| Autism spectrum disorder | |

| |
| Other names |
|
|---|---|
| Repetitively stacking or lining up objects is a common trait associated with autism. | |
| Symptoms | Difficulties in social interaction, verbal and nonverbal communication, and the presence of repetitive behavior or restricted interests |
| Complications | Social isolation, educational and employment problems, anxiety, stress, bullying, depression, self-harm |
| Usual onset | Early childhood |
| Duration | Lifelong |
| Causes | Multifactorial, with many uncertain factors |
| Risk factors | Family history, certain genetic conditions, having older parents, certain prescribed drugs, perinatal and neonatal health issues |
| Diagnostic method | Based on combination of clinical observation of behavior and development and comprehensive diagnostic testing completed by a team of qualified professionals (including psychiatrists, clinical psychologists, neuropsychologists, pediatricians, and speech-language pathologists). For adults, the use of a patient's written and oral history of autistic traits becomes more important |
| Differential diagnosis | Intellectual disability, anxiety, bipolar disorder, depression, Rett syndrome, attention deficit hyperactivity disorder, schizoid personality disorder, selective mutism, schizophrenia, obsessive‚Äďcompulsive disorder, social anxiety disorder, Einstein syndrome, PTSD, learning disorders (mainly speech disorders) |
| Management | Applied behavior analysis, cognitive behavioral therapy, occupational therapy, psychotropic medication, speech‚Äďlanguage pathology |
| Frequency | Estimated 1 in 100 children (1%) worldwide[1] |
Autism, formally called autism spectrum disorder (ASD) or autism spectrum condition (ASC), is a neurodevelopmental disorder characterized by deficits in social communication and social interaction, and repetitive or restricted patterns of behaviors, interests, or activities, which can include hyper- and hyporeactivity to sensory input. Autism is clinically regarded as a spectrum disorder, meaning that it can manifest very differently in each person. Because of this, there is wide variation in the support needs of people across the autism spectrum.
With autism now known to be a lifelong, unpreventable condition, many forms of therapy, such as speech and occupational therapy, have been developed that may help autistic people. Some therapies have been shown to improve certain symptoms of autism, such as socialization, communication, expressive language, intellectual functioning, language development, and acquisition of daily living skills.
The understanding of autism has been shaped by cultural, scientific, and societal factors, and its perception and treatment have changed over time as scientific understanding of autism has developed. Psychiatry has traditionally classified autism as a mental disorder, but the autism rights movement and an increasing number of researchers see autism as part of neurodiversity, the natural diversity in human thinking and experience, with strengths, differences, and weaknesses.
History
The term "autism" was introduced by Eugen Bleuler, who first described schizophrenia (a disorder that was previously known as dementia praecox) in 1911.[2] The diagnosis of schizophrenia at that time was broader than its modern equivalent, and autistic children were said to have childhood schizophrenia. Bleuler used the term "autism" to describe the situation of patients who had lost contact with reality, and who appeared to exist in their own fantasy world, unable to communicate with other people.
In the 1930s and 1940s, Leo Kanner and Hans Asperger described two related syndromes, later termed infantile autism and Asperger syndrome respectively. In 1943, Kanner published his landmark paper "Autistic Disturbances of Affective Contact," describing 11 children who displayed "a powerful desire for aloneness" and "an obsessive insistence on persistent sameness."[3] Kanner took the term "autism," which Bleuler previously attributed to the inward, introspective symptoms typical in adult schizophrenia patients, and labeled the children in his study as having "infantile autism." He classified his description of autism to be independent from the psychotic disorder of schizophrenia, explaining how autism was not a precursor to schizophrenia, and that the symptoms of autism appeared evident and present at birth and early life.
Hans Asperger described an "autistic psychopathy of childhood" which he identified in over 200 children, with particular detailed descriptions of four young boys, who showed a pattern of behavior and skills including "lack of empathy, poor ability to make friends, unidirectional conversation, strong preoccupation with special interests, and awkward movements."[4] His symptoms described ‚Äúa particularly interesting and highly recognizable type of child,‚ÄĚ later called "Asperger syndrome" and listed in the DSM-IV in 1994 as one of autism‚Äôs four subcategories.[5]
Although both Kanner and Asperger described conditions they believed to be distinct from schizophrenia, autistic children continued to be diagnosed under various terms related to schizophrenia in both the Diagnostic and Statistical Manual of Mental Disorders (DSM) and International Classification of Diseases (ICD). By the 1970s it had become more widely recognized that autism and schizophrenia were in fact distinct psychiatric conditions, and in 1980, this was formalized for the first time with new diagnostic categories in the DSM-III.[6] Asperger syndrome was introduced in the DSM-IV as a formal diagnosis in 1994, but in 2013, Asperger syndrome and infantile autism were reunified into a single diagnostic category, autism spectrum disorder (ASD).[7]
By the twenty-first century, there was a shift in attitudes away from the view that autism spectrum disorder is a disease, that must be treated or cured, toward the view that it is a part of neurodiversity, the natural diversity in human thinking and experience, with strengths, differences, and weaknesses.[8]
Classification
Before the DSM-5 (2013) and ICD-11 (2022) diagnostic manuals were adopted, what is now called ASD was found under the diagnostic category pervasive developmental disorder. The previous system relied on a set of closely related and overlapping diagnoses such as Asperger syndrome and Kanner syndrome. This created unclear boundaries between the terms, so for the DSM-5 and ICD-11, a spectrum approach was taken.
