Addiction
Currently working on —Jennifer Tanabe (talk) May 2020
Addiction is a brain disorder characterized by compulsive engagement in rewarding stimuli despite adverse consequences. Despite the involvement of a number of psychosocial factors, a biological process—one that is induced by repeated exposure to an addictive stimulus—is the core pathology that drives the development and maintenance of an addiction. The two properties that characterize all addictive stimuli are that they are reinforcing (i.e., they increase the likelihood that a person will seek repeated exposure to them) and intrinsically rewarding (i.e., they are perceived as being inherently positive, desirable, and pleasurable).
Classic hallmarks of addiction include impaired control over substances or behavior, preoccupation with substance or behavior, and continued use despite consequences. Habits and patterns associated with addiction are typically characterized by immediate gratification (short-term reward), coupled with delayed deleterious effects (long-term costs).
Definition
The American Society of Addiction Medicine defines addiction as follows:
Addiction is a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and an individual’s life experiences. People with addiction use substances or engage in behaviors that become compulsive and often continue despite harmful consequences.[1]
Addiction is a brain disorder characterized by compulsive engagement in rewarding stimuli despite adverse consequences.[2] The two properties that characterize all addictive stimuli are that they are reinforcing (in other words, they increase the likelihood that a person will seek repeated exposure to them) and intrinsically rewarding (meaning, they are perceived as being inherently positive, desirable, and pleasurable).[3]
Classic hallmarks of addiction include impaired control over substances or behavior, preoccupation with substance or behavior, and continued use despite consequences. Habits and patterns associated with addiction are typically characterized by immediate gratification (short-term reward), coupled with delayed deleterious effects (long-term costs).[4]
Types of addiction
| Addiction and dependence glossary | |
* addiction – a biopsychosocial disorder characterized by compulsively seeking to achieve a desired effect, such as intoxication, despite harm and adverse consequences to self and others
|
Addiction has traditionally been used in reference to substance abuse where there are obvious physical dependencies. However, the term has been expanded to include behaviors that may lead to a reward (such as gambling, eating, sexual activity, or even shopping).[5] A gene transcription factor known as ΔFosB has been identified as a necessary common factor involved in both behavioral and drug addictions, which are associated with the same set of neural adaptations in the reward system.[6][7]
Examples of drug and behavioral addictions include alcoholism, marijuana addiction, amphetamine addiction, cocaine addiction, nicotine addiction, opioid addiction, food addiction, video game addiction, gambling addiction, and sexual addiction. The only behavioral addiction recognized by the DSM-5 and the ICD-10 is gambling addiction. With the introduction of the ICD-11 gaming addiction was appended.[8]
The term addiction is misused frequently to refer to other compulsive behaviors or disorders, particularly dependence.[9] An important distinction between drug addiction and dependence is that drug dependence is a disorder in which cessation of drug use results in an unpleasant state of withdrawal, which can lead to further drug use. Addiction is the compulsive use of a substance or performance of a behavior that is independent of withdrawal. Addiction can occur in the absence of dependence, and dependence can occur in the absence of addiction, although the two often occur together.
Biological mechanisms
ΔFosB, a gene transcription factor, has been identified as playing a critical role in the development of addictive states in both behavioral addictions and drug addictions.[6][10][7] Overexpression of ΔFosB in the nucleus accumbens is necessary and sufficient for many of the neural adaptations seen in drug addiction; it has been implicated in addictions to alcohol, cannabinoids, cocaine, nicotine, phenylcyclidine, and substituted amphetamines[6][11] as well as addictions to natural rewards such as sex, exercise, and food.[10][7]
In the nucleus accumbens, ΔFosB functions as a "sustained molecular switch" and "master control protein" in the development of an addiction.In other words, once "turned on" (sufficiently overexpressed) ΔFosB triggers a series of transcription events that ultimately produce an addictive state (compulsive reward-seeking involving a particular stimulus); this state is sustained for months after cessation of drug use due to the abnormal and exceptionally long half-life of ΔFosB isoforms.[12] ΔFosB expression in D1-type nucleus accumbens medium spiny neurons directly and positively regulates drug self-administration and reward sensitization through positive reinforcement while decreasing sensitivity to aversion.[13]
Besides increased ΔFosB expression in the nucleus accumbens, there are many other correlations in the neurobiology of behavioral addictions with drug addictions.
