- "Drug abuse" redirects here.
| Substance abuse | |

| |
| Other names | Drug abuse, substance use disorder, substance misuse disorder |
|---|---|
| Complications | Drug overdose |
Substance abuse, also known as Substance use disorder (SUD), and formerly as drug abuse, is use of a drug in amounts or by methods which are harmful to the individual or others. It is a form of substance-related disorder. Differing definitions of drug abuse are used in public health, medical, and criminal justice contexts. In some cases criminal or anti-social behavior occurs when the person is under the influence of a drug, and long term personality changes in individuals may occur as well. In addition to possible physical, social, and psychological harm, use of some drugs may also lead to criminal penalties, although these vary widely depending on the local jurisdiction. Those suffering from SUD are in danger of overdose, which may be life threatening.
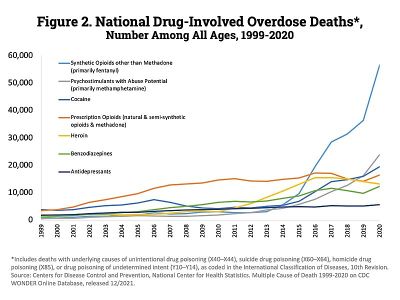
Drugs most often associated with this term include: alcohol, amphetamines, barbiturates, benzodiazepines, cannabis, cocaine, hallucinogens, methaqualone, and opioids. Rates of substance use disorders vary by nation and by substance, but the overall prevalence is high. The cost to society of the impact of SUD on such large numbers of the population is not only economic, but more importantly, is destructive to the individuals, their families, and the social well-being of society as a whole.
Definitions
Differing definitions are used in public health, medical, and criminal justice contexts. Generally the term "drug abuse" is no longer employed for a variety of reasons, one being that what constitutes a "drug" is debatable.
Medical definitions
| Addiction and dependence glossary | |
* addiction – a biopsychosocial disorder characterized by compulsively seeking to achieve a desired effect, such as intoxication, despite harm and adverse consequences to self and others
|
Today, the term "drug abuse" is no longer a current medical diagnosis in either of the most used diagnostic tools in the world, the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM), and the World Health Organization's International Statistical Classification of Diseases (ICD). "Substance abuse disorder" is now the preferred term. Following is a brief history of the various terms used in medical diagnosis.
The first edition of the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (published in 1952) grouped alcohol and other drug abuse under "Sociopathic Personality Disturbances," which were thought to be symptoms of deeper psychological disorders or moral weakness. The third edition, published in 1980, was the first to recognize substance abuse (including drug abuse) and substance dependence as conditions separate from substance abuse alone, bringing in social and cultural factors. The definition of dependence emphasized tolerance to drugs, and withdrawal from them as key components to diagnosis, whereas abuse was defined as "problematic use with social or occupational impairment" but without withdrawal or tolerance.[1]
In 1987, the DSM-III-R category "psychoactive substance abuse," which included former concepts of drug abuse was defined as "a maladaptive pattern of use indicated by...continued use despite knowledge of having a persistent or recurrent social, occupational, psychological or physical problem that is caused or exacerbated by the use (or by) recurrent use in situations in which it is physically hazardous." It was the first definition to give equal weight to behavioral and physiological factors in diagnosis.
In 1994, the DSM-IV defined substance dependence as "a syndrome involving compulsive use, with or without tolerance and withdrawal"; whereas substance abuse was defined as "problematic use without compulsive use, significant tolerance, or withdrawal."[2] By 2000, the DSM-IV-TR defined substance dependence as "when an individual persists in use of alcohol or other drugs despite problems related to use of the substance, substance dependence may be diagnosed."[3] The following criteria were given for diagnosis of substance abuse:
- A. A maladaptive pattern of substance use leading to clinically significant impairment or distress, as manifested by one (or more) of the following, occurring within a 12-month period:
- Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home (e.g., repeated absences or poor work performance related to substance use; substance-related absences, suspensions or expulsions from school; neglect of children or household)
- Recurrent substance use in situations in which it is physically hazardous (e.g., driving an automobile or operating a machine when impaired by substance use)
- Recurrent substance-related legal problems (e.g., arrests for substance-related disorderly conduct)
- Continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance (e.g., arguments with spouse about consequences of intoxication, physical fights)
- B. The symptoms have never met the criteria for Substance Dependence for this class of substance.