The DSM-5 and ICD-11 use different categorization tools to define this spectrum. DSM-5 uses a "level" system, which ranks how in need of support the patient is,[9] while the ICD-11 system has two axes, social communication and reciprocal social interactions and inflexible patterns of behavior, interests, or activities.[10]
Autism is currently defined as a highly variable neurodevelopmental disorder that is generally thought to cover a broad and deep spectrum, manifesting very differently from one person to another. Some have high support needs, may be non-speaking, and experience developmental delays; this is more likely with other co-existing diagnoses. Others have relatively low support needs; they may have more typical speech-language and intellectual skills but atypical social/conversation skills, narrowly focused interests, and wordy, pedantic communication. They may still require significant support in some areas of their lives.
The spectrum model should not be understood as a continuum running from mild to severe, but instead means that autism has numerous aspects that can present very differently in each person. How a person presents can depend on context, and may vary over time.
ICD
The World Health Organization's International Classification of Diseases (11th Revision), ICD-11, was was adopted by the 72nd World Health Assembly in 2019 and came into full effect as of January 2022.[11] It describes ASD as follows:
Autism spectrum disorder is characterised by persistent deficits in the ability to initiate and to sustain reciprocal social interaction and social communication, and by a range of restricted, repetitive, and inflexible patterns of behaviour, interests or activities that are clearly atypical or excessive for the individual's age and sociocultural context. The onset of the disorder occurs during the developmental period, typically in early childhood, but symptoms may not become fully manifest until later, when social demands exceed limited capacities. Deficits are sufficiently severe to cause impairment in personal, family, social, educational, occupational or other important areas of functioning and are usually a pervasive feature of the individual's functioning observable in all settings, although they may vary according to social, educational, or other context. Individuals along the spectrum exhibit a full range of intellectual functioning and language abilities.[10]
DSM
The American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), released in 2022, is the current version of the DSM.[12] It is the predominant mental health diagnostic system used in the United States and Canada, and is often used in Anglophone countries.
Its fifth edition, DSM-5, released in May 2013, was the first to define ASD as a single diagnosis, which is still the case in the DSM-5-TR. ASD encompasses previous diagnoses, including the four traditional diagnoses of autism‚ÄĒclassic Kanner syndrome, Asperger syndrome, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified (PDD-NOS)‚ÄĒand the range of diagnoses that included the word "autism." Rather than distinguishing among these diagnoses, the DSM-5 and DSM-5-TR adopt a dimensional approach to diagnosing disorders that fall underneath the autism spectrum umbrella in one diagnostic category. Within this category, the DSM includes a framework that differentiates each person by dimensions of symptom severity, as well as by associated features (the presence of other disorders or factors that likely contribute to the symptoms, other neurodevelopmental or mental disorders, intellectual disability, or language impairment).[12]
The symptom domains are social communication and restricted, repetitive behaviors, with the option of a separate severity‚ÄĒthe negative impact of the symptoms on the person‚ÄĒbeing specified for each domain, rather than an overall severity. Until 2013, deficits in social function and communication were considered two separate symptom domains. The current social communication domain criteria for autism diagnosis require people to have deficits across three social skills: social-emotional reciprocity, nonverbal communication, and developing and sustaining relationships. Further, the DSM-5 changed to an onset age "in the early developmental period," with a note that symptoms "may not become fully manifest until social communication demands exceed limited capacities," rather than the previous, more restricted three years of age.[13] These changes remain in the DSM-5-TR.
Symptoms and characteristics
For many people, autistic characteristics first appear during infancy or childhood and follow a steady course without remission. Autistic people may be severely impaired in some respects but average, or even superior, in others.[14][15]
There are many signs associated with autism, and the presentation varies widely.[16] The table below contains common signs:
Common signs for autistic spectrum disorder - avoidance of eye-contact
- little or no babbling as an infant
- not showing interest in indicated objects
- delayed language skills (e.g. having a smaller vocabulary than peers or difficulty expressing themselves in words)
- reduced interest in other children or caretakers, possibly with more interest in objects
- difficulty playing reciprocal games (e.g. peek-a-boo)
- hyper- or hypo-sensitivity to or unusual response to the smell, texture, sound, taste, or appearance of things
- resistance to changes in routine
- repetitive, limited, or otherwise unusual usage of toys (e.g. lining up toys)
- repetition of words or phrases (echolalia)
- repetitive motions or movements, including stimming
- self-harming
Social and communication skills
Autistic people display atypical nonverbal behaviors or show differences in nonverbal communication. They may make infrequent eye contact, even when called by name, or avoid it altogether. They often recognize fewer emotions and their meaning from others' facial expressions, and may not respond with facial expressions expected by their non-autistic peers.[17] At least half of autistic children have unusual prosody.[18]
Differences in verbal communication begin to be noticeable in childhood, as many autistic children develop language skills at an uneven pace. Verbal communication may be delayed or never develop (nonverbal autism), while reading ability may be present before school age (hyperlexia). Infants may show delayed onset of babbling, unusual gestures, diminished responsiveness, and vocal patterns that are not synchronized with the caregiver. In the second and third years, autistic children may have less frequent and less diverse babbling, consonants, words, and word combinations; their gestures are less often integrated with words. Autistic children are less likely to make requests or share experiences and more likely to simply repeat others' words (echolalia).[17] Autistic adults' verbal communication skills largely depend on when and how well speech is acquired during childhood.
