range of psychotherapists (including family therapy), counselors, and public health professionals. In addition, there are peer support roles where personal experience of similar issues is the primary source of expertise.[124][125][126][127]
A major option for many mental disorders is psychotherapy. There are several main types. Cognitive behavioral therapy (CBT) is widely used and is based on modifying the patterns of thought and behavior associated with a particular disorder. Other psychotherapy include dialectic behavioral therapy (DBT) and interpersonal psychotherapy (IPT). Psychoanalysis, addressing underlying psychic conflicts and defenses, has been a dominant school of psychotherapy and is still in use. Systemic therapy or family therapy is sometimes used, addressing a network of significant others as well as an individual.
Some psychotherapies are based on a humanistic approach. There are a number of specific therapies used for particular disorders, which may be offshoots or hybrids of the above types. Mental health professionals often employ an eclectic or integrative approach. Much may depend on the therapeutic relationship, and there may be problems with trust, confidentiality and engagement.
Medication
Pharmacotherapy is a therapy that uses pharmaceutical drugs. Pharmacotherapy is used in the treatment of mental illness through the use of antidepressants, benzodiazepines, and the use of elements such as lithium. A major option for many mental disorders is psychiatric medication and there are several main groups. Antidepressants are used for the treatment of clinical depression, as well as often for anxiety and a range of other disorders. Anxiolytics (including sedatives) are used for anxiety disorders and related problems such as insomnia. Mood stabilizers are used primarily in bipolar disorder. Antipsychotics are used for psychotic disorders, notably for positive symptoms in schizophrenia, and also increasingly for a range of other disorders. Stimulants are commonly used, notably for ADHD.[128]
Despite the different conventional names of the drug groups, there may be considerable overlap in the disorders for which they are actually indicated, and there may also be off-label use of medications. There can be problems with adverse effects of medication and adherence to them, and there is also criticism of pharmaceutical marketing and professional conflicts of interest. However, these medications in combination with non-pharmacological methods, such as cognitive behavioral therapy (CBT) are seen to be most effective in treating mental disorders.
Other
Electroconvulsive therapy (ECT) is sometimes used in severe cases when other interventions for severe intractable depression have failed. ECT is usually indicated for treatment resistant depression, severe vegetative symptoms, psychotic depression, intense suicidal ideation, depression during pregnancy, and catonia. Psychosurgery is considered experimental but is advocated by some neurologists in certain rare cases.[129][130]
Counseling (professional) and co-counseling (between peers) may be used. Psychoeducation programs may provide people with the information to understand and manage their problems. Creative therapies are sometimes used, including music therapy, art therapy or drama therapy. Lifestyle adjustments and supportive measures are often used, including peer support, self-help groups for mental health and supported housing or supported employment (including social firms). Some advocate dietary supplements.[131]
Reasonable accommodations (adjustments and supports) might be put in place to help an individual cope and succeed in environments despite potential disability related to mental health problems. This could include an emotional support animal or specifically trained psychiatric service dog. As of 2019 cannabis is specifically not recommended as a treatment.[132]
Demographics
Mental disorders are common. Stigma and discrimination can add to the suffering and disability associated with mental disorders, leading to various social movements attempting to increase understanding and challenge social exclusion.
Evidence from the WHO suggests that nearly half of the world's population is affected by mental illness with an impact on their self-esteem, relationships and ability to function in everyday life.[133] An individual's emotional health can impact their physical health. Poor mental health can lead to problems such as the ability to make adequate decisions and substance abuse.[134]
Good mental health can improve life quality whereas poor mental health can worsen it. According to Richards, Campania, & Muse-Burke, "There is growing evidence that is showing emotional abilities are associated with pro-social behaviors such as stress management and physical health."[134] Their research also concluded that people who lack emotional expression are inclined to anti-social behaviors (e.g., drug and alcohol abuse, physical fights, vandalism), which reflects ones mental health and suppressed emotions.[134] Adults and children who face mental illness may experience social stigma, which can exacerbate the issues.[135]
Children and young adults
According to 2020 data, mental illnesses have a stagnant incidence among adults but are increasing among the youth, categorized as 12 to 17-year-olds.[136] Approximately 13% of youth in the United States reported suffering from at least one major depressive episode in 2019-20, with the greatest increase (18%) in Oregon.[136] Only 28% receive consistent treatment and 70% are left untreated.[136] In lower-income communities, it is more common to forego treatment as a result of financial resources. Being left untreated also leads to unhealthy coping mechanisms such as substance abuse, which in turn causes its own host of mental health issues.
Mental health and stability is a very important factor in a person's everyday life. The human brain develops many skills at an early age including social skills, behavioral skills, and one's way of thinking. Learning how to interact with others and how to focus on certain subjects are essential lessons to learn at a young age. This starts from the time we can talk all the way to when we are so old that we can barely walk. However, there are people in society who have difficulties with these skills and behave differently. A mental illness consists of a wide range of conditions that affects a person's mood, thinking, and behavior.[137] About 26% of people in the United States, ages 18 and older, have been diagnosed with some kind of mental disorder. However, not much is said about children with mental illnesses even though many develop one, even as early as age three.
The most common mental illnesses in children include, but are not limited to anxiety disorder, as well as depression in older children and teens. Having a mental illness at a younger age is different from having one in adulthood. Children's brains are still developing and will continue to develop until around the age of twenty-five.[138] When a mental illness is thrown into the mix, it becomes significantly harder for a child to acquire the necessary skills and habits that people use throughout the day. For example, behavioral skills don't develop as fast as motor or sensory skills do.[138] So when a child has an anxiety disorder, they begin to lack proper social interaction and associate many ordinary things with intense fear.[139] This can be scary for the child because they don't necessarily understand why they act and think the way that they do. Many researchers say that parents should keep an eye on their child if they have any reason to believe that something is slightly off.[138] If the children are evaluated earlier, they become more acquainted to their disorder and treating it becomes part of their daily routine.[138] This is opposed to adults who might not recover as quickly because it is more difficult for them to adopt when already being accustomed to a certain direction of life.
Mental illness affects not only the person themselves but the people around them. Friends and family also play an important role in the child's mental health stability and treatment.[140] If the child is young, parents are the ones who evaluate their child and decide whether or not they need some form of help.[141] Friends are a support system for the child and family as a whole. Living with a mental disorder is never easy, so it's always important to have people around to make the days a little easier. However, there are negative factors that come with the social aspect of mental illness as well. Parents are sometimes held responsible for their child's illness.[141] People also say that the parents raised their children in a certain way or they acquired their behavior from them. Family and friends are sometimes so ashamed of the idea of being close to someone with a disorder that the child feels isolated and thinks that they have to hide their illness from others.[141] When in reality, hiding it from people prevents the child from getting the right amount of social interaction and treatment to thrive in today's society.