Behaviors like gambling have been linked to the new found idea of the brain's capacity to anticipate rewards. The reward system can be triggered by early detectors of the behavior, and trigger dopamine neurons to begin stimulating behaviors. But in some cases, it can lead to many issues due to error, or reward-prediction errors. These errors can act as teaching signals to create a complex behavior task over time.[14]
One of the most important discoveries of addictions has been the drug based reinforcement and, even more important, reward based learning processes. Several structures of the brain are important in the conditioning process of behavioral addiction; these subcortical structures form the brain regions known as the reward system. One of the major areas of study is the amygdala, a brain structure which involves emotional significance and associated learning. Research shows that dopaminergic projections from the ventral tegmental area facilitate a motivational or learned association to a specific behavior.[15] Dopamine neurons take a role in the learning and sustaining of many acquired behaviors. The most common mechanism of dopamine is to create addictive properties along with certain behaviors.[16]
There are three stages to the dopamine reward system: bursts of dopamine, triggering of behavior, and further impact to the behavior. Once electronically signaled, possibly through the behavior, dopamine neurons let out a ‘burst-fire’ of elements to stimulate areas along fast transmitting pathways. The behavior response then perpetuates the striated neurons to further send stimuli.[14] Once the behavior is triggered, it is hard to work away from the dopamine reward system.
Substance use disorder
Substance use disorder (SUD), also known as a drug use disorder, is the persistent use of drugs (including alcohol) despite substantial harm and adverse consequences. Such addiction can be defined as "the compulsive seeking and taking of drugs despite horrendous consequences or loss of control over drug use."[13] Substance use disorders are characterized by an array of mental, physical, and behavioral symptoms that may cause problems related to loss of control, strain to one's interpersonal life, hazardous use, tolerance, and withdrawal.[17]
In the current Diagnostic and Statistical Manual of Mental Disorders, DSM-5, substance abuse and substance dependence have been merged into the category of substance use disorders.ref name=DSM-5/> The severity of substance use disorders can vary widely; in the diagnosis of a SUD, the severity of an individual's SUD is qualified as mild, moderate, or severe on the basis of how many of the 11 diagnostic criteria are met.
Drug classes that are involved in SUD include: alcohol; caffeine; cannabis; hallucinogens (such as arylcyclohexylamines); other hallucinogens (such as LSD); inhalants; opioids; sedatives, hypnotics, or anxiolytics; stimulants; tobacco; and other or unknown substances.[18]
Addiction exacts an "astoundingly high financial and human toll" on individuals and society as a whole.[2] In the United States, the total economic cost to society is greater than that of all types of diabetes and all cancers combined:
Risky substance use and untreated addiction account for one-third of inpatient hospital costs and 20 percent of all deaths in the United States each year, and cause or contribute to more than 100 other conditions requiring medical care, as well as vehicular crashes, other fatal and non-fatal injuries, overdose deaths, suicides, homicides, domestic discord, the highest incarceration rate in the world and many other costly social consequences. The economic cost to society is greater than the cost of diabetes and all cancers combined. [19]
These costs arise from the direct adverse effects of drugs and associated healthcare costs, long-term complications (such as lung cancer from smoking tobacco products, liver cirrhosis and dementia from chronic alcohol consumption, and meth mouth from methamphetamine use), the loss of productivity and associated welfare costs, fatal and non-fatal accidents, suicides, homicides, and incarceration, among others.[20]
Diagnosis
Diagnosis of substance use disorder (SUD) usually involves an in-depth examination, typically by psychiatrist, psychologist, or drug and alcohol counselor.[21] The most commonly used guidelines are published in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5).<[17]
The 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) uses the term "substance use disorder" to refer to a spectrum of drug use-related disorders. The DSM-5 eliminates the terms "abuse" and "dependence" from diagnostic categories, instead using the specifiers of mild, moderate and severe to indicate the extent of disordered use. These specifiers are determined by the number of diagnostic criteria present in a given case. In the DSM-5, the term drug addiction is synonymous with severe substance use disorder.