Autistic people struggle to understand the social context and subtext of neurotypical conversational or printed situations, and form different conclusions about the content.[19] Temple Grandin, an autistic woman involved in autism activism, described her inability to understand neurotypicals' social communication as leaving her feeling "like an anthropologist from Mars."[20]
Historically, autistic children were said to be delayed in developing a theory of mind, and the empathizing‚Äďsystemizing theory has argued that while autistic people have compassion (affective empathy) for others with similar presentation of symptoms, they have limited, though not necessarily absent, cognitive empathy. Based on findings that at a population level, females are stronger empathizers and males are stronger systemizers, the "extreme male brain" theory posits that autism represents an extreme of the male pattern (impaired empathizing and enhanced systemizing).[21] This may present as social na√Įvety,[22] lower than average intuitive perception of the utility or meaning of body language, social reciprocity, and/or social expectations, including the habitus, social cues, and/or some aspects of sarcasm.[12]
According to the medical model, autistic people experience social communications impairments. This deficit-based view predicts that autistic‚Äďautistic interaction would be less effective than autistic‚Äďnon-autistic interactions or even non-functional.[23] Recent research has increasingly questioned these findings, as the "double empathy problem" theory argues that there is a lack of mutual understanding and empathy between both neurotypical persons and autistic individuals.[24][25]
However, research has found that autistic‚Äďautistic interactions are as effective in information transfer as interactions between non-autistics are, and that communication breaks down only between autistics and non-autistics:
Non-autistic people struggle to identify autistic mental states, identify autistic facial expressions, overestimate autistic egocentricity, and are less willing to socially interact with autistic people. Thus, although non-autistic people are generally characterised as socially skilled, these skills may not be functional, or effectively applied, when interacting with autistic people. [23]
Thus there has been a recent shift to acknowledge that autistic people may simply respond and behave differently than non-autistic people.
Restricted and repetitive behaviors
The second core symptom of ASD is a pattern of restricted and repetitive behaviors, activities, and interests. In order to be diagnosed with ASD under the DSM-5-TR, a person must have at least two of the following behaviors:[12]
- Repetitive behaviors ‚Äď Repetitive behaviors such as rocking, hand flapping, finger flicking, head banging, or repeating phrases or sounds. These behaviors may occur constantly or only when the person gets stressed, anxious or upset. These behaviors are also known as "stimming."
- Resistance to change ‚Äď A strict adherence to routines such as eating certain foods in a specific order or taking the same path to school every day. The person may become distressed if there is a change or disruption to their routine.
- Restricted interests ‚Äď An excessive interest in a particular activity, topic, or hobby, and devoting all their attention to it. For example, young children might completely focus on things that spin and ignore everything else. Older children might try to learn everything about a single topic, such as the weather or sports, and perseverate or talk about it constantly.
- Sensory reactivity ‚Äď An unusual reaction to certain sensory inputs, such as negative reaction to specific sounds or textures, fascination with lights or movements, or apparent indifference to pain or heat.
Self-injury
Self-injurious behaviors (SIB) are relatively common in autistic people, and can include head-banging, self-cutting, self-biting, and hair-pulling; some of these can result in serious injury or death.
- Frequency and/or continuation of self-injurious behavior can be influenced by environmental factors (such as reward for halting self-injurious behavior). However this does not apply to younger children with autism.
- Higher rates of self-injury are noted in socially isolated autistic people. This includes a suicide rate for verbal autistics that is nine times that of the general population.[26]
Other features
Autistic people may have symptoms that do not contribute to the official diagnosis, but that can affect the person or the family.
- Some people with ASD show unusual or notable abilities, ranging from splinter skills (such as the memorization of trivia) to rare talents in mathematics, music, or artistic reproduction, which in exceptional cases are considered a part of the savant syndrome.[27]
- More generally, autistic people tend to show a "spiky profile," with strong abilities in some areas contrasting with much weaker abilities in others.[28]
- Motor difficulties are common, ranging from gross motor problems, such as a clumsy, uncoordinated gait to difficulties with fine-motor control, such as manipulating objects and writing.[29]
- Pathological demand avoidance can occur. People with this set of autistic symptoms are more likely to refuse to do what is asked or expected of them, even to activities they enjoy.
- Unusual or atypical eating behavior is common in children with ASD. Selectivity is the most common problem, although eating rituals and food aversions also occur.[30]
Diagnosis
The diagnosis of autism is based on a person's reported and directly observed behavior; there are no known biomarkers for autism spectrum conditions that allow for a conclusive diagnosis.
In most cases, diagnostic criteria codified in the World Health Organization's International Classification of Diseases (ICD) or the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (DSM) are used. These reference manuals are regularly updated based on advances in research, systematic evaluation of clinical experience, and healthcare considerations. Currently, the DSM-5-TR published in 2022 and the ICD-11 that came into effect in 2022 are used. Which autism spectrum diagnoses can be made and which criteria are used depends on the local healthcare system's regulations.