Stigmas are also a well-known factor in mental illness. A stigma is defined as “a mark of disgrace associated with a particular circumstance, quality, or person.” Stigmas are used especially when it comes to mentally disabled people. One example of such a stigma is the assumption that everyone with a mental problem, no matter how mild or severe, is automatically considered destructive or a criminal person.[142] However, mental illnesses differ from their portrayal in the media. In a recent study, a majority of young people associate mental illness with extreme sadness or violent tendencies .[143] Many people with psychiatric disorders like ADHD or anxiety can live an ordinary life with the correct treatment. Along with social stigmas, individuals with a mental illness can develop a self-stigma. A self-stigma is when the affected individual does not come forward about their feelings in fear of being judged. These self-stigmas can deter the individual from seeking help and treatment.[144]
Sueki, (2013) carried out a study titled “The effect of suicide-related internet use on users’ mental health: A longitudinal Study”. This study investigated the effects of suicide-related internet use on user's suicidal thoughts, predisposition to depression and anxiety, and loneliness. The study consisted of 850 internet users; the data was obtained by carrying out a questionnaire amongst the participants. This study found that browsing websites related to suicide, and methods used to commit suicide, harmed suicidal thoughts and increased depression and anxiety tendencies. The study concluded that as suicide-related internet use adversely affected the mental health of certain age groups it may be prudent to reduce or control their exposure to these websites. These findings certainly suggest that the internet can indeed have a profoundly negative impact on our mental health.[145]
Psychiatrist Thomas Szasz compared that 50 years ago children were either categorized as good or bad, and today "all children are good, but some are mentally healthy and others are mentally ill". Social control and forced identity creation is the cause of many mental health problems among today's children.[146] A behavior or misbehavior might not be an illness but exercise of their free will and today's immediacy in drug administration for every problem along with the legal over-guarding and regard of a child's status as a dependent shakes their personal self and invades their internal growth.
The homeless population
Mental illness is not only prevalent among children and young adults but also the homeless. Mental illness is thought to be extremely prevalent among homeless populations, though access to proper diagnoses is limited. In an article written by Lisa Godman and her colleagues, they reference Smith’s research on the prevalence of PTSD among homeless people. His research stated, "Homelessness itself is a risk factor for emotional disorder."[147] What this quote is saying is that being homeless itself can cause the emotional disorder. Without looking for other reasons for emotional disorder and really looking at the simple fact that an individual is homeless can cause the emotional disorder. Godman’s article stated "Recently, Smith ( 1991) investigated the prevalence of PTSD among a sample of 300 randomly selected homeless single women and mothers in St. Louis, Missouri. Using the Diagnostic Interview Schedule (DIS; Robins, 1981; Robins & Helzer, 1984), she found that 53% of the respondents could be diagnosed as exhibiting full-blown cases of PTSD."Template:Cite quote As the source explains, the conclusion that was drawn from Smith’s investigation after studying 300 homeless individuals is that 53% of those people were eligible to be diagnosed with PTSD. She continues and states: "In addition, data from clinical observations, self-reports, and empirical studies suggest that at least two commonly reported symptoms of psychological trauma, social disaffiliation and learned helplessness are highly prevalent among homeless individuals and families."[148] Other data were able to prove that PTSD and learned helplessness were two symptoms that were very much present among homeless individuals and families. The question would be how are these people being helped. This is evident that mental health among the homeless is an issue existing but barely touched.[149] In another article by Stephen W. Hwang and Rochelle E Garner, they talk about the ways that the homeless are getting actually getting help. It states "For homeless people with mental illness, case management linked to other services was effective in improving psychiatric symptoms, and assertive case management was effective in decreasing psychiatric hospitalizations and increasing outpatient contacts. For homeless people with substance abuse problems, case management resulted in greater decreases in substance use than did usual care."[150] The question would be how are these people being helped. As the source explained, case management provided by services helped improve psychiatric symptoms. It also caused a decrease in substance use than usual media care.[151]
Cultural and religious considerations
Mental health is a socially constructed and socially defined concept; that is, different societies, groups, cultures, institutions, and professions have very different ways of conceptualizing its nature and causes, determining what is mentally healthy, and deciding what interventions, if any, are appropriate.[152] Thus, different professionals will have different cultural, class, political and religious backgrounds, which will impact the methodology applied during treatment. In the context of deaf mental health care, it is necessary for professionals to have cultural competency of deaf and hard of hearing people and to understand how to properly rely on trained, qualified, and certified interpreters when working with culturally Deaf clients.
Research has shown that there is stigma attached to mental illness.[153] Due to such stigma, individuals may resist 'labeling' and may be driven to respond to mental health diagnoses with denialism.[154] Family caregivers of individuals with mental disorders may also suffer discrimination or face stigma.[155]
Addressing and eliminating the social stigma and perceived stigma attached to mental illness has been recognized as crucial to education and awareness surrounding mental health issues. In the United Kingdom, the Royal College of Psychiatrists organized the campaign Changing Minds (1998–2003) to help reduce stigma,[156] while in the United States, efforts by entities such as the Born This Way Foundation and The Manic Monologues specifically focus on removing the stigma surrounding mental illness.[157][158] The National Alliance on Mental Illness is a U.S. institution founded in 1979 to represent and advocate for those struggling with mental health issues. NAMI helps to educate about mental illnesses and health issues, while also working to eliminate stigma[159] attached to these disorders.
Many mental health professionals are beginning to, or already understand, the importance of competency in religious diversity and spirituality. They are also partaking in cultural training to better understand which interventions work best for these different groups of people. The American Psychological Association explicitly states that religion must be respected. Education in spiritual and religious matters is also required by the American Psychiatric Association,[160] however, far less attention is paid to the damage that more rigid, fundamentalist faiths commonly practiced in the United States can cause.[161] This theme has been widely politicized in 2018 such as with the creation of the Religious Liberty Task Force in July of that year.[162] Also, many providers and practitioners in the United States are only beginning to realize that the institution of mental healthcare lacks knowledge and competence of many non-Western cultures, leaving providers in the United States ill-equipped to treat patients from different cultures.[163]
Society and culture
Different societies or cultures, even different individuals in a subculture, can disagree as to what constitutes optimal versus pathological biological and psychological functioning. Research has demonstrated that cultures vary in the relative importance placed on, for example, happiness, autonomy, or social relationships for pleasure. Likewise, the fact that a behavior pattern is valued, accepted, encouraged, or even statistically normative in a culture does not necessarily mean that it is conducive to optimal psychological functioning.
People in all cultures find some behaviors bizarre or even incomprehensible. But just what they feel is bizarre or incomprehensible is ambiguous and subjective.[164] These differences in determination can become highly contentious. The process by which conditions and difficulties come to be defined and treated as medical conditions and problems, and thus come under the authority of doctors and other health professionals, is known as medicalization or pathologization.