When the fifth edition of the DSM (DSM-5), was released in 2013, it revisited this terminology. The principal change was a transition from the abuse/dependence terminology. In the DSM-IV era, abuse was seen as an early, or less hazardous, form of the disease characterized with the dependence criteria. However, this distinction often led to confusion, both within the medical community and with the general public. In the DSM-5, substance abuse and substance dependence have been merged into the category of substance use disorders and they no longer exist as individual concepts.[4]
While substance abuse and dependence were either present or not, substance use disorder has three levels of severity: mild, moderate, and severe.
Public health definitions
Public health practitioners have attempted to look at substance use from a broader perspective than the individual, emphasizing the role of society, culture, and availability. Some health professionals choose to avoid the terms alcohol or drug "abuse" in favor of language they consider more objective, such as "substance and alcohol type problems" or "harmful/problematic use" of drugs.
For example, the Health Officers Council of British Columbia — in their 2005 policy discussion paper, A Public Health Approach to Drug Control in Canada — adopted a public health model of psychoactive substance use that challenges the simplistic black-and-white construction of the binary (or complementary) antonyms "use" vs. "abuse." This model explicitly recognizes a spectrum of use, ranging from beneficial use to chronic dependence, and recommends changing the view of individual harmful illegal drug use from being primarily a criminal issue to being primarily a health issue.[5]
Drug misuse
"Drug misuse" is a term used commonly when prescription medication with sedative, anxiolytic, analgesic, or stimulant properties are used for mood alteration or intoxication, ignoring the fact that overdose of such medicines can sometimes have serious adverse effects. It sometimes involves drug diversion from the individual for whom it was prescribed.
Prescription misuse has been defined differently and rather inconsistently based on the status of drug prescription, the uses without a prescription, intentional use to achieve intoxicating effects, route of administration, co-ingestion with alcohol, and the presence or absence of dependence symptoms. Chronic use of certain substances leads to a change in the central nervous system known as a 'tolerance' to the medicine such that more of the substance is needed in order to produce desired effects. With some substances, stopping or reducing use can cause withdrawal symptoms to occur, but this is highly dependent on the specific substance in question.[6]
Avenues of obtaining prescription drugs for misuse are varied: sharing between family and friends, illegally buying medications at school or work, and often "doctor shopping" to find multiple physicians to prescribe the same medication, without knowledge of other prescribers. Increasingly, law enforcement is holding physicians responsible for prescribing controlled substances without fully establishing patient controls, such as a patient "drug contract." Concerned physicians are educating themselves on how to identify medication-seeking behavior in their patients, and are becoming familiar with "red flags" that would alert them to potential prescription drug abuse.[7]
Issues
As already noted, medical diagnoses no longer use the term "drug abuse," preferring instead "substance use disorder." Indeed, what constitutes a "drug" is debatable. For instance, GHB, a naturally occurring substance in the central nervous system, is considered a drug and is illegal in many countries, while nicotine is not officially considered a drug in most countries.
In the U.S., drugs have been legally classified into five categories, schedule I, II, III, IV, or V in the Controlled Substances Act, based on their deemed potential for abuse. Usage of some drugs is strongly correlated. For example, the consumption of seven illicit drugs (amphetamines, cannabis, cocaine, ecstasy, legal highs, LSD, and magic mushrooms) is correlated.[8]
Additionally, the word "abuse" implies a recognized standard of use for any substance. Drinking an occasional glass of wine is considered acceptable in most Western countries, while drinking several bottles is seen as an abuse. Strict temperance advocates, who may or may not be religiously motivated, would see drinking even one glass as an abuse. Some groups even condemn caffeine use in any quantity. Similarly, adopting the view that any (recreational) use of cannabis or substituted amphetamines constitutes drug abuse implies a decision made that the substance is harmful, even in minute quantities.[9]
The current preferred term, "substance use disorder" (SUD), avoids these problems.
Diagnosis
Individuals whose drug or alcohol use cause significant impairment or distress may have a substance use disorder (SUD). Diagnosis usually involves an in-depth examination, typically by psychiatrist, psychologist, or drug and alcohol counselor.