According to the DSM-5-TR (2022), in order to receive a diagnosis of autism spectrum disorder, one must present with "persistent deficits in social communication and social interaction" and "restricted, repetitive patterns of behavior, interests, or activities."[12] These behaviors must begin in early childhood and affect one's ability to perform everyday tasks. Furthermore, the symptoms must not be fully explainable by intellectual developmental disorder or global developmental delay.
Diagnostic process
There are several factors that make autism spectrum disorder difficult to diagnose. First, there are no standardized imaging, molecular, or genetic tests that can be used to diagnose ASD.[31] Additionally, there is great variation in how ASD affects individuals. The behavioral manifestations of ASD depend on one's developmental stage, age of presentation, current support, and individual variability. Lastly, there are multiple conditions that may present similarly to autism spectrum disorder, including intellectual disability, hearing impairment, a specific language impairment such as Landau‚ÄďKleffner syndrome, ADHD, anxiety disorder, and psychotic disorders. Furthermore, the presence of autism can make it harder to diagnose coexisting psychiatric disorders such as depression.
Diagnosis of ASD in adults poses unique challenges because it relies on an accurate developmental history and because autistic adults sometimes learn coping strategies, known as "masking" or "camouflaging", which may make it more difficult to obtain a diagnosis.[32][11]
Differences in behavioral presentation and gender-stereotypes may make it more challenging to diagnose autism spectrum disorder in a timely manner in females. A notable percentage of autistic females may be misdiagnosed, diagnosed after a considerable delay, or not diagnosed at all.[33]
Screening
About half the parents of children with ASD notice their child's atypical behaviors by age 18 months, and about four-fifths notice by age 24 months.[34] If a child does not meet any of the following milestones, it is an indication that further evaluation should be conducted:
- No response to name (or gazing with direct eye contact) by 6 months.
- No babbling by 12 months.
- No gesturing (pointing, waving, etc.) by 12 months.
- No single words by 16 months.
- No two-word (spontaneous, not just echolalic) phrases by 24 months.
- Loss of any language or social skills, at any age.
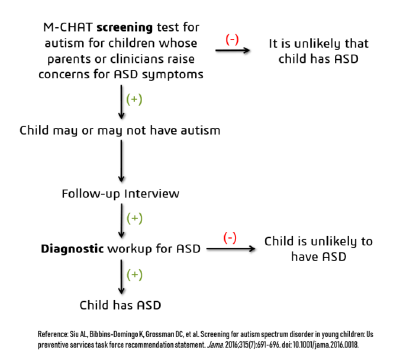
Screening tools include the Modified Checklist for Autism in Toddlers (M-CHAT), the Early Screening of Autistic Traits Questionnaire, and the First Year Inventory; initial data on M-CHAT and its predecessor, the Checklist for Autism in Toddlers (CHAT), on children aged 18‚Äď30 months suggests that it is best used in a clinical setting and that it has low sensitivity (many false-negatives) but good specificity (few false-positives).[34] It may be more accurate to precede these tests with a broadband screener that does not distinguish ASD from other developmental disorders.
Although genetic screening for autism is generally still impractical, it can be considered in some cases, such as children with neurological symptoms and dysmorphic features.
Misdiagnosis
There is a significant level of misdiagnosis of autism in neurodevelopmentally typical children. This high rate of lost diagnosis cannot be accounted for by successful ASD treatment alone. The most common reason parents reported as the cause of lost ASD diagnosis was new information about the child, such as a replacement diagnosis.
Many of the children who were later found not to meet ASD diagnosis criteria received diagnosis for another developmental disorder. Most common was ADHD, but other diagnoses included sensory disorders, anxiety, personality disorder, or learning disability. Psychological disorders may cause obsessive behavior, speech and communication problems, and other issues that may seem like autism. Some examples are: avoidant personality disorder, obsessive compulsive disorder (OCD), reactive attachment disorder, social (pragmatic) communication disorder, and schizophrenia, although this is rare in children.[35]
Some behavioral variations that resemble autistic traits are repetitive behaviors, sensitivity to change in daily routines, focused interests, and toe-walking. These are considered normal behavioral variations when they do not cause impaired function. Boys are more likely to exhibit repetitive behaviors especially when excited, tired, bored, or stressed. Some ways of distinguishing typical behavioral variations from autistic behaviors are the ability of the child to suppress these behaviors and the absence of these behaviors during sleep.
Possible causes
Exactly what causes autism remains unknown: "To date no one genetic feature or environmental cause has proven etiological in explaining most cases autism or has been able to account for rising rates of autism."[36] Despite extensive ASD research, the locus of what causes autism "whether in terms of root causes, brain bases, or psychological anomalies" is still unclear.[15]
It was long mostly presumed that there is a common cause at the genetic, cognitive, and neural levels for the social and non-social components of ASD's symptoms, described as a triad in the classic autism criteria. However, it is increasingly suspected that autism is instead a complex disorder whose core aspects have distinct causes that often co-occur.[37]
While it is unlikely that ASD has a single cause, many risk factors identified in the research literature may contribute to ASD development. These include genetics, prenatal and perinatal factors (meaning factors during pregnancy or very early infancy), neuroanatomical abnormalities, and environmental factors.