Religion
Religious, spiritual, or transpersonal experiences and beliefs meet many criteria of delusional or psychotic disorders.[165][166] A belief or experience can sometimes be shown to produce distress or disability—the ordinary standard for judging mental disorders.[167] There is a link between religion and schizophrenia,[168] a complex mental disorder characterized by a difficulty in recognizing reality, regulating emotional responses, and thinking in a clear and logical manner. Those with schizophrenia commonly report some type of religious delusion,[168][169][170] and religion itself may be a trigger for schizophrenia.[171]
Cultural bias
Current diagnostic guidelines, namely the DSM and to some extent the ICD, have been criticized as having a fundamentally Euro-American outlook. Opponents argue that even when diagnostic criteria are used across different cultures, it does not mean that the underlying constructs have validity within those cultures, as even reliable application can prove only consistency, not legitimacy.[172] Advocating a more culturally sensitive approach, critics such as Carl Bell and Marcello Maviglia contend that the cultural and ethnic diversity of individuals is often discounted by researchers and service providers.[173]
Cross-cultural psychiatrist Arthur Kleinman contends that the Western bias is ironically illustrated in the introduction of cultural factors to the DSM-IV. Disorders or concepts from non-Western or non-mainstream cultures are described as "culture-bound", whereas standard psychiatric diagnoses are given no cultural qualification whatsoever, revealing to Kleinman an underlying assumption that Western cultural phenomena are universal.[174] Kleinman's negative view towards the culture-bound syndrome is largely shared by other cross-cultural critics. Common responses included both disappointment over the large number of documented non-Western mental disorders still left out and frustration that even those included are often misinterpreted or misrepresented.[175]
Many mainstream psychiatrists are dissatisfied with the new culture-bound diagnoses, although for partly different reasons. Robert Spitzer, a lead architect of the DSM-III, has argued that adding cultural formulations was an attempt to appease cultural critics, and has stated that they lack any scientific rationale or support. Spitzer also posits that the new culture-bound diagnoses are rarely used, maintaining that the standard diagnoses apply regardless of the culture involved. In general, mainstream psychiatric opinion remains that if a diagnostic category is valid, cross-cultural factors are either irrelevant or are significant only to specific symptom presentations.[172]
Clinical conceptions of mental illness also overlap with personal and cultural values in the domain of morality, so much so that it is sometimes argued that separating the two is impossible without fundamentally redefining the essence of being a particular person in a society.[176] In clinical psychiatry, persistent distress and disability indicate an internal disorder requiring treatment; but in another context, that same distress and disability can be seen as an indicator of emotional struggle and the need to address social and structural problems.[177][178] This dichotomy has led some academics and clinicians to advocate a postmodernist conceptualization of mental distress and well-being.[179][180]
Such approaches, along with cross-cultural and "heretical" psychologies centered on alternative cultural and ethnic and race-based identities and experiences, stand in contrast to the mainstream psychiatric community's alleged avoidance of any explicit involvement with either morality or culture.[181] In many countries there are attempts to challenge perceived prejudice against minority groups, including alleged institutional racism within psychiatric services.[182] There are also ongoing attempts to improve professional cross cultural sensitivity.
Laws and policies
Three-quarters of countries around the world have mental health legislation. Compulsory admission to mental health facilities (also known as involuntary commitment) is a controversial topic. It can impinge on personal liberty and the right to choose, and carry the risk of abuse for political, social and other reasons; yet it can potentially prevent harm to self and others, and assist some people in attaining their right to healthcare when they may be unable to decide in their own interests.[183]
All human rights oriented mental health laws require proof of the presence of a mental disorder as defined by internationally accepted standards, but the type and severity of disorder that counts can vary in different jurisdictions. The two most often used grounds for involuntary admission are said to be serious likelihood of immediate or imminent danger to self or others, and the need for treatment. Applications for someone to be involuntarily admitted usually come from a mental health practitioner, a family member, a close relative, or a guardian. Human-rights-oriented laws usually stipulate that independent medical practitioners or other accredited mental health practitioners must examine the patient separately and that there should be regular, time-bound review by an independent review body.[183] The individual should also have personal access to independent advocacy.
For involuntary treatment to be administered (by force if necessary), it should be shown that an individual lacks the mental capacity for informed consent (i.e. to understand treatment information and its implications, and therefore be able to make an informed choice to either accept or refuse). Legal challenges in some areas have resulted in supreme court decisions that a person does not have to agree with a psychiatrist's characterization of the issues as constituting an "illness", nor agree with a psychiatrist's conviction in medication, but only recognize the issues and the information about treatment options.[184]
Proxy consent (also known as surrogate or substituted decision-making) may be transferred to a personal representative, a family member or a legally appointed guardian. Moreover, patients may be able to make, when they are considered well, an advance directive stipulating how they wish to be treated should they be deemed to lack mental capacity in future.[183] The right to supported decision-making, where a person is helped to understand and choose treatment options before they can be declared to lack capacity, may also be included in legislation.[185] There should at the very least be shared decision-making as far as possible. Involuntary treatment laws are increasingly extended to those living in the community, for example outpatient commitment laws (known by different names) are used in New Zealand, Australia, the United Kingdom and most of the United States.
The World Health Organization reports that in many instances national mental health legislation takes away the rights of persons with mental disorders rather than protecting rights, and is often outdated.[183] In 1991, the United Nations adopted the Principles for the Protection of Persons with Mental Illness and the Improvement of Mental Health Care, which established minimum human rights standards of practice in the mental health field. In 2006, the UN formally agreed the Convention on the Rights of Persons with Disabilities to protect and enhance the rights and opportunities of disabled people, including those with psychosocial disabilities.[186]
The term insanity, sometimes used colloquially as a synonym for mental illness, is often used technically as a legal term. The insanity defense may be used in a legal trial (known as the mental disorder defence in some countries).
Perception and discrimination
Stigma
The social stigma associated with mental disorders is a widespread problem. The US Surgeon General stated in 1999 that: "Powerful and pervasive, stigma prevents people from acknowledging their own mental health problems, much less disclosing them to others."[187] In the United States, racial and ethnic minorities are more likely to experience mental health disorders often due to low socioeconomic status, and discrimination.[188][189] In Taiwan, those with mental disorders are subject to general public's misperception that the root causes of the mental disorders are "over-thinking", "having a lot of time and nothing better to do", "stagnant", "not serious in life", "not paying enough attention to the real life affairs", "mentally weak", "refusing to be resilient", "turning back to perfectionistic strivings", "not bravery" and so forth.[190]
Employment discrimination is reported to play a significant part in the high rate of unemployment among those with a diagnosis of mental illness.[191] An Australian study found that having a mental illness is a bigger barrier to employment than a physical disability.[192]Template:Better source The mentally ill are stigmatized in Chinese society and can not legally marry.[193]
Efforts are being undertaken worldwide to eliminate the stigma of mental illness,[194] although the methods and outcomes used have sometimes been criticized.[195]
Media and general public
Media coverage of mental illness comprises predominantly negative and pejorative depictions, for example, of incompetence, violence or criminality, with far less coverage of positive issues such as accomplishments or human rights issues.[196][197][198] Such negative depictions, including in children's cartoons, are thought to contribute to stigma and negative attitudes in the public and in those with mental health problems themselves, although more sensitive or serious cinematic portrayals have increased in prevalence.[199][200]
In the United States, the Carter Center has created fellowships for journalists in South Africa, the U.S., and Romania, to enable reporters to research and write stories on mental health topics.[201] Former US First Lady Rosalynn Carter began the fellowships not only to train reporters in how to sensitively and accurately discuss mental health and mental illness, but also to increase the number of stories on these topics in the news media.[202][203] There is also a World Mental Health Day, which in the US and Canada falls within a Mental Illness Awareness Week.