There are 11 diagnostic criteria which can be broadly categorized into issues arising from substance use related to loss of control, strain to one's interpersonal life, hazardous use, and pharmacologic effects. DSM-5 guidelines for the diagnosis of a substance use disorder requires that the individual have significant impairment or distress from their pattern of drug use, and at least two of the symptoms listed below in a given year.[17]
- Using more of a substance than planned, or using a substance for a longer interval than desired
- Inability to cut down despite desire to do so
- Spending substantial amount of the day obtaining, using, or recovering from substance use
- Cravings or intense urges to use
- Repeated usage causes or contributes to an inability to meet important social, or professional obligations
- Persistent usage despite user's knowledge that it is causing frequent problems at work, school, or home
- Giving up or cutting back on important social, professional, or leisure activities because of use
- Using in physically hazardous situations, or usage causing physical or mental harm
- Persistent use despite the user's awareness that the substance is causing or at least worsening a physical or mental problem
- Tolerance: needing to use increasing amounts of a substance to obtain its desired effects
- Withdrawal: characteristic group of physical effects or symptoms that emerge as amount of substance in the body decreases
There are additional qualifiers and exceptions outlined in the DSM. For instance, if an individual is taking opiates as prescribed, they may experience physiologic effects of tolerance and withdrawal, but this would not cause an individual to meet criteria for a SUD without additional symptoms also being present.[17]
Past editions have used physical dependence and the associated withdrawal syndrome to identify an addictive state. Tolerance is the process by which the body continually adapts to the substance and requires increasingly larger amounts to achieve the original effects. Physical dependence occurs when the body has adjusted by incorporating the substance into its "normal" functioning – attained homeostasis – and therefore physical withdrawal symptoms occur upon cessation of use. Symptoms of withdrawal generally include, but are not limited to, body aches, anxiety, irritability, intense cravings for the substance, nausea, hallucinations, headaches, cold sweats, tremors, and seizures.
Medical researchers who actively study addiction have criticized the DSM classification of addiction for being flawed and involving arbitrary diagnostic criteria.[2] Writing in 2013, the director of the United States National Institute of Mental Health discussed the invalidity of the DSM-5's classification of mental disorders:[22]
While DSM has been described as a "Bible" for the field, it is, at best, a dictionary, creating a set of labels and defining each. The strength of each of the editions of DSM has been "reliability" – each edition has ensured that clinicians use the same terms in the same ways. The weakness is its lack of validity. Unlike our definitions of ischemic heart disease, lymphoma, or AIDS, the DSM diagnoses are based on a consensus about clusters of clinical symptoms, not any objective laboratory measure. In the rest of medicine, this would be equivalent to creating diagnostic systems based on the nature of chest pain or the quality of fever.
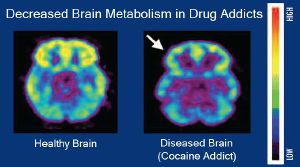
Given that addiction manifests in structural changes to the brain, it is possible that non-invasive neuroimaging scans obtained via MRI could be used to help diagnose addiction in the future.[23] As a diagnostic biomarker, ΔFosB expression could be used to diagnose addiction, but this would require a brain biopsy and therefore is not used in clinical practice.
Treatment
According to a review, "in order to be effective, all pharmacological or biologically based treatments for addiction need to be integrated into other established forms of addiction rehabilitation, such as cognitive behavioral therapy, individual and group psychotherapy, behavior-modification strategies, twelve-step programs, and residential treatment facilities."[24]
Detoxification
Depending on the severity of use, and the given substance, early treatment of acute withdrawal may include medical detoxification. Of note, acute withdrawal from heavy alcohol use should be done under medical supervision to prevent a potentially deadly withdrawal syndrome known as delirium tremens. See also Alcohol detoxification.