Comorbid conditions
Autism is correlated or comorbid with several personality traits/disorders. Comorbidity may increase with age and may worsen the course of youth with ASDs and make intervention and treatment more difficult. Distinguishing between ASDs and other diagnoses can be challenging because the traits of ASDs often overlap with symptoms of other disorders, and the characteristics of ASDs make traditional diagnostic procedures difficult.[36]
Some comorbid conditions are the following:
- The most common medical condition occurring in people with ASDs is seizure disorder or epilepsy; gastrointestinal problems also commonly occur in autistic people.
- Intellectual disabilities, including learning disabilities, are some of the most common comorbid disorders with ASDs, As diagnosis is increasingly being given to people with higher functioning autism, there is a tendency for the proportion with comorbid intellectual disability to decrease over time.
- Various anxiety disorders and depression tend to co-occur with ASD.[38]
- Sleep problems affect about two-thirds of people with ASD at some point in childhood. These most commonly include symptoms of insomnia, such as difficulty falling asleep, frequent nocturnal awakenings, and early morning awakenings. Sleep problems are associated with difficult behaviors and family stress, and are often a focus of clinical attention over and above the primary ASD diagnosis.
Prognosis
There is no evidence of a cure for autism. The degree of symptoms can decrease, occasionally to the extent that people lose their diagnosis of ASD. It is not known whether intensive treatment is the reason or how often this outcome happens. Although core difficulties tend to persist, symptoms often become less severe with age.
Acquiring language before age six, having an IQ above 50, and having a marketable skill all predict better outcomes; independent living is unlikely in autistic people with higher support needs.
Management
There is no treatment as such for autism, although treatment of co-occurring conditions remains an important goal. here is no cure for autism as of 2023, nor can any of the known treatments significantly reduce brain mutations caused by autism, although those who require little to no support are more likely to experience a lessening of symptoms over time.
The main goals of treatment are to lessen associated deficits and family distress, and to increase quality of life and functional independence. Behavioral, psychological, education, and/or skill-building interventions may be used to assist autistic people to learn life skills necessary for living independently, as well as other social, communication, and language skills.
While medications have not been found to help with core symptoms, they may be used for associated symptoms, such as irritability, inattention, or repetitive behavior patterns.
Non-pharmacological interventions
ASD treatment generally focuses on behavioral and educational interventions to target its two core symptoms: social communication deficits and restricted, repetitive behaviors. Intensive, sustained special education or remedial education programs and behavior therapy early in life may help children acquire self-care, social, and job skills.
Generally, when educating those with autism, specific tactics may be used to effectively relay information to these people. Using as much social interaction as possible is key in targeting the inhibition autistic people experience concerning person-to-person contact. Additionally, research has shown that employing semantic groupings, which involves assigning words to typical conceptual categories, can be beneficial in fostering learning.[39]
Educational interventions often used include applied behavior analysis (ABA), developmental models, structured teaching, speech and language therapy and social skills therapy.[40] Among these approaches, interventions either treat autistic features comprehensively, or focus treatment on a specific area of deficit.
Pharmacological interventions
No known medication relieves autism's core symptoms of social and communication impairments. Medications may be used to treat ASD symptoms that interfere with integrating a child into home or school when behavioral treatment fails. They may also be used for associated health problems, such as ADHD, anxiety, or if the person is hurting themself or aggressive with others, but their routine prescription for ASD's core features is not recommended.
More than half of US children diagnosed with ASD are prescribed psychoactive drugs or anticonvulsants, with the most common drug classes being antidepressants, stimulants, and antipsychotics.[41] SSRI antidepressants, such as fluoxetine and fluvoxamine, have been shown to be effective in reducing repetitive and ritualistic behaviors, while the stimulant medication methylphenidate is beneficial for some children with co-morbid inattentiveness or hyperactivity.[40]
Alternative medicine
A multitude of researched alternative therapies have also been implemented. Results of a systematic review on interventions to address health outcomes among autistic adults found emerging evidence to support mindfulness-based interventions for improving mental health. This includes decreasing stress, anxiety, ruminating thoughts, anger, and aggression.[42]
There is evidence to suggest that music therapy improves social interactions, verbal communication, and nonverbal communication skills.[43] Studies on pet therapy have also shown positive effects.[44]
Epidemiology
The World Health Organization (WHO) estimates about 1 in 100 children had autism during the period from 2012 to 2021 as that was the average estimate in studies published during that period with a trend of increasing prevalence over time. They note however, that this estimate represents an average figure, and reported prevalence varies substantially across studies. The prevalence of autism in many low- and middle-income countries is unknown.[1] The number of people diagnosed has increased considerably since the 1990s, which may be partly due to increased recognition of the condition.[45]
While rates of ASD are consistent across cultures, they vary greatly by gender, with boys diagnosed far more frequently than girls: ASD is more than four times more common among boys than among girls.[46]
Society and culture
An autistic culture has emerged, accompanied by the autistic rights and neurodiversity movements, that argues autism should be accepted as a difference to be accommodated rather than cured.