The most commonly used guidelines are published in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which lists 11 diagnostic criteria which can be broadly categorized into issues arising from substance use related to loss of control, strain to one's interpersonal life, hazardous use, and pharmacologic effects. Diagnosis of a substance use disorder require that the individual have significant impairment or distress from their pattern of drug use, and satisfies at least two of these 11 criteria in a given year.[4]
- Using more of a substance than planned, or using a substance for a longer interval than desired
- Inability to cut down despite desire to do so
- Spending substantial amount of the day obtaining, using, or recovering from substance use
- Cravings or intense urges to use
- Repeated usage causes or contributes to an inability to meet important social, or professional obligations
- Persistent usage despite user's knowledge that it is causing frequent problems at work, school, or home
- Giving up or cutting back on important social, professional, or leisure activities because of use
- Using in physically hazardous situations, or usage causing physical or mental harm
- Persistent use despite the user's awareness that the substance is causing or at least worsening a physical or mental problem
- Tolerance: needing to use increasing amounts of a substance to obtain its desired effects
- Withdrawal: characteristic group of physical effects or symptoms that emerge as amount of substance in the body decreases
There are additional qualifiers and exceptions outlined in the DSM. For instance, if an individual is taking opiates as prescribed, they may experience physiologic effects of tolerance and withdrawal, but this would not cause an individual to meet criteria for a SUD without additional symptoms also being present.[4] A physician trained to evaluate and treat substance use disorders will take these nuances into account during a diagnostic evaluation.
Severity
Substance use disorders can range widely in severity, and there are numerous methods to monitor and qualify the severity of an individual's SUD. The DSM-5 includes specifiers for severity of a SUD. Individuals who meet only 2 or 3 criteria are often deemed to have mild SUD. Substance users who meet 4 or 5 criteria may have their SUD described as moderate, and persons meeting 6 or more criteria as severe.[4]
The quantity of criteria met offer a rough gauge on the severity of illness, but licensed professionals will also take into account a more holistic view when assessing severity which includes specific consequences and behavioral patterns related to an individual's substance use. They will also typically follow frequency of use over time, and assess for substance-specific consequences, such as the occurrence of blackouts, or arrests for driving under the influence of alcohol, when evaluating someone for an alcohol use disorder. There are additional qualifiers for stages of remission that are based on the amount of time an individual with a diagnosis of a SUD has not met any of the 11 criteria except craving.[4]
Screening tools
There are several different screening tools that have been validated for use with adolescents, such as the CRAFFT,[10] and with adults, such as CAGE, AUDIT and DALI.[11]
Laboratory tests to detect alcohol and other drugs in urine and blood may be useful during the assessment process to confirm a diagnosis, to establish a baseline, and later, to monitor progress. However, since these tests measure recent substance use rather than chronic use or dependence, they are not recommended as screening tools.[12]
Dual diagnosis
The terms “dual diagnosis” or “co-occurring disorders,” refer to having a mental health and substance use disorder at the same time, and it is common for individuals with SUDs to have other psychological problems.[13] According to the British Association for Psychopharmacology (BAP), “symptoms of psychiatric disorders such as depression, anxiety and psychosis are the rule rather than the exception in patients misusing drugs and/or alcohol.”[14] Integration of mental health and addiction services generally lead to better outcomes for clients with co-occurring disorders than when treatment services are separate.
Signs and symptoms
The symptoms of substance use disorder (SUD) include physical and psychological changes, dependent on which substance is being abused. In some cases, criminal or anti-social behavior occurs when the person is under the influence of a drug. Long term personality changes in individuals may also occur.[15] In addition to possible physical, social, and psychological harm, use of certain drugs may lead to criminal penalties, depending on the local jurisdiction.
One symptom that abusers of any substance will experience are unpleasant withdrawal symptoms if the drug is taken away from them.[16][17]
Common symptoms of SUD include:
- Sudden changes in behavior – may engage in secretive or suspicious behavior
- Mood changes – anger towards others, paranoia, and little care shown about themselves or their future
- Problems with work or school – lack of attendance
- Changes in eating and sleeping habits
- Changes in friendship groups and poor family relationships
- A sudden unexplained change in financial needs – leading to borrowing/stealing money
Depending on the actual compound, substance abuse may lead to health problems, social problems, morbidity, injuries, unprotected sex, violence, deaths, motor vehicle accidents, homicides, suicides, physical dependence, or psychological addiction.[18]
Substance abuse, including alcohol and prescription drugs, can induce symptomatology which resembles mental illness. This can occur both in the intoxicated state and also during the withdrawal state. In some cases these substance induced psychiatric disorders can persist long after detoxification, such as prolonged psychosis or depression after amphetamine or cocaine abuse. A protracted withdrawal syndrome can also occur with symptoms persisting for months after cessation of use. Benzodiazepines are the most notable drug for inducing prolonged withdrawal effects with symptoms sometimes persisting for years after cessation of use. Both alcohol, barbiturate as well as benzodiazepine withdrawal can potentially be fatal. Abuse of hallucinogens can trigger delusional and other psychotic phenomena long after cessation of use.