The general public have been found to hold a strong stereotype of dangerousness and desire for social distance from individuals described as mentally ill.[204] A US national survey found that a higher percentage of people rate individuals described as displaying the characteristics of a mental disorder as "likely to do something violent to others", compared to the percentage of people who are rating individuals described as being "troubled".[205]
Recent depictions in media have included leading characters successfully living with and managing a mental illness, including in bipolar disorder in Homeland (2011) and posttraumatic stress disorder in Iron Man 3 (2013).Template:Original research inline
Violence
Despite public or media opinion, national studies have indicated that severe mental illness does not independently predict future violent behavior, on average, and is not a leading cause of violence in society. There is a statistical association with various factors that do relate to violence (in anyone), such as substance abuse and various personal, social and economic factors.[206] A 2015 review found that in the United States, about 4% of violence is attributable to people diagnosed with mental illness,[207] and a 2014 study found that 7.5% of crimes committed by mentally ill people were directly related to the symptoms of their mental illness.[208] The majority of people with serious mental illness are never violent.[209]
In fact, findings consistently indicate that it is many times more likely that people diagnosed with a serious mental illness living in the community will be the victims rather than the perpetrators of violence.[210][211] In a study of individuals diagnosed with "severe mental illness" living in a US inner-city area, a quarter were found to have been victims of at least one violent crime over the course of a year, a proportion eleven times higher than the inner-city average, and higher in every category of crime including violent assaults and theft.[212] People with a diagnosis may find it more difficult to secure prosecutions, however, due in part to prejudice and being seen as less credible.[213]
However, there are some specific diagnoses, such as childhood conduct disorder or adult antisocial personality disorder or psychopathy, which are defined by, or are inherently associated with, conduct problems and violence. There are conflicting findings about the extent to which certain specific symptoms, notably some kinds of psychosis (hallucinations or delusions) that can occur in disorders such as schizophrenia, delusional disorder or mood disorder, are linked to an increased risk of serious violence on average. The mediating factors of violent acts, however, are most consistently found to be mainly socio-demographic and socio-economic factors such as being young, male, of lower socioeconomic status and, in particular, substance abuse (including alcoholism) to which some people may be particularly vulnerable.[56][210][214][215]
High-profile cases have led to fears that serious crimes, such as homicide, have increased due to deinstitutionalization, but the evidence does not support this conclusion.[215][216] Violence that does occur in relation to mental disorder (against the mentally ill or by the mentally ill) typically occurs in the context of complex social interactions, often in a family setting rather than between strangers.[217] It is also an issue in health care settings[218] and the wider community.[219]
Mental health
The recognition and understanding of mental health conditions have changed over time and across cultures and there are still variations in definition, assessment and classification, although standard guideline criteria are widely used. In many cases, there appears to be a continuum between mental health and mental illness, making diagnosis complex.[78] According to the World Health Organization (WHO), over a third of people in most countries report problems at some time in their life which meet criteria for diagnosis of one or more of the common types of mental disorder.[220] Corey M Keyes has created a two continua model of mental illness and health which holds that both are related, but distinct dimensions: one continuum indicates the presence or absence of mental health, the other the presence or absence of mental illness.[221] For example, people with optimal mental health can also have a mental illness, and people who have no mental illness can also have poor mental health.[222]
Notes
- ↑ Mental illness – Symptoms and causes (8 June 2019).
- ↑ Derek Bolton, What is Mental Disorder?: An Essay in Philosophy, Science, and Values (Oxford University Press, 2008, ISBN 978-0198565925).
- ↑ Dan J. Stein, What is a mental disorder? A perspective from cognitive-affective science Canadian Journal of Psychiatry 58(12) (2013): 656–662. Retrieved June 2, 2021.
- ↑ American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5 (American Psychiatric Publishing, 2013, ISBN 978-0890425558).
- ↑ Chapter 6: Mental, behavioural or neurodevelopmental disorders ICD-11 for Mortality and Morbidity Statistics. Retrieved June 2, 2021.
- ↑ Neil Pickering, The Metaphor of Mental Illness (Oxford University Press, 2006, ISBN 978-0198530879).
- ↑ L.J. Rapport, R.M. Todd, M.A. Lumley, and S.A. Fisicaro, The diagnostic meaning of "nervous breakdown" among lay populations Journal of Personality Assessment 71(2) (1998):242-252. Retrieved June 2, 2021.
- ↑ Nervous breakdown Health Direct, August, 2019. Retrieved June 2, 2021.
- ↑ 9.0 9.1 9.2 9.3 David H. Barlow, Vincent Mark Durand, and Stefan G. Hofmann, Abnormal Psychology: An integrative approach (Cengage Learning, 2017, ISBN 978-1305950443).
- ↑ Karen Rhea Nemet-Nejat, Daily Life in Ancient Mesopotamia (Greenwood, 1998, ISBN 978-0313294976).
- ↑ 11.0 11.1 Jeremy Black and Anthony Green, Gods, Demons and Symbols of Ancient Mesopotamia: An Illustrated Dictionary (University of Texas Press, 1992, ISBN 978-0292707948).
- ↑ Amy E. Wenzel, The SAGE Encyclopedia of Abnormal and Clinical Psychology (SAGE Publications, Inc., 2017, ISBN 978-1483365831).
- ↑ T.J. Schoeneman, The role of mental illness in the European witch hunts of the sixteenth and seventeenth centuries: an assessment Journal of the History of the Behavioral Sciences 13(4) (1977):337–351. Retrieved June 2, 2021.
- ↑ Template:Cite document
- ↑ (December 2010) The economic consequences of deinstitutionalisation of mental health services: lessons from a systematic review of European experience: Economic consequences of deinstitutionalisation of mental health services. Health & Social Care in the Community 19 (2): 113–125.
- ↑ 16.0 16.1 16.2 (December 2010) Mental health care and the politics of inclusion: A social systems account of psychiatric deinstitutionalization. Theoretical Medicine and Bioethics 31 (6): 411–427.
- ↑ 17.0 17.1 17.2 17.3 (25 October 2018) Criminalization Through Transinstitutionalization: A Critical Review of the Penrose Hypothesis in the Context of Compensation Imprisonment. Frontiers in Psychiatry 9: 534.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs named:3 - ↑ (December 2019) An assessment of awareness of mental health conditions and its association with socio-demographic characteristics: a cross-sectional study in a rural district in Bangladesh. BMC Health Services Research 19 (1): 562.
- ↑ Bangen, Hans: Geschichte der medikamentösen Therapie der Schizophrenie. Berlin 1992, Template:ISBN
- ↑ (1994)The Myth of the Reliability of DSM. Journal of Mind and Behavior 15 (1&2).
- ↑ Edward Shorter (2013) How Everyone Became Depressed: The Rise and Fall of the Nervous Breakdown, Oxford University Press Template:ISBN
- ↑ David Healy (2013) Pharmageddon, University of California Press Template:ISBN
- ↑ Peter Tyrer (2013) Models for Mental Disorder, Wiley-Blackwell Template:ISBN
- ↑ 25.0 25.1 25.2 U.S. Public Health Service (1999). "Overview of Mental Health Services", Mental Health: A Report of the Surgeon General.
- ↑ Dix, D (April 2006). 'I Tell What I Have Seen'—The Reports of Asylum Reformer Dorothea Dix. 1843. American Journal of Public Health 96 (4): 622–624.
- ↑ Luchins, AS (November 1989). Moral Treatment in Asylums and General Hospitals in 19th-Century America. The Journal of Psychology 123 (6): 585–607.
- ↑ Beers, Clifford Whittingham (8 April 2004). A Mind That Found Itself: An Autobiography. Project Gutenberg.
- ↑ (1983) The Mental Hygiene Movement, the Development of Personality and the School: The Medicalization of American Education. History of Education Quarterly 23 (2): 123–149.
- ↑ 30.0 30.1 30.2 (September 1991) The quiet success of the national plan for the chronically mentally ill. Hospital & Community Psychiatry 42 (9): 899–905.
- ↑ 31.0 31.1 Deinstitutionalization: A Psychiatric "Titanic". WGBH Educational Foundation (10 May 2005). Excerpts from (1997) Out of the Shadows: Confronting America's Mental Illness Crisis. New York: John Wiley & Sons. ISBN 978-0471161615.