Worldwide, events related to autism include the United Nations-sanctioned World Autism Awareness Day on April 2, which leads into and World Autism Month celebrated by "Autism Speaks."[47]
Neurodiversity movement
Some autistic people, as well as a growing number of researchers, have advocated a shift in attitudes toward the view that autism spectrum disorder is a difference, rather than a disease that must be treated or cured.[48]
"Neurodiversity" is understood as:
The idea that people experience and interact with the world around them in many different ways; there is no one "right" way of thinking, learning, and behaving, and differences are not viewed as deficits.[49]
The neurodiversity claim for ASD contains two different aspects: The first is that autism is a natural variation; the second aspect is about conferring rights and value to the neurodiversity condition, demanding recognition and acceptance without being labelled disabled or as having a disorder.[50]
The autism rights movement advocates for including greater acceptance of autistic behaviors; therapies that focus on coping skills rather than imitating the behaviors of those without autism; and the recognition of the autistic community as a minority group.[51]
Symbols and flags
Over the years, multiple organizations have tried to capture the essence of autism in symbols. In 1963, the board for the National Autistic Society, led by Gerald Gasson, proposed the "puzzle piece" as a symbol for autism, because it fit their view of autism as a "puzzling condition."[52] In 1999, the Autism Society adopted the puzzle ribbon as the universal sign of autism awareness, representing the complexity of the autism spectrum: "With each piece being a different color and shape, it shows that autism affects a diverse group of people and that no two people or families have the same experience with autism." [53]
The puzzle symbol later received mixed reviews as the mystery of autism began to be replaced with an understanding of neurodiversity. Several different symbols have been suggested, including the infinity symbol with rainbow colors as well as gold. However, no consensus has been reached.
Caregivers
Families who care for an autistic child face added stress from a number of different causes.[54] Parents may struggle to understand the diagnosis and to find appropriate care options.
Siblings of children with ASD experience a wide range of challenges, but while there are some shared experiences, each situation is unique. Aside from the variation in autistic children themselves, the family dynamics and financial situation greatly impact any sibling's experience: "Life with an autistic sibling can be overwhelmingly difficult. For others, it has its ups and downs. There are even some children who see their sibling's autism as a plus." [55]
Notes
- ‚ÜĎ 1.0 1.1 Autism World Health Organization (November 15, 2023). Retrieved January 11, 2024.
- ‚ÜĎ Eugen Bleuler, Joseph Zinkin (trans.), Dementia Praecox or The Group of Schizophrenias (International Universities Press, 1950 (original 1911).
- ‚ÜĎ Leo Kanner, Autistic Disturbances of Affective Contact Nervous Child 35 (4): 100‚Äď136. Retrieved January 12, 2024.
- ‚ÜĎ Hans Asperger, ‚Äú‚ÄėAutistic Psychopathy‚Äô in Childhood,‚ÄĚ in Autism and Asperger Syndrome edited by Uta Frith (Cambridge University Press, 1991, ISBN 978-0521386081), 37-92. Originally published as ‚ÄúDie ‚ÄėAutistischen Psychopathen‚Äô im Kindesalter,‚ÄĚ Archiv f√ľr Psychiatrie und Nervenkrankenheiten 117 (1944):76-136.
- ‚ÜĎ American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders DSM-IV, 4th ed (Washington, DC: American Psychiatric Association, 1994, ISBN 0890420610).
- ‚ÜĎ American Psychiatric Association, DSM-III: Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition (American Psychiatric Association, 1980, ISBN 978-0521315289).
- ‚ÜĎ American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5 (American Psychiatric Publishing, 2013, ISBN 978-0890425541).
- ‚ÜĎ Andrew Solomon, The Autism Rights Movement The New Yorker (May 23, 2008). Retrieved January 12, 2024.
- ‚ÜĎ Autism Spectrum Disorder (ASD): Diagnostic Criteria CDC (November 2, 2022). Retrieved January 12, 2024.
- ‚ÜĎ 10.0 10.1 6A02 Autism spectrum disorder: Diagnostic Requirements ICD-11 for Mortality and Morbidity Statistics (January 2023). Retrieved January 12, 2024.
- ‚ÜĎ 11.0 11.1 ICD-11 World Health Organization. Retrieved January 12, 2024.
- ‚ÜĎ 12.0 12.1 12.2 12.3 12.4 American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition Text Revision: DSM-5-TR (American Psychiatric Publishing, 2022, ISBN 0890425760).
- ‚ÜĎ DSM-5 Diagnostic Criteria: Autism Spectrum Disorder Interagency Autism Coordinating Committee (IACC), U.S. Department of Health & Human Services. Retrieved January 12, 2024.
- ‚ÜĎ Louise Cummings (ed.), Handbook of Pragmatic Language Disorders (Springer, 2021, ISBN 978-3030749842).
- ‚ÜĎ 15.0 15.1 Jill Boucher, Autism Spectrum Disorders (SAGE Publications Ltd, 2022, ISBN 978-1529744651).
- ‚ÜĎ Autism: Signs and symptoms Public Health Agency of Canada (April 7, 2022). Retrieved January 12, 2024.
- ‚ÜĎ 17.0 17.1 Autism Spectrum Disorder: Communication Problems in Children National Institute on Deafness and Other Communication Disorders (April 13, 2020). Retrieved January 12, 2024.
- ‚ÜĎ Riccardo Fusaroli, Anna Lambrechts, Dan Bang, Dermot M. Bowler, and Sebastian B. Gaigg, "Is voice a marker for Autism spectrum disorder? A systematic review and meta-analysis" Autism Research 10(3) (2017):384‚Äď407. Retrieved January 12, 2024.
- ‚ÜĎ Beverly Vicker, Social communication and language characteristics associated with high-functioning, verbal children and adults with autism spectrum disorder Indiana Resource Center for Autism. Retrieved January 12, 2024.