Therapy
Therapists often classify people with chemical dependencies as either interested or not interested in changing. About 11% of Americans with substance use disorder seek treatment, and 40–60% of those people relapse within a year.[25] Treatments usually involve planning for specific ways to avoid the addictive stimulus, and therapeutic interventions intended to help a client learn healthier ways to find satisfaction. Clinical leaders in recent years have attempted to tailor intervention approaches to specific influences that affect addictive behavior, using therapeutic interviews in an effort to discover factors that led a person to embrace unhealthy, addictive sources of pleasure or relief from pain.
From the applied behavior analysis literature and the behavioral psychology literature, several evidence-based intervention programs have emerged, such as behavioral marital therapy, community reinforcement approach, cue exposure therapy, and contingency management strategies.[26][27] In addition, the same author suggests that social skills training adjunctive to inpatient treatment of alcohol dependence is probably efficacious.
A meta-analytic review on the efficacy of various behavioral therapies for treating drug and behavioral addictions found that cognitive behavioral therapy (e.g., relapse prevention and contingency management), motivational interviewing, and a community reinforcement approach were effective interventions with moderate effect sizes.[28]
Clinical and preclinical evidence indicate that consistent aerobic exercise, especially endurance exercise (e.g., marathon running), actually prevents the development of certain drug addictions and is an effective adjunct treatment for drug addiction, and for psychostimulant addiction in particular.[10][29][30][31][32] Consistent aerobic exercise magnitude-dependently (i.e., by duration and intensity) reduces drug addiction risk, which appears to occur through the reversal of drug induced addiction-related neuroplasticity.[10][30] One review noted that exercise may prevent the development of drug addiction by altering ΔFosB or c-Fos immunoreactivity in the striatum or other parts of the reward system.[32] Aerobic exercise decreases drug self-administration, reduces the likelihood of relapse, and induces opposite effects on striatal dopamine receptor D2 (DRD2) signaling (increased DRD2 density) to those induced by addictions to several drug classes (decreased DRD2 density).[10][30] Consequently, consistent aerobic exercise may lead to better treatment outcomes when used as an adjunct treatment for drug addiction.[10][30][31]
Medication
Medication-assisted treatment (MAT) refers to the combination of behavioral interventions and medications to treat substance use disorders.[33] Certain medications can be useful in treating severe substance use disorders. In the United States five medications are approved to treat alcohol and opioid use disorders.[34] There are no approved medications for cocaine, methamphetamine, or other substance use disorders as of 2002.[34]
Medications, such as methadone and disulfiram, can be used as part of broader treatment plans to help a patient function comfortably without illicit opioids or alcohol.[35] Medications can be used in treatment to lessen withdrawal symptoms. Evidence has demonstrated the efficacy of MAT at reducing illicit drug use and overdose deaths, improving retention in treatment, and reducing HIV transmission.[36][37][38]
Alcohol addiction
- Further information: Alcoholism
Alcohol, like opioids, can induce a severe state of physical dependence and produce withdrawal symptoms such as delirium tremens. Because of this, treatment for alcohol addiction usually involves a combined approach dealing with dependence and addiction simultaneously. Benzodiazepines have the largest and the best evidence base in the treatment of alcohol withdrawal and are considered the gold standard of alcohol detoxification.[39]
Pharmacological treatments for alcohol addiction include drugs like naltrexone (opioid antagonist), disulfiram, acamprosate, and topiramate.[40][41] Rather than substituting for alcohol, these drugs are intended to affect the desire to drink, either by directly reducing cravings as with acamprosate and topiramate, or by producing unpleasant effects when alcohol is consumed, as with disulfiram. These drugs can be effective if treatment is maintained, but compliance can be an issue as alcoholic patients often forget to take their medication, or discontinue use because of excessive side effects.[42][43] According to a Cochrane Collaboration review, the opioid antagonist naltrexone has been shown to be an effective treatment for alcoholism, with the effects lasting three to twelve months after the end of treatment.[44]
Cannabinoid addiction
As of 2010, there are no effective pharmacological interventions for cannabinoid addiction.[45] A 2013 review on cannabinoid addiction noted that the development of CB1 receptor agonists that have reduced interaction with β-arrestin 2 signaling might be therapeutically useful.[46]
Nicotine addiction
- Further information: Smoking cessation
Another area in which drug treatment has been widely used is in the treatment of nicotine addiction, which usually involves the use of nicotine replacement therapy, nicotinic receptor antagonists, or nicotinic receptor partial agonists.[47][48] Examples of drugs that act on nicotinic receptors and have been used for treating nicotine addiction include antagonists like bupropion and the partial agonist varenicline.[47][48]
Opioid addiction
- Further information: Opioid use disorder
Opioids cause physical dependence, and treatment typically addresses both dependence and addiction.