Cannabis may trigger anxiety reactions and panic attacks during intoxication.[19] Researchers have found that cannabis use is associated with an earlier diagnosis schizophrenia and other psychotic disorders, as well as making schizophrenia and psychosis symptoms worse and increasing numbers relapses and hospitalizations.[20]
Severe anxiety and depression are commonly induced by sustained alcohol abuse, which in most cases abates with prolonged abstinence. Even sustained moderate alcohol use may increase anxiety and depression levels in some individuals. In most cases these drug induced psychiatric disorders fade away with prolonged abstinence.[21]
There is a high rate of suicide in alcoholics and other drug abusers. Suicide is also very common in adolescent alcohol abusers, with one in four suicides in adolescents being related to alcohol abuse.[22] Alcohol abuse is also associated with increased risks of committing criminal offenses including child abuse, domestic violence, rapes, burglaries and assaults.[23]
Treatment
Treatment for substance abuse disorder is not simple. Rather than a single treatment, a variety of different approaches are required for success:
In order to be effective, all pharmacological or biologically based treatments for addiction need to be integrated into other established forms of addiction rehabilitation, such as cognitive behavioral therapy, individual and group psychotherapy, behavior-modification strategies, twelve-step programs, and residential treatment facilities.[24]
Depending on the severity of use, and the given substance, early treatment of acute withdrawal may include medical detoxification prior to any other form of treatment.
Alcoholics Anonymous[25] and Narcotics Anonymous[26] are the most widely known self-help organizations in which members support each other not to use alcohol or drugs respectively. These organizations provide the support of a recovering community who use the "Twelve-Step program" to overcome addiction. Beyond the support of people who have common experience and success with the program, there is also the spiritual component of accepting the presence and help of a "higher power" in their lives.
Medication
Certain medications can be useful in treating severe substance use disorders, as drug substitutes or to lessen withdrawal symptoms. In the United States, several medications, such as disulfiram and methadone, are approved to treat alcohol and opioid use disorders.[27] There are no approved medications for cocaine, methamphetamine, or other substance use disorders.
Approved medications can be used as part of broader treatment plans to help a patient function comfortably without illicit opioids or alcohol.[28] Medication-assisted treatment (MAT) refers to such combinations of behavioral interventions and medications to treat substance use disorders. Evidence has demonstrated the efficacy of MAT at reducing illicit drug use and overdose deaths, improving retention in treatment, and reducing HIV transmission.[29]
Psychological interventions
Therapeutic treatments usually involve planning for specific ways to avoid the addictive stimulus, and therapeutic interventions intended to help a client learn healthier ways to find satisfaction. Therapists attempt to tailor intervention approaches to specific influences that affect addictive behavior, using therapeutic interviews in an effort to discover factors that led a person to embrace unhealthy, addictive sources of pleasure or relief from pain.
A meta-analytic review on the efficacy of various behavioral therapies for treating drug and behavioral addictions found that cognitive behavioral therapy (such as relapse prevention and contingency management), motivational interviewing, and a community reinforcement approach were effective interventions with moderate effect sizes.[30]
Clinical and preclinical evidence indicate that consistent aerobic exercise, especially endurance exercise (such as marathon running), actually prevents the development of certain drug addictions and is an effective adjunct treatment for drug addiction, and for psychostimulant addiction in particular.[31][32] Consistent aerobic exercise reduces drug addiction risk, decreases drug self-administration, reduces the likelihood of relapse, and induces opposite effects on striatal dopamine receptor D2 (DRD2) signaling (increased DRD2 density) to those induced by addictions to several drug classes (decreased DRD2 density). Consequently, consistent aerobic exercise may lead to better treatment outcomes when used as an adjunct treatment for drug addiction.[31][32]
Causes
The causes of SUDs can be categorized according to social, psychological, and biological factors. However, it is important to bear in mind that these categories are used by scientists partly for convenience; the categories often overlap (for example, adolescents and adults whose parents had (or have) an alcohol use disorder display higher rates of alcohol problems, a phenomenon that can be due to genetic, observational learning, socioeconomic, and other causal factors). Most researchers in this and related areas (such as the etiology of psychopathology generally), emphasize that various causal factors interact and influence each other in complex and multifaceted ways.[33]
Social determinants
Among older adults, being divorced, separated, or single; having more financial resources; lack of religious affiliation; bereavement; involuntary retirement; and homelessness are all associated with alcohol problems, including alcohol use disorder.