- ‚ÜĎ David Cohen, Temple Grandin: 'I'm an anthropologist from Mars' The Guardian (October 25, 2005). Retrieved January 12, 2024.
- ‚ÜĎ Simon Baron-Cohen, Rebecca C. Knickmeyer, and Matthew K. Belmonte, Sex differences in the brain: implications for explaining autism Science 310(5749) (November 4, 2005): 819‚Äď823. Retrieved January 12, 2024.
- ‚ÜĎ James C. McPartland, Ami Klin, and Fred R. Volkmar (eds.), Asperger Syndrome: Assessing and Treating High-Functioning Autism Spectrum Disorders (The Guilford Press, 2014, ISBN 978-1462514144).
- ‚ÜĎ 23.0 23.1 Catherine J. Crompton et al., Autistic peer-to-peer information transfer is highly effective Autism 24(7) (May 20, 2020):1704‚Äď1712. Retrieved January 12, 2024.
- ‚ÜĎ Damian E.M. Milton, On the ontological status of autism: the 'double empathy problem' Disability & Society 27(6) (October 2012):883‚Äď887. Retrieved January 12, 2024.
- ‚ÜĎ Damian Milton, Emine Gurbuz, and Beatriz L√≥pez, The 'double empathy problem': Ten years on Autism 26(8) (November, 2022):1901‚Äď1903. Retrieved January 12, 2024.
- ‚ÜĎ Amelia Hill, Autism could be seen as part of personality for some diagnosed, experts say The Guardian (July 31, 2023). Retrieved January 13, 2024.
- ‚ÜĎ Darold A. Treffert, The savant syndrome: an extraordinary condition. A synopsis: past, present, future Philosophical Transactions of the Royal Society of London: Series B, Biological Sciences 364(1522) (2009): 1351‚Äď1357. Retrieved January 13, 2024.
- ‚ÜĎ Nancy Doyle, Neurodiversity at work: a biopsychosocial model and the impact on working adults British Medical Bulletin 135(1) (September 2020):108‚Äď125. Retrieved January 15, 2024.
- ‚ÜĎ Lauren Schenkman, Motor difficulties in autism, explained Spectrum (August 13, 2022). Retrieved January 15, 2024.
- ‚ÜĎ Autism and Food Aversions Autism Speaks. Retrieved January 15, 2024.
- ‚ÜĎ Screening and Diagnosis of Autism Spectrum Disorder Centers for Disease Control and Prevention (March 31, 2022). Retrieved January 15, 2024.
- ‚ÜĎ Yunhe Huang, Samuel R. Arnold, Kitty-Rose Foley, and Julian N. Trollor, Diagnosis of autism in adulthood: A scoping review Autism 24(6) (August 2020):1311‚Äď1327. Retrieved January 16, 2024.
- ‚ÜĎ Georgia Lockwood Estrin, Victoria Milner, Debbie Spain, Francesca Happ√©, and Emma Colvert, Barriers to Autism Spectrum Disorder Diagnosis for Young Women and Girls: a Systematic ReviewReview Journal of Autism and Developmental Disorders 8(4) (October 29, 2020):454‚Äď470. Retrieved January 16, 2024.
- ‚ÜĎ 34.0 34.1 Rebecca J. Landa, Diagnosis of autism spectrum disorders in the first 3 years of life Nature Clinical Practice: Neurology 4(3) (February 5, 2008). Retrieved January 16, 2024.
- ‚ÜĎ Camille Noe Pag√°n, Conditions That May Look Like Autism, but Aren't WebMD (January 18, 2022). Retrieved January 16, 2024.
- ‚ÜĎ 36.0 36.1 Johnny L. Matson and Peter Sturmey (eds.), Handbook of Autism and Pervasive Developmental Disorder: Assessment, Diagnosis, and Treatment (Springer, 2022, ISBN 978-3030885373).
- ‚ÜĎ Francesca Happ√© and Angelica Ronald, The 'fractionable autism triad': a review of evidence from behavioural, genetic, cognitive and neural research Neuropsychology Review 18(4) (December 2008):287‚Äď304. Retrieved January 16, 2024.
- ‚ÜĎ Eric J. Mash and Russell A. Barkley (eds.), Child Psychopathology (The Guilford Press, 2014, ISBN 978-1462516681).
- ‚ÜĎ Marian Sigman and Lisa Capps, Children with Autism: A Developmental Perspective (Harvard University Press, 1997, ISBN 978-0674053137).
- ‚ÜĎ 40.0 40.1 Scott M. Myers and Chris Plauch√© Johnson, Management of children with autism spectrum disorders Pediatrics 120(5) (November 2007):1162‚Äď1182. Retrieved January 16, 2024.
- ‚ÜĎ Carolyn A. Doyle and Christopher J. McDougle, Pharmacologic treatments for the behavioral symptoms associated with autism spectrum disorders across the lifespan Dialogues in Clinical Neuroscience 14(3) (2012):263‚Äď279. Retrieved January 17, 2024.
- ‚ÜĎ Teal W. Benevides et al., Interventions to address health outcomes among autistic adults: A systematic review Autism (24)(6) (August 2020):1345‚Äď1359. Retrieved January 17, 2024.