Physical dependence is treated using replacement drugs such as suboxone or subutex (both containing the active ingredients buprenorphine) and methadone.[49][50] Although these drugs perpetuate physical dependence, the goal of opiate maintenance is to provide a measure of control over both pain and cravings. Use of replacement drugs increases the addicted individual's ability to function normally and eliminates the negative consequences of obtaining controlled substances illicitly. Once a prescribed dosage is stabilized, treatment enters maintenance or tapering phases. In the United States, opiate replacement therapy is tightly regulated in methadone clinics and under the DATA 2000 legislation. In some countries, other opioid derivatives such as levomethadyl acetate,[51] dihydrocodeine,[52] dihydroetorphine[53] and even heroin[54][55] are used as substitute drugs for illegal street opiates, with different prescriptions being given depending on the needs of the individual patient. Baclofen has led to successful reductions of cravings for stimulants, alcohol, and opioids, and also alleviates alcohol withdrawal syndrome. Many patients have stated they "became indifferent to alcohol" or "indifferent to cocaine" overnight after starting baclofen therapy.[56] Some studies show the interconnection between opioid drug detoxification and overdose mortality.[57]
Psychostimulant addiction
As of May 2014, there is no effective pharmacotherapy for any form of psychostimulant addiction.[24][58][59][60] Reviews from 2015, 2016, and 2018 indicated that TAAR1-selective agonists have significant therapeutic potential as a treatment for psychostimulant addictions;[61][62][63] however, as of 2018, the only compounds which are known to function as TAAR1-selective agonists are experimental drugs.[61][62][63]
Research
Template:Expand section Research indicates that vaccines which utilize anti-drug monoclonal antibodies can mitigate drug-induced positive reinforcement by preventing the drug from moving across the blood–brain barrier;[64] however, current vaccine-based therapies are only effective in a relatively small subset of individuals.[64][65] As of November 2015, vaccine-based therapies are being tested in human clinical trials as a treatment for addiction and preventive measure against drug overdoses involving nicotine, cocaine, and methamphetamine.[64]
The new study shows, that the vaccine may also save lives during a drug overdose. In this instance, the idea is that the body will respond to the vaccine by quickly producing antibodies to prevent the opioids from accessing the brain.[66]
Since addiction involves abnormalities in glutamate and GABAergic neurotransmission,[67][68] receptors associated with these neurotransmitters (e.g., AMPA receptors, NMDA receptors, and GABAB receptors) are potential therapeutic targets for addictions.[67][68][69][70] N-acetylcysteine, which affects metabotropic glutamate receptors and NMDA receptors, has shown some benefit in preclinical and clinical studies involving addictions to cocaine, heroin, and cannabinoids.[67] It may also be useful as an adjunct therapy for addictions to amphetamine-type stimulants, but more clinical research is required.[67]
Current medical reviews of research involving lab animals have identified a drug class – class I histone deacetylase inhibitors[note 1] – that indirectly inhibits the function and further increases in the expression of accumbal ΔFosB by inducing G9a expression in the nucleus accumbens after prolonged use.[73][74][71][72] These reviews and subsequent preliminary evidence which used oral administration or intraperitoneal administration of the sodium salt of butyric acid or other class I HDAC inhibitors for an extended period indicate that these drugs have efficacy in reducing addictive behavior in lab animals[note 2] that have developed addictions to ethanol, psychostimulants (i.e., amphetamine and cocaine), nicotine, and opiates;[74][72][75][76] however, few clinical trials involving human addicts and any HDAC class I inhibitors have been conducted to test for treatment efficacy in humans or identify an optimal dosing regimen.[note 3]
Gene therapy for addiction is an active area of research. One line of gene therapy research involves the use of viral vectors to increase the expression of dopamine D2 receptor proteins in the brain.[78][79][80][81][82]
Risk factors