Psychological determinants
Psychological causal factors include cognitive, affective, and developmental determinants, among others. For example, individuals who begin using alcohol or other drugs in their teens are more likely to have a substance use disorder as adults. Other common risk factors are being male, being under 25, having other mental health problems, and lack of familial support and supervision.[34] Some of these causal factors can also be categorized as social or biological.
Other psychological risk factors include high impulsivity, sensation seeking, neuroticism, and openness to experience in combination with low conscientiousness.[21]
Biological determinants
Children born to parents with SUDs have roughly a two-fold increased risk in developing a SUD compared to children born to parents without any SUDs.[34]
Epidemiology
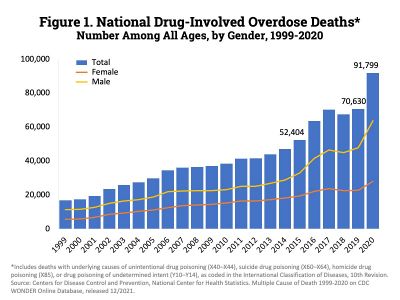
Rates of substance use disorders vary by nation and by substance, but the overall prevalence is high. On a global level, men are affected at a much higher rate than women. Younger individuals are also more likely to be affected than older adults.[36]
The initiation of drug use including alcohol is most likely to occur during adolescence, and some experimentation with substances by older adolescents is common. However, the large majority of adolescents will phase out of drug use before it becomes problematic.
Legislation
Most governments have designed legislation to criminalize certain types of drug use. These drugs are often called "illegal drugs" but generally what is illegal is their unlicensed production, distribution, and possession. These drugs are also called "controlled substances." Laws vary across countries, and even within them, and have fluctuated widely throughout history. Even for simple possession, legal punishment can be quite severe, including the death penalty in some countries.
Attempts by government-sponsored drug control policy to interdict drug supply and eliminate drug abuse have been largely unsuccessful. Despite drug legislation (or perhaps because of it), large, organized criminal drug cartels operate worldwide. Advocates of decriminalization argue that drug prohibition makes drug dealing a lucrative business, leading to much of the associated criminal activity.
Notes
- ↑ American Psychiatric Association, DSM-III: Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition (American Psychiatric Association, 1980, ISBN 978-0521315289).
- ↑ American Psychiatric Association, DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (American Psychiatric Association, 1994, ISBN 978-0890420621).
- ↑ American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR) (American Psychiatric Association, 2000, ISBN 978-0890420256).
- ↑ 4.0 4.1 4.2 4.3 4.4 American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5 (American Psychiatric Association, 2013, ISBN 978-0890425541).
- ↑ A Public Health Approach To Drug Control in Canada Health Officers Council of British Columbia, October 2005. Retrieved October 10, 2022.
- ↑ Deborah Antai-Otong, Psychiatric Nursing: Biological and Behavioral Concepts (Delmar Cengage Learning, 2000, ISBN 978-1418038724).
- ↑ How can prescription drug misuse be prevented? Misuse of Prescription Drugs Research Report, National Institute on Drug Abuse, June 2020. Retrieved October 10, 2022.
- ↑ Elaine Fehrman, Vincent Egan, Alexander N. Gorban, Jeremy Levesley, Evgeny M. Mirkes, and Awaz K. Muhammad, Personality Traits and Drug Consumption. A Story Told by Data (Springer, 2019, ISBN 978-3030104412).
- ↑ Philip Jenkins, Synthetic Panics: The Symbolic Politics of Designer Drugs (NYU Press, 1999, ISBN 978-0814742433).
- ↑ John R. Knight, Lon Sherritt, Lydia A. Shrier, Sion Kim Harris, and Grace Chang, Validity of the CRAFFT Substance Abuse Screening Test Among Adolescent Clinic Patients Arch Pediatr Adolesc Med. 156(6) (2002):607-614. Retrieved October 10, 2022.