- ↑ 32.0 32.1 Koyanagi, Chris (August 2007), Learning From History: Deinstitutionalization of People with Mental Illness As Precursor to Long-Term Care Reform, Menlo Park, CA: Kaiser Family Foundation
- ↑ 33.0 33.1 33.2 Mental disorders (October 2014).
- ↑ American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th, Arlington, VA: American Psychiatric Publishing, 101–05. ISBN 978-0-89042-555-8.
- ↑ (2000). Evolving Formulations: Sharing Complex Information with Clients. Behavioural and Cognitive Psychotherapy 28 (3): 307–10.
- ↑ HealthWise (2004) Mental Health Assessment. {{#invoke:webarchive|webarchive}} Yahoo! Health
- ↑ (May 1997) ABC of mental health. Mental health assessment. BMJ 314 (7093): 1536–9.
- ↑ (May 2003) Impact of structured clinical interviews on physicians' practices in community mental health settings. Psychiatric Services 54 (5): 712–8.
- ↑ (April 2000) Diagnosis of nonpsychotic patients in community clinics. The American Journal of Psychiatry 157 (4): 581–7.
- ↑ What is HoNOS?.
- ↑ Introduction to HoNOS.
- ↑ (November 2005) A review of the psychometric properties of the Health of the Nation Outcome Scales (HoNOS) family of measures. Health and Quality of Life Outcomes 3 (1): 76.
- ↑ (June 2001) Value of HoNOS in assessing patient change in NHS psychotherapy and psychological treatment services. The British Journal of Psychiatry 178 (6): 561–6.
- ↑ Caplan, Paula J., "Psychiatry's bible, the DSM, is doing more harm than good", 28 April 2012.
- ↑ (August 2013) The new crisis of confidence in psychiatric diagnosis. Annals of Internal Medicine 159 (3): 221–2.
- ↑ (2013) Mad Science: Psychiatric Coercion, Diagnosis, and Drugs. Transaction Publishers. Template:ISBN needed
- ↑ (April 2002) Selling sickness: the pharmaceutical industry and disease mongering. BMJ 324 (7342): 886–91.
- ↑ (July 2007) Age of onset of mental disorders: a review of recent literature. Current Opinion in Psychiatry 20 (4): 359–64.
- ↑ (December 2008) Why do many psychiatric disorders emerge during adolescence?. Nature Reviews. Neuroscience 9 (12): 947–57.
- ↑ (August 2009) Schizophrenia. Lancet 374 (9690): 635–45.
- ↑ (June 2001) Recovery from psychotic illness: a 15- and 25-year international follow-up study. The British Journal of Psychiatry 178 (6): 506–17.
- ↑ (December 2005) Long-term outcome of patients with schizophrenia: a review. Canadian Journal of Psychiatry 50 (14): 892–900.
- ↑ (December 2003)The McLean-Harvard First-Episode Mania Study: prediction of recovery and first recurrence. The American Journal of Psychiatry 160 (12): 2099–107.
- ↑ (July 2011) Grand challenges in global mental health. Nature 475 (7354): 27–30.
- ↑ Center for Psychiatric Rehabilitation What is Psychiatric Disability and Mental Illness? {{#invoke:webarchive|webarchive}} Boston University, Retrieved January 2012
- ↑ 56.0 56.1 (2005) A sociology of mental health and illness, 3rd, Milton Keynes: Open University Press. ISBN 978-0-335-21583-6. {{ safesubst:#invoke:Unsubst||date=__DATE__ |$B= }}
- ↑ Ferney, V. (2003) The Hierarchy of Mental Illness: Which diagnosis is the least debilitating? New York City Voices Jan/March
- ↑ (May 2008) Disability and treatment of specific mental and physical disorders across the world. The British Journal of Psychiatry 192 (5): 368–75.
- ↑ (June 2011) Global burden of disease in young people aged 10–24 years: a systematic analysis. Lancet 377 (9783): 2093–102.
- ↑ CIS: UN Body Takes On Rising Suicide Rates – Radio Free Europe / Radio Liberty 2006.
- ↑ (29 January 2000) Understanding suicidal behaviour. Leicester: BPS Books, 33–37. ISBN 978-1-85433-290-5.
- ↑ (October 2002) Suicide and psychiatric diagnosis: a worldwide perspective. World Psychiatry 1 (3): 181–5.
- ↑ (April 1999)Classifications in psychiatry: a conceptual history. The Australian and New Zealand Journal of Psychiatry 33 (2): 145–60.
- ↑ Perring, C. (2005) Mental Illness Stanford Encyclopedia of Philosophy
- ↑ (February 2010) Are psychiatrists an endangered species? Observations on internal and external challenges to the profession. World Psychiatry 9 (1): 21–8.
- ↑ (October 2011) A renovation of psychiatry is needed. World Psychiatry 10 (3): 198–9.
- ↑ Medicine's big new battleground: does mental illness really exist? (11 May 2013).
- ↑ NIMH » Mental Disorders as Brain Disorders: Thomas Insel at TEDxCaltech. U.S. Department of Health and Human Services (23 April 2013).
- ↑ (November 2016) Understanding comorbidity among internalizing problems: Integrating latent structural models of psychopathology and risk mechanisms. Development and Psychopathology 28 (4pt1): 987–1012.
- ↑ (March 2014) The p Factor: One General Psychopathology Factor in the Structure of Psychiatric Disorders?. Clinical Psychological Science 2 (2): 119–137.
- ↑ (November 2016) Beyond comorbidity: Toward a dimensional and hierarchical approach to understanding psychopathology across the life span. Development and Psychopathology 28 (4pt1): 971–986.
- ↑ (November 2016) Molecular genetic approaches to understanding the comorbidity of psychiatric disorders. Development and Psychopathology 28 (4pt1): 1089–1101.
- ↑ (February 2017) A hierarchical causal taxonomy of psychopathology across the life span. Psychological Bulletin 143 (2): 142–186.
- ↑ Mental disorders (9 April 2018).
- ↑ Mental disorders.
- ↑ Gazzaniga, M.S., & Heatherton, T.F. (2006). Psychological Science. New York: W.W. Norton & Company, Inc.{{ safesubst:#invoke:Unsubst||date=__DATE__ |$B= }}
- ↑ 77.0 77.1 77.2 Mental Health: Types of Mental Illness (1 July 2005).
- ↑ 78.0 78.1 (1999) "The Fundamentals of Mental Health and Mental Illness", Mental Health: A Report of the Surgeon General. National Institute of Mental Health, 26–50. ISBN 978-0-16-050300-9.
- ↑ NIMH (2005) Teacher's Guide: Information about Mental Illness and the Brain {{#invoke:webarchive|webarchive}} Curriculum supplement from The NIH Curriculum Supplements Series
- ↑ (May 2006) The DSM-IV and ICD-10 categories of recurrent [major] depressive and bipolar II disorders: evidence that they lie on a dimensional spectrum. Journal of Affective Disorders 92 (1): 45–54.
- ↑ McIntyre, Roger S. (7 March 2017). Mixed features and mixed states in psychiatry: from calculus to geometry. Cambridge University Press.
- ↑ (2007). Assessment and diagnosis of personality disorder: perennial issues and an emerging reconceptualization. Annual Review of Psychology 58 (1): 227–57.
- ↑ (July 2007)Comparison of alternative models for personality disorders. Psychological Medicine 37 (7): 983–94.
- ↑ Eating Disorders.