There are many known risk factors associated with an increased chance of developing a substance use disorder. Children born to parents with SUDs have roughly a two-fold increased risk in developing a SUD compared to children born to parents without any SUDs.[83] Taking highly addictive drugs, and those who develop SUDs in their teens are more likely to have continued symptoms into adulthood.[83] Other common risk factors are being male, being under 25, having other mental health problems, and lack of familial support and supervision.[83] Psychological risk factors include high impulsivity, sensation seeking, neuroticism and openness to experience in combination with low conscientiousness.[84][85]
There are a number of genetic and environmental risk factors for developing an addiction, that vary across the population.[13][86] Genetic and environmental risk factors each account for roughly half of an individual's risk for developing an addiction;[13] the contribution from epigenetic risk factors to the total risk is unknown.[86] Even in individuals with a relatively low genetic risk, exposure to sufficiently high doses of an addictive drug for a long period of time (e.g., weeks–months) can result in an addiction.[13]
Genetic factors
- See also: Alcoholism#Genetic variation
It has long been established that genetic factors along with environmental (e.g., psychosocial) factors are significant contributors to addiction vulnerability.[13][86] Epidemiological studies estimate that genetic factors account for 40–60% of the risk factors for alcoholism.[87] Similar rates of heritability for other types of drug addiction have been indicated by other studies.[88] Knestler hypothesized in 1964 that a gene or group of genes might contribute to predisposition to addiction in several ways. For example, altered levels of a normal protein due to environmental factors could then change the structure or functioning of specific brain neurons during development. These altered brain neurons could change the susceptibility of an individual to an initial drug use experience. In support of this hypothesis, animal studies have shown that environmental factors such as stress can affect an animal's genotype.[88]
Overall, the data implicating specific genes in the development of drug addiction is mixed for most genes. One reason for this may be that the case is due to a focus of current research on common variants. Many addiction studies focus on common variants with an allele frequency of greater than 5% in the general population; however, when associated with disease, these only confer a small amount of additional risk with an odds ratio of 1.1–1.3 percent. On the other hand, the rare variant hypothesis states that genes with low frequencies in the population (<1%) confer much greater additional risk in the development of the disease.[89]
Genome-wide association studies (GWAS) are used to examine genetic associations with dependence, addiction, and drug use. These studies employ an unbiased approach to finding genetic associations with specific phenotypes and give equal weight to all regions of DNA, including those with no ostensible relationship to drug metabolism or response. These studies rarely identify genes from proteins previously described via animal knockout models and candidate gene analysis. Instead, large percentages of genes involved in processes such as cell adhesion are commonly identified. This is not to say that previous findings, or the GWAS findings, are erroneous. The important effects of endophenotypes are typically not capable of being captured by these methods. Furthermore, genes identified in GWAS for drug addiction may be involved either in adjusting brain behavior prior to drug experiences, subsequent to them, or both.[90]
A study that highlights the significant role genetics play in addiction is the twin studies. Twins have similar and sometimes identical genetics. Analyzing these genes in relation to genetics has helped geneticists understand how much of a role genes play in addiction. Studies performed on twins found that rarely did only one twin have an addiction. In most cases where at least one twin suffered from an addiction, both did, and often to the same substance.[91] Cross addiction is when already has a predisposed addiction and then starts to become addicted to something different. If one family member has a history of addiction, the chances of a relative or close family developing those same habits are much higher than one who has not been introduced to addiction at a young age.[92] In a recent study done by the National Institute on Drug Abuse, from 2002 to 2017, overdose deaths have almost tripled amongst male and females. In 2017, 72,306 overdose deaths happened in the U.S. that were reported.[93]
Environmental factors