- ‚ÜĎ M. Geretsegger, L. Fusar-Poli, C. Elefant, K.A. M√∂ssler, G. Vitale, and C. Gold, Music therapy for autistic people Cochrane Database Syst Rev. (2022)(5) (May 2022): CD004381. Retrieved January 17, 2024.
- ‚ÜĎ Christina B. Rumayor and Amy M. Thrasher, Reflections on Recent Research Into Animal-Assisted Interventions in the Military and Beyond Current Psychiatry Reports 19(12) (November 2017):110. Retrieved January 17, 2024.
- ‚ÜĎ G. Russell, S. Stapley, T. Newlove-Delgado, A. Salmon, R. White, F. Warren, A. Pearson, and T. Ford, "Time trends in autism diagnosis over 20 years: a UK population-based cohort study" Journal of Child Psychology and Psychiatry, and Allied Disciplines 63(6) (August 2021):674‚Äď682.
- ‚ÜĎ Autism spectrum disorder (ASD): How Often ASD Occurs Centers for Disease Control and Prevention (December 9, 2022). Retrieved January 11, 2024.
- ‚ÜĎ World Autism Awareness Day Autism Speaks. Retrieved January 15, 2024.
- ‚ÜĎ Elizabeth Pellicano and Jacquiline den Houting, Annual Research Review: Shifting from ‚Äėnormal science‚Äô to neurodiversity in autism science Journal of Child Psychology and Psychiatry, and Allied Disciplines 63(4) (November 2021):381‚Äď396. Retrieved January 17, 2024.
- ‚ÜĎ Nicole Baumer and Julia Frueh, What is neurodiversity? Harvard Health Publishing (November 23, 2021). Retrieved January 17, 2024.
- ‚ÜĎ Pier Jaarsma and Stellan Welin, Autism as a natural human variation: reflections on the claims of the neurodiversity movement Health Care Analysis 20(1) (March 2012):20‚Äď30. Retrieved January 17, 2024.
- ‚ÜĎ Paul Ratner, Should Autism Be Cured or Is "Curing" Offensive? Big Think (July 10, 2016). Retrieved January 17, 2024.
- ‚ÜĎ Debra Muzikar, The Autism Puzzle Piece: A symbol that‚Äôs going to stay or go? The Art of Autism (April 20, 2019). Retrieved January 15, 2024.
- ‚ÜĎ Debra Solomon, The History of the Autism Puzzle Piece Ribbon Spectrum Strategies (May 2, 2018). Retrieved January 15, 2024.
- ‚ÜĎ Fred R. Volkmar, Sally J. Rogers, Rhea Paul, and Kevin A. Pelphrey (eds.), Handbook of Autism and Pervasive Developmental Disorders: Volume Two: Assessment, Interventions, and Policy (‚ÄéWiley, 2014, ISBN 978-1118107034).
- ‚ÜĎ Lisa Jo Rudy, What It's Like Being the Sibling of an Autistic Child Very Well Mind (November 27, 2023). Retrieved January 15, 2024.
ReferencesISBN links support NWE through referral fees
- American Psychiatric Association. DSM-III: Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition. American Psychiatric Association, 1980. ISBN 978-0521315289
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-IV, 4th ed. Washington, DC: American Psychiatric Association, 1994. ISBN 0890420610
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. American Psychiatric Publishing, 2013. ISBN 978-0890425541
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition Text Revision: DSM-5-TR. American Psychiatric Publishing, 2022. ISBN 0890425760
- Boucher, Jill. Autism Spectrum Disorders. SAGE Publications Ltd, 2022. ISBN 978-1529744651
- Cummings, Louise (ed.). Handbook of Pragmatic Language Disorders. Springer, 2021. ISBN 978-3030749842
- Frith, Uta. Autism and Asperger Syndrome. Cambridge University Press, 1991. ISBN 978-0521386081
- Mash, Eric J., and Russell A. Barkley (eds.). Child Psychopathology. The Guilford Press, 2014. ISBN 978-1462516681
- Matson, Johnny L., and Peter Sturmey (eds.). Handbook of Autism and Pervasive Developmental Disorder: Assessment, Diagnosis, and Treatment. Springer, 2022. ISBN 978-3030885373
- McPartland, James C., Ami Klin, and Fred R. Volkmar (eds.). Asperger Syndrome: Assessing and Treating High-Functioning Autism Spectrum Disorders. The Guilford Press, 2014. ISBN 978-1462514144
- Sigman, Marian, and Lisa Capps. Children with Autism: A Developmental Perspective. Harvard University Press, 1997. ISBN 978-0674053137
- Volkmar, Fred R., Sally J. Rogers, Rhea Paul, and Kevin A. Pelphrey (eds.). Handbook of Autism and Pervasive Developmental Disorders: Volume Two: Assessment, Interventions, and Policy. Wiley, 2014. ISBN 978-1118107034
External links
All links retrieved January 17, 2024.
- Autism World Health Organization (WHO)
- Autism spectrum disorder (ASD) Centers for Disease Control and Prevention (CDC)
- Autism Spectrum Disorder National Institute of Mental Health (NIMH)
- What Is Autism? Autism Speaks
- What Is Autism Spectrum Disorder? American Psychiatric Association
- Autism spectrum disorder Mayo Clinic
- Autism Spectrum Disorder Cleveland Clinic
- International Classification of Diseases 11th Revision (ICD-11) World Health Organization
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.