- ↑ NIMH » Eating Disorders.
- ↑ (March 2007)The spectra of neurasthenia and depression: course, stability and transitions. European Archives of Psychiatry and Clinical Neuroscience 257 (2): 120–7.
- ↑ (2002). Uncommon psychiatric syndromes, 4th edn. Journal of Neurology, Neurosurgery & Psychiatry 73 (2): 211–c.
- ↑ (July 2018)Preventive strategies for mental health. The Lancet. Psychiatry 5 (7): 591–604.
- ↑ 89.0 89.1 89.2 89.3 89.4 Risks To Mental Health: An Overview Of Vulnerabilities And Risk Factors (2012).
- ↑ (December 2000) A twin study of personality disorders. Comprehensive Psychiatry 41 (6): 416–25.
- ↑ (1 March 2010) The genetic epidemiology of personality disorders. Dialogues in Clinical Neuroscience 12 (1): 103–14.
- ↑ 92.0 92.1 (December 2007) Prevention of anxiety disorders. International Review of Psychiatry 19 (6): 647–54.
- ↑ (April 2009) Disruptive insights in psychiatry: transforming a clinical discipline. The Journal of Clinical Investigation 119 (4): 700–5.
- ↑ American Psychiatric Association 3 May 2013 Release Number 13-33
- ↑ (April 2016) Patterns of Nonrandom Mating Within and Across 11 Major Psychiatric Disorders. JAMA Psychiatry 73 (4): 354–61.
- ↑ (March 2007) Stress during development: Impact on neuroplasticity and relevance to psychopathology. Progress in Neurobiology 81 (4): 197–217.
- ↑ (June 1995) The social context of mental illness and violence. Journal of Health and Social Behavior 36 (2): 122–37.
- ↑ 98.0 98.1 (October 2005) Schizophrenia and urbanicity: a major environmental influence—conditional on genetic risk. Schizophrenia Bulletin 31 (4): 795–9.
- ↑ 99.0 99.1 (March 2015) Nutritional medicine as mainstream in psychiatry. The Lancet. Psychiatry 2 (3): 271–4.
- ↑ The Report. The Schizophrenia Commission (13 November 2012).
- ↑ (2009) "Table E-4 Risk Factors for Anxiety", Prevention of Mental Disorders, Substance Abuse, and Problem Behaviors: A Developmental Perspective. National Academies Press, 530–531. DOI:10.17226/12480. ISBN 978-0-309-12674-8.
- ↑ (2008). Prevention of bipolar disorder in at-risk children: theoretical assumptions and empirical foundations. Development and Psychopathology 20 (3): 881–97.
- ↑ 103.0 103.1 103.2 Cannabis and mental health.
- ↑ (March 2009) Tests of causal links between alcohol abuse or dependence and major depression. Archives of General Psychiatry 66 (3): 260–6.
- ↑ (October 2005) Neuropsychiatric effects of caffeine. Advances in Psychiatric Treatment 11 (6): 432–39.
- ↑ (August 2011)Caffeine challenge test and panic disorder: a systematic literature review. Expert Review of Neurotherapeutics 11 (8): 1185–95.
- ↑ (July 2007) Schizophrenia. BMJ 335 (7610): 91–5.
- ↑ (December 2009) Cannabis-induced bipolar disorder with psychotic features: a case report. Psychiatry 6 (12): 44–8.
- ↑ The Relationship between Mental Health, Mental Illness and Chronic Physical Conditions.
- ↑ (October 2016)Neuroticism's prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: a meta-analysis on 59 longitudinal/prospective studies with 443 313 participants. Psychological Medicine 46 (14): 2883–2906.
- ↑ 111.0 111.1 (July 2013) Neuroticism and common mental disorders: meaning and utility of a complex relationship. Clinical Psychology Review 33 (5): 686–697.
- ↑ (April 2012) The dappled nature of causes of psychiatric illness: replacing the organic-functional/hardware-software dichotomy with empirically based pluralism. Molecular Psychiatry 17 (4): 377–88.
- ↑ (2004) Prevention of mental disorders: effective interventions and policy options: summary report. Geneva: World Health Organization. ISBN 978-92-4-159215-4.
- ↑ (February 2012) European Psychiatric Association (EPA) guidance on prevention of mental disorders. European Psychiatry 27 (2): 68–80.
- ↑ Mental health promotion and mental illness prevention: The economic case. London School of Economics and Political Science (2 February 2011).
- ↑ NIMH » Research Priorities for Strategic Objective 3.
- ↑ (2009). Preventing child abuse and neglect with parent training: evidence and opportunities. The Future of Children 19 (2): 95–118.
- ↑ (December 2011) Parenting for mental health: what does the evidence say we need to do? Report of Workpackage 2 of the DataPrev project. Health Promotion International 26 (Suppl 1): i10-28.
- ↑ (2010). Prevention of major depression. Annual Review of Clinical Psychology 6: 181–212.
- ↑ (August 2003) Examining the effects of prevention programs on the incidence of new cases of mental disorders: the lack of statistical power. The American Journal of Psychiatry 160 (8): 1385–91.
- ↑ 121.0 121.1 (March 2017) Nutritional Psychiatry: Where to Next?. EBioMedicine 17 (17): 24–29.
- ↑ (March 2017) Compulsory community and involuntary outpatient treatment for people with severe mental disorders. The Cochrane Database of Systematic Reviews 3: CD004408.
- ↑ (November 2017) Nutritional psychiatry: the present state of the evidence. The Proceedings of the Nutrition Society 76 (4): 427–436.
- ↑ (January 2006)National estimates for mental health mutual support groups, self-help organizations, and consumer-operated services. Administration and Policy in Mental Health 33 (1): 92–103.
- ↑ The Joseph Rowntree Foundation (1998) The experiences of mental health service users as mental health professionals {{#invoke:webarchive|webarchive}}
- ↑ (2011). User/consumer involvement in mental health service delivery. Epidemiologia e Psichiatria Sociale 14 (1): 10–4.
- ↑ (December 2006) Beliefs about using consumer consultants in inpatient psychiatric units. International Journal of Mental Health Nursing 15 (4): 258–65.
- ↑ NIMH » Mental Health Medications.
- ↑ Mind Disorders Encyclopedia Psychosurgery [Retrieved on 5 August 2008]
- ↑ (June 2005) Psychosurgery: past, present, and future. Brain Research. Brain Research Reviews 48 (3): 409–19.
- ↑ (January 2008) Nutritional therapies for mental disorders. Nutrition Journal 7 (1): 2.
- ↑ (December 2019) Cannabinoids for the treatment of mental disorders and symptoms of mental disorders: a systematic review and meta-analysis. The Lancet. Psychiatry 6 (12): 995–1010.
- ↑ (February 2010) A systematic review: Students with mental health problems-A growing problem. International Journal of Nursing Practice 16 (1): 1–6.
- ↑ 134.0 134.1 134.2 (July 2010) Self-care and Well-being in Mental Health Professionals: The Mediating Effects of Self-awareness and Mindfulnes. Journal of Mental Health Counseling 32 (3): 247–264.
- ↑ (6 July 2017) Stigma towards Mental Health Problems during Childhood and Adolescence: Theory, Research and Intervention Approaches. Journal of Child and Family Studies 26 (11): 2949–2959.
- ↑ 136.0 136.1 136.2 Mental Health in America - Youth Data (in en).