Environmental risk factors for addiction are the experiences of an individual during their lifetime that interact with the individual's genetic composition to increase or decrease his or her vulnerability to addiction.[13] A number of different environmental factors have been implicated as risk factors for addiction, including various psychosocial stressors;[13] however, an individual's exposure to an addictive drug is by far the most significant environmental risk factor for addiction.[13] The National Institute on Drug Abuse (NIDA) cites lack of parental supervision, the prevalence of peer substance use, drug availability, and poverty as risk factors for substance use among children and adolescents.[94]
Adverse childhood experiences (ACEs) are various forms of maltreatment and household dysfunction experienced in childhood. The Adverse Childhood Experiences Study by the Centers for Disease Control and Prevention has shown a strong dose–response relationship between ACEs and numerous health, social, and behavioral problems throughout a person's lifespan, including those associated with substance abuse.[95] Children's neurological development can be permanently disrupted when they are chronically exposed to stressful events such as physical, emotional, or sexual abuse, physical or emotional neglect, witnessing violence in the household, or a parent being incarcerated or suffering from a mental illness. As a result, the child's cognitive functioning or ability to cope with negative or disruptive emotions may be impaired. Over time, the child may adopt substance use as a coping mechanism, particularly during adolescence.[95] A study of 900 court cases involving children who experienced abuse found that a vast amount of them went on to suffer from some form of addiction in their adolescence or adult life.[96] This pathway towards addiction that is opened through stressful experiences during childhood can be avoided by a change in environmental factors throughout an individual's life and opportunities of professional help.[96] If one has friends or peers who engage in drug use favorably, the chances of them developing an addiction increases. Family conflict and home management is also a cause for one to become engaged in alcohol or other drug use.[97]
Age
Adolescence represents a period of unique vulnerability for developing an addiction.[98] In adolescence, the incentive-rewards systems in the brain mature well before the cognitive control center. This consequentially grants the incentive-rewards systems a disproportionate amount of power in the behavioral decision-making process. Therefore, adolescents are increasingly likely to act on their impulses and engage in risky, potentially addicting behavior before considering the consequences.[99] Not only are adolescents more likely to initiate and maintain drug use, but once addicted they are more resistant to treatment and more liable to relapse.[100][101]
Statistics have shown that those who start to drink alcohol at a younger age are more likely to become dependent later on. About 33% of the population tasted their first alcohol between the ages of 15 and 17, while 18% experienced it prior to this. As for alcohol abuse or dependence, the numbers start off high with those who first drank before they were 12 and then drop off after that. For example, 16% of alcoholics began drinking prior to turning 12 years old, while only 9% first touched alcohol between 15 and 17. This percentage is even lower, at 2.6%, for those who first started the habit after they were 21.[102]
Most individuals are exposed to and use addictive drugs for the first time during their teenage years.[103] In the United States, there were just over 2.8 million new users of illicit drugs in 2013 (~7,800 new users per day);[103] among them, 54.1% were under 18 years of age.[103] In 2011, there were approximately 20.6 million people in the United States over the age of 12 with an addiction.[104] Over 90% of those with an addiction began drinking, smoking or using illicit drugs before the age of 18.[104]
Comorbid disorders
Individuals with comorbid (i.e., co-occurring) mental health disorders such as depression, anxiety, attention-deficit/hyperactivity disorder (ADHD) or post-traumatic stress disorder are more likely to develop substance use disorders.[105][106][107] The NIDA cites early aggressive behavior as a risk factor for substance use.[94] A study by the National Bureau of Economic Research found that there is a "definite connection between mental illness and the use of addictive substances" and a majority of mental health patients participate in the use of these substances: 38% alcohol, 44% cocaine, and 40% cigarettes.[108]
Epigenetic factors
Transgenerational epigenetic inheritance