- ↑ Martin M. Antony and David H. Barlow (eds.), Handbook of Assessment and Treatment Planning for Psychological Disorders, Third Edition (The Guilford Press, 2020, ISBN 978-1462544882).
- ↑ Center for Substance Abuse Treatment, Chapter 2—Screening for Substance Use Disorders A Guide to Substance Abuse Services for Primary Care Clinicians (Rockville, MD: Substance Abuse and Mental Health Services Administration, 1997). Retrieved October 10, 2022.
- ↑ A.R. Lingford-Hughes, S. Welch, L. Peters, and D.J. Nutt, BAP updated guidelines: evidence-based guidelines for the pharmacological management of substance abuse, harmful use, addiction and comorbidity: recommendations from BAP Journal of Psychopharmacology 26(7) (July 2012):899-952. Retrieved October 10, 2022.
- ↑ Ashley L Peterson, Integrating mental health and addictions services to improve client outcomes Issues in Mental Health Nursing 34(10) (October 2013): 752–756. Retrieved October 10, 2022.
- ↑ Carl Hart and Charles Ksir, Drugs, Society, and Human Behavior (McGraw-Hill Education, 2017, ISBN 978-1259913860).
- ↑ Paula Spencer Scott, Signs of Drug Addiction WebMD. Retrieved October 10, 2022.
- ↑ Drug Abuse and Addiction HelpGuide. Retrieved October 10, 2022.
- ↑ P. Burke, J. O'Sullivan, and B.L. Vaughan, Adolescent substance use: brief interventions by emergency care providers Pediatric Emergency Care 21(11) (November 2005): 770–776. Retrieved October 10, 2022.
- ↑ José Alexandre Crippa, Antonio Waldo Zuardi, Rocio Martín-Santos, Sagnik Bhattacharyya, Zerrin Atakan, Philip McGuire, and Paolo Fusar-Poli, Cannabis and anxiety: a critical review of the evidence Hum Psychopharmacol 24(7) October, 2009]: 515-523. Retrieved October 10, 2022.
- ↑ Shweta Patel, Sahar Khan, M. Saipavankumar, and Pousettef Hamid, The Association Between Cannabis Use and Schizophrenia: Causative or Curative? A Systematic Review Cureus 12(7) (July 2020): e9309. Retrieved October 10, 2022.
- ↑ 21.0 21.1 Katie Evans and Michael J. Sullivan, Dual Diagnosis: Counseling the Mentally Ill Substance Abuser (The Guilford Press, 2000, ISBN 978-1572304468).
- ↑ Rory C. O'Connor and Noel Sheehy, Understanding Suicidal Behaviour (Wiley, 2000, ISBN 978-1854332905).
- ↑ Richard Isralowitz, Drug Use: A Reference Handbook (ABC-CLIO, 2004, ISBN 978-1576077085).
- ↑ Sara B. Taylor, Candace R. Lewis, and M. Foster Olive, The neurocircuitry of illicit psychostimulant addiction: acute and chronic effects in humans Subst. Abuse Rehabil. 4 (2013): 29–43. Retrieved October 10, 2022.
- ↑ Alcoholics Anonymous Retrieved October 10, 2022.
- ↑ Narcotics Anonymous Retrieved October 10, 2022.
- ↑ American Psychiatric Association, Practice Guidelines for the Treatment of Psychiatric Disorders (American Psychiatric Publishing, 2006, ISBN 978-0890423851).
- ↑ Antoine B. Douaihy, Thomas M. Kelly, and Carl Sullivan, Medications for Substance Use Disorders Soc Work Public Health 28(0) (2013): 264–278. Retrieved October 10, 2022.
- ↑ Office of the Surgeon General, Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health (CreateSpace, 2017, ISBN 978-1974580620).
- ↑ M. Walter, et al., Psychosocial Treatment of Addictive Disorders – An Overview of Psychotherapeutic Options and their Efficacy Fortschr Neurol Psychiatr 83(4) (2015):201–210. Retrieved October 10, 2022.
- ↑ 31.0 31.1 Christopher M. Olsen, Natural Rewards, Neuroplasticity, and Non-Drug Addictions Neuropharmacology 61(7) (2011): 1109–1122. Retrieved October 10, 2022.
- ↑ 32.0 32.1 Wendy J. Lynch, Alexis B. Peterson, Victoria Sanchez, Jean Abel, and Mark A. Smith, Exercise as a Novel Treatment for Drug Addiction: A Neurobiological and Stage-Dependent Hypothesis Neurosci Biobehav Rev 37(8) (2013):1622–1644. Retrieved October 10, 2022.