- ↑ proof missing
- ↑ 138.0 138.1 138.2 138.3 (31 October 2014) Adolescent Mental Health—Opportunity and Obligation. Science 346 (6209): 547–549.
- ↑ (December 2013) Pragmatic Deficits and Social Impairment in Children with ADHD. Journal of Child Psychology and Psychiatry 54 (12): 1275–283.
- ↑ NIMH » Child and Adolescent Mental Health.
- ↑ 141.0 141.1 141.2 (July 2005) The Stigmatization of Mental Illness in Children and Parents: Developmental Issues, Family Concerns, and Research Needs.. Journal of Child Psychology and Psychiatry 46 (7): 714–34.
- ↑ (June 2003) Depictions of Mental Illnesses in Children's Media. Journal of Mental Health 12 (3): 249–58.
- ↑ (January 2008) Children's Understanding of Mental Illness: An Exploratory Study. Child: Care, Health and Development 34 (1): 10–18.
- ↑ The Tragedy of Mental Illness Stigma. Psychology Today.
- ↑ (2013) The Effect of Suicide-Related Internet Use on Users' Mental Health.. Crisis 34 (5): 348–353.
- ↑ from The Los Angeles Times, March 15, 2001.
- ↑ (1991). Homelessness as psychological trauma. Broadening perspectives. The American Psychologist 46 (11): 1219–1225.
- ↑ Interventions to Improve the Health of the HomelessA Systematic Review | Request PDF (in en).
- ↑ (November 1991) Homelessness as psychological trauma. Broadening perspectives.. The American Psychologist 46 (11): 1219–1225.
- ↑ Interventions to Improve the Health of the HomelessA Systematic Review | Request PDF (in en).
- ↑ (1 November 2005) Interventions to Improve the Health of the Homeless: A Systematic Review. American Journal of Preventive Medicine 29 (4): 311–311.e75.
- ↑ Weare, Katherine (2000). Promoting Mental, Emotional and Social Health: A Whole School Approach. London: RoutledgeFalmer. ISBN 978-0-415-16875-5.
- ↑ Office of the Deputy Prime Minister – Social Exclusion Unit: "Factsheet 1: Stigma and Discrimination on Mental Health Grounds". 2004.
- ↑ (2010) Mental Health Ethics: The Human Context. Routledge. ISBN 9781136881930.
- ↑ (26 September 2014) Experiences of Stigma and Discrimination among Caregivers of Persons with Schizophrenia in China: A Field Survey. PLOS ONE 9 (9).
- ↑ Royal College of Psychiatrists: Changing Minds.
- ↑ Erin Blakemore (29 April 2019). A play that hopes to smash the stigma surrounding mental illness.. The Washington Post.
- ↑ Rachael Myrow (2 May 2019). 'Manic Monologues' Seeks to Disrupt the Stigma Around Mental Illness.. KQED.
- ↑ NAMI Presents: Cure Stigma (in en).
- ↑ (2000) Handbook of Psychotherapy and Religious Diversity. Washington, DC: American Psychological Association. ISBN 978-1-55798-624-5.
- ↑ Religious Trauma Syndrome (in en-US).
- ↑ Jeff Sessions' new task force puts freedom of religion first (in en).
- ↑ How culture shapes your mind — and your mental illness - The Boston Globe.
- ↑ (2002). Incomprehensibility: the role of the concept in DSM-IV definition of schizophrenic delusions. Medicine, Health Care and Philosophy 5 (3): 291–5.
- ↑ (May 2001) Faith or delusion? At the crossroads of religion and psychosis. Journal of Psychiatric Practice 7 (3): 163–72.
- ↑ (2008). Enlightened or Delusional?: Differentiating Religious, Spiritual, and Transpersonal Experiences from Psychopathology. Journal of Humanistic Psychology 48 (4): 505–27.
- ↑ Clarke, Isabel (2010). Psychosis and Spirituality: Consolidating the New Paradigm. John Wiley & Sons, 240. ISBN 978-0-470-97029-4.
- ↑ 168.0 168.1 (March 2002) Religious delusions in patients admitted to hospital with schizophrenia. Social Psychiatry and Psychiatric Epidemiology 37 (3): 130–8.
- ↑ (1 June 2010) Delusions with religious content in patients with psychosis: how they interact with spiritual coping. Psychiatry 73 (2): 158–72.
- ↑ (1 April 2010) Phenomenology of delusions and hallucinations in schizophrenia by religious convictions. Mental Health, Religion & Culture 13 (3): 245–59.
- ↑ (November 2010)Evolution of spirituality and religiousness in chronic schizophrenia or schizo-affective disorders: a 3-years follow-up study. Social Psychiatry and Psychiatric Epidemiology 45 (11): 1095–103.
- ↑ 172.0 172.1 (2000). Adult psychopathology: issues and controversies. Annual Review of Psychology 51 (1): 377–404.
- ↑ Vedantam, Shankar, "Psychiatry's Missing Diagnosis: Patients' Diversity Is Often Discounted", The Washington Post, 26 June 2005.
- ↑ (1997). Triumph or pyrrhic victory? The inclusion of culture in DSM-IV. Harvard Review of Psychiatry 4 (6): 343–4.
- ↑ (1997) Troublesome Disguises: Underdiagnosed Psychiatric Syndromes. Blackwell Science. {{ safesubst:#invoke:Unsubst||date=__DATE__ |$B= }}
- ↑ (2006). The Role of Moral Judgment in Personality Disorder Diagnosis. Journal of Personality Disorders 20 (2): 184–85.
- ↑ (April 2005) Cultural differences in conceptual models of depression. Social Science & Medicine 60 (7): 1625–35.
- ↑ (2004). 'There are orphans in Africa still looking for my hands': African women refugees and the sources of emotional distress. Health Sociology Review 13: 54–64.
- ↑ (March 2001) Postpsychiatry: a new direction for mental health. BMJ 322 (7288): 724–7.
- ↑ (2000). Psychiatry and Postmodern Theory. Journal of Medical Humanities 21 (2): 71–84.
- ↑ (2005). The heresy of African-centered psychology. The Journal of Medical Humanities 26 (4): 215–35.
- ↑ (2007). Institutional racism in mental health services does not imply racism in individual psychiatrists: Commentary on... Institutional racism in psychiatry. Psychiatric Bulletin 31 (10): 367–68.
- ↑ 183.0 183.1 183.2 183.3 (2005) WHO Resource Book on Mental Health: Human rights and legislation. World Health Organization. ISBN 978-92-4-156282-9. {{ safesubst:#invoke:Unsubst||date=__DATE__ |$B= }}
- ↑ (June 2007) Starson v. Swayze: the Supreme Court speaks out (not all that clearly) on the question of "capacity". Canadian Journal of Psychiatry 52 (6): 390–6.
- ↑ Manitoba Family Services and Housing. The Vulnerable Persons Living with a Mental Disability Act, 1996Template:Psc
- ↑ ENABLE website UN section on disability
- ↑ (1999) "A Vision for the Future", Mental Health: A Report of the Surgeon General. National Institute of Mental Health, 451–58. ISBN 978-0-16-050300-9.
- ↑ Racial and Ethnic Minority Populations (24 September 2014).
- ↑ (December 2005) Stigma: barrier to mental health care among ethnic minorities. Issues in Mental Health Nursing 26 (10): 979–99.
- ↑ MedPartner Taiwan (22 May 2019). 別再說「想太多」!一張表看懂憂鬱症身心症狀 (in zh-tw).