Epigenetic genes and their products (e.g., proteins) are the key components through which environmental influences can affect the genes of an individual;[86] they also serve as the mechanism responsible for transgenerational epigenetic inheritance, a phenomenon in which environmental influences on the genes of a parent can affect the associated traits and behavioral phenotypes of their offspring (e.g., behavioral responses to environmental stimuli).[86] In addiction, epigenetic mechanisms play a central role in the pathophysiology of the disease;[13] it has been noted that some of the alterations to the epigenome which arise through chronic exposure to addictive stimuli during an addiction can be transmitted across generations, in turn affecting the behavior of one's children (e.g., the child's behavioral responses to addictive drugs and natural rewards).[86] However, the components that are responsible for the heritability of characteristics that make an individual more susceptible to drug addiction in humans remain largely unknown given that patterns of inheritance cannot be explained by simple genetic mechanisms. [109]
The general classes of epigenetic alterations that have been implicated in transgenerational epigenetic inheritance include DNA methylation, histone modifications, and downregulation or upregulation of microRNAs.[86] With respect to addiction, more research is needed to determine the specific heritable epigenetic alterations that arise from various forms of addiction in humans and the corresponding behavioral phenotypes from these epigenetic alterations that occur in human offspring.[86][109] Based upon preclinical evidence from animal research, certain addiction-induced epigenetic alterations in rats can be transmitted from parent to offspring and produce behavioral phenotypes that decrease the offspring's risk of developing an addiction.[note 4][86] More generally, the heritable behavioral phenotypes that are derived from addiction-induced epigenetic alterations and transmitted from parent to offspring may serve to either increase or decrease the offspring's risk of developing an addiction.[86][109]
Behavioral addictions
Behavioral addiction is a form of addiction that involves a compulsion to engage in an inherently rewarding non-substance-related behavior – sometimes called a "natural reward"[6][10] – despite adverse consequences to the person's physical, mental, social, or financial well-being.[110][2]
Addiction to both drugs and behavioral rewards may arise from similar dysregulation of the mesolimbic dopamine system. Preclinical evidence has demonstrated that marked increases in the expression of ΔFosB through repetitive and excessive exposure to a natural reward induces the same behavioral effects and neuroplasticity as occurs in a drug addiction.[10]
Psychiatric and medical classifications
Diagnostic models do not currently include the criteria necessary to identify behaviors as addictions in a clinical setting.
Behavioral addictions have been introduced as a new diagnostic category in DSM-5, but the only category included is gambling addiction. Internet gaming addiction is included in the appendix as a condition for further study.[111][112]
In September 2019, the American Society of Addiction Medicine (ASAM) issued a public statement defining all addiction in terms of brain changes:
Addiction is a treatable, chronic medical disease involving complex interactions among brain circuits, genetics, the environment, and an individual’s life experiences. People with addiction use substances or engage in behaviors that become compulsive and often continue despite harmful consequences.[1]
The type of excessive behaviors identified as being addictive include gambling, food, chocolate, sexual intercourse, use of pornography, use of computers, playing video games, use of the internet and other digital media, exercise, and shopping.
Gambling provides a natural reward which is associated with compulsive behavior and for which clinical diagnostic manuals, namely the DSM-5, have identified diagnostic criteria for an addiction. In order for a person's gambling behavior to meet criteria of an addiction, it shows certain characteristics, such as mood modification, compulsivity, and withdrawal. There is evidence from functional neuroimaging that gambling activates the reward system and the mesolimbic pathway in particular.[113] Similarly, shopping and playing video games are associated with compulsive behaviors in humans and have also been shown to activate the mesolimbic pathway and other parts of the reward system.[10] Based upon this evidence, gambling addiction, video game addiction, and shopping addiction are classified accordingly.[10][113]
Reviews of both clinical research in humans and preclinical studies involving ΔFosB have identified compulsive sexual activity – specifically, any form of sexual intercourse