- ↑ James MacKillop, George A. Kenna, Lorenzo Leggio, and Lara A. Ray (eds.), Integrating Psychological and Pharmacological Treatments for Addictive Disorders (Routledge, 2017, ISBN 978-1138919105).
- ↑ 34.0 34.1 Fred F. Ferri, Ferri's Clinical Advisor (Elsevier, 2020, ISBN 978-0323713337).
- ↑ 35.0 35.1 Overdose Death Rates. By National Institute on Drug Abuse (NIDA). Retrieved November 29, 2022.
- ↑ Marc Galanter, Herbert D. Kleber, and Kathleen T. Brady (eds.), The American Psychiatric Publishing Textbook of Substance Abuse Treatment (American Psychiatric Publishing, 2014, ISBN 978-1585624720).
ReferencesISBN links support NWE through referral fees
- American Psychiatric Association. DSM-III: Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition. American Psychiatric Association, 1980. ISBN 978-0521315289
- American Psychiatric Association. DSM-IV: Diagnostic and Statistical Manual of Mental Disorders, 4th Edition. American Psychiatric Association, 1994. ISBN 978-0890420621
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision (DSM-IV-TR). American Psychiatric Association, 2000. ISBN 978-0890420256
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. American Psychiatric Association, 2013. ISBN 978-0890425541
- American Psychiatric Association. Practice Guidelines for the Treatment of Psychiatric Disorders. American Psychiatric Publishing, 2006. ISBN 978-0890423851
- Antai-Otong, Deborah. Psychiatric Nursing: Biological and Behavioral Concepts. Delmar Cengage Learning, 2000. ISBN 978-1418038724
- Antony, Martin M., and David H. Barlow (eds.). Handbook of Assessment and Treatment Planning for Psychological Disorders, Third Edition. The Guilford Press, 2020. ISBN 978-1462544882
- Evans, Katie, and Michael J. Sullivan. Dual Diagnosis: Counseling the Mentally Ill Substance Abuser. The Guilford Press, 2000. ISBN 978-1572304468
- Fehrman, Elaine, Vincent Egan, Alexander N. Gorban, Jeremy Levesley, Evgeny M. Mirkes, and Awaz K. Muhammad. Personality Traits and Drug Consumption. A Story Told by Data. Springer, 2019. ISBN 978-3030104412
- Ferri, Fred F. Ferri's Clinical Advisor. Elsevier, 2020. ISBN 978-0323713337
- Galanter, Marc, Herbert D. Kleber, and Kathleen T. Brady (eds.). The American Psychiatric Publishing Textbook of Substance Abuse Treatment. American Psychiatric Publishing, 2014. ISBN 978-1585624720
- Hart, Carl, and Charles Ksir. Drugs, Society, and Human Behavior. McGraw-Hill Education, 2017. ISBN 978-1259913860
- Isralowitz, Richard. Drug Use: A Reference Handbook. ABC-CLIO, 2004. ISBN 978-1576077085
- Jenkins, Philip. Synthetic Panics: The Symbolic Politics of Designer Drugs. NYU Press, 1999. ISBN 978-0814742433
- MacKillop, James, George A. Kenna, Lorenzo Leggio, and Lara A. Ray (eds.). Integrating Psychological and Pharmacological Treatments for Addictive Disorders. Routledge, 2017. ISBN 978-1138919105
- Office of the Surgeon General. Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health. CreateSpace, 2017. ISBN 978-1974580620
- O'Connor, Rory C., and Noel Sheehy. Understanding Suicidal Behaviour. Wiley, 2000. ISBN 978-1854332905
- O'Toole, Marie T. (ed). Mosby's Dictionary of Medicine, Nursing & Health Professions. Elsevier, 2016. ISBN 978-0323222051
External links
All links retrieved February 26, 2023.
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- The National Institute on Drug Abuse
- Preventing Addiction: The Importance of Drug Prevention Southern California Sunrise Recovery Center
- How To Help Prevent And Treat Substance Abuse No Matter What Recovery
- The Danger of Underage Marijuana Use Wellness Retreat Recovery Center
- Understanding Co-Occurring Disorders Everlast Recovery Centers
- Medication-Assisted Treatment in Colorado Healing Pines Recovery
- Drug Rehab in Encinitas, CA Akasha Recovery
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.