- ↑ (September 2006) Mental illness and employment discrimination. Current Opinion in Psychiatry 19 (5): 522–6.
- ↑ Lucas, Clay. Stigma hurts job prospects. Sydney Morning Herald.
- ↑ Richard Spencer. "China relaxes laws on love and marriage", 21 August 2003.
- ↑ Stop Stigma. Bipolarworld-net.canadawebhosting.com (29 April 2002).
- ↑ (November 2006)Prejudice and schizophrenia: a review of the 'mental illness is an illness like any other' approach. Acta Psychiatrica Scandinavica 114 (5): 303–18.
- ↑ (October 2002) Depictions of mental illness in print media: a prospective national sample. The Australian and New Zealand Journal of Psychiatry 36 (5): 697–700.
- ↑ Edney, RD. (2004) Mass Media and Mental Illness: A Literature Review {{#invoke:webarchive|webarchive}} Canadian Mental Health Association
- ↑ (1997). The portrayal of mental illness on prime-time television. Journal of Community Psychology 25 (3): 289–302.
- ↑ (2003). Media frames of mental illnesses: The potential impact of negative frames. Journal of Mental Health 12 (3): 259–69.
- ↑ (2003). News Media Portrayal of Mental Illness: Implications for Public Policy. American Behavioral Scientist 46 (12): 1594–600.
- ↑ The Carter Center (18 July 2008). The Carter Center Awards 2008–2009 Rosalynn Carter Fellowships for Mental Health Journalism. Press release.
- ↑ The Rosalynn Carter Fellowships For Mental Health Journalism. The Carter Center (2013).
- ↑ Rosalynn Carter's Leadership in Mental Health (19 July 2016).
- ↑ (September 1999) Public conceptions of mental illness: labels, causes, dangerousness, and social distance. American Journal of Public Health 89 (9): 1328–33.
- ↑ (September 1999) The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. American Journal of Public Health 89 (9): 1339–45.
- ↑ (February 2009) The intricate link between violence and mental disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry 66 (2): 152–61.
- ↑ (February 2015) Mental illness, mass shootings, and the politics of American firearms. American Journal of Public Health 105 (2): 240–9.
- ↑ (October 2014)How often and how consistently do symptoms directly precede criminal behavior among offenders with mental illness?. Law and Human Behavior 38 (5): 439–49.
- ↑ (May 2015) Mental illness and reduction of gun violence and suicide: bringing epidemiologic research to policy. Annals of Epidemiology 25 (5): 366–76.
- ↑ 210.0 210.1 (June 2003) Violence and mental illness: an overview. World Psychiatry 2 (2): 121–4.
- ↑ (October 2001) Risks for individuals with schizophrenia who are living in the community. Psychiatric Services 52 (10): 1358–66.
- ↑ (August 2005) Crime victimization in adults with severe mental illness: comparison with the National Crime Victimization Survey. Archives of General Psychiatry 62 (8): 911–21.
- ↑ (2001). Crime Victims with Developmental Disabilities: A Review Essay. Criminal Justice and Behavior 28 (6): 655–94.
- ↑ (May 1998) Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Archives of General Psychiatry 55 (5): 393–401.
- ↑ 215.0 215.1 (August 2009) Schizophrenia and violence: systematic review and meta-analysis. PLOS Medicine 6 (8): e1000120.
- ↑ (January 1999) Homicides by people with mental illness: myth and reality. The British Journal of Psychiatry 174 (1): 9–14.
- ↑ (January 2005) Family violence among adults with severe mental illness: a neglected area of research. Trauma, Violence & Abuse 6 (1): 40–54.
- ↑ (December 2001) Assaultive behavior by psychiatric in-patients and its related factors. The Journal of Nursing Research 9 (5): 139–51.
- ↑ (August 2004) Schizophrenia, neighbourhood, and crime. Acta Psychiatrica Scandinavica 110 (2): 92–7.
- ↑ (2000). Cross-national comparisons of the prevalences and correlates of mental disorders. WHO International Consortium in Psychiatric Epidemiology. Bulletin of the World Health Organization 78 (4): 413–26.
- ↑ (June 2010) Mental Illness and Mental Health: The Two Continua Model Across the Lifespan. Journal of Adult Development 17 (2): 110–119.
- ↑ What is Mental Health and Mental Illness? | Workplace Mental Health Promotion.
ReferencesISBN links support NWE through referral fees
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. American Psychiatric Publishing, 2013. ISBN 978-0890425558
- Barlow, David H., Vincent Mark Durand, and Stefan G. Hofmann. Abnormal Psychology: An integrative approach. Cengage Learning, 2017. ISBN 978-1305950443
- Black, Jeremy, and Anthony Green. Gods, Demons and Symbols of Ancient Mesopotamia: An Illustrated Dictionary. University of Texas Press, 1992. ISBN 978-0292707948
- Bolton, Derek. What is Mental Disorder?: An Essay in Philosophy, Science, and Values. Oxford University Press, 2008. ISBN 978-0198565925
- Nemet-Nejat, Karen Rhea. Daily Life in Ancient Mesopotamia. Greenwood, 1998. ISBN 978-0313294976
- Wenzel, Amy E. The SAGE Encyclopedia of Abnormal and Clinical Psychology. SAGE Publications, Inc., 2017. ISBN 978-1483365831
- (2006) Private and Public Protection: Civil Mental Health Legislation. Edinburgh: Dunedin Academic Press. ISBN 978-1-903765-61-6.
- (2004) Discovering Psychology. Worth Publishers. ISBN 978-0-7167-5704-7.
- (1976) Paranoia: A Study in Diagnosis, Boston Studies in the Philosophy of Science. ISBN 978-90-277-0704-8. Template:Publisher missing
- (1983) Psychiatry as Medicine. The Hague: Nijhoff. ISBN 978-90-247-2837-4.
- ((National Academies of Sciences, Engineering, and Medicine)) (2016). Ending Discrimination Against People with Mental and Substance Use Disorders: The Evidence for Stigma Change. Washington, DC: National Academies Press. DOI:10.17226/23442. ISBN 978-0-309-43912-1.
- Porter, Roy (2002). Madness: a brief history. Oxford [Oxfordshire]: Oxford University Press. ISBN 978-0-19-280266-8.
- (1992) The Scientific Basis of Psychiatry. London: W.B. Saunders. Template:ISBN needed
- Wiencke, Markus (2006). "Schizophrenie als Ergebnis von Wechselwirkungen: Georg Simmels Individualitätskonzept in der Klinischen Psychologie", Georg Simmel in Translation: Interdisciplinary Border-Crossings in Culture and Modernity. Cambridge: Cambridge Scholars Press, 123–55. ISBN 978-1-84718-060-5.
- Radden, Jennifer. (20 February 2019). "Mental Disorder (Illness)". Stanford Encyclopedia of Philosophy.
- (2018) Management of physical health conditions in adults with severe mental disorders. WHO. ISBN 978-92-4-155038-3.
External links
All links retrieved
- National Institute of Mental Health
- International Committee of Women Leaders on Mental Health The Carter Center
- Mental Health Conditions National Alliance on Mental Illness (NAMI)
- What Is Mental Illness? American Psychiatric Association
- Mental Disorders MedLine Plus
- Types of Mental Illness WebMD
- Learn About Mental Health Centers for Disease Control and Prevention (CDC)
| ||||||||||||||||||||||||||||||||
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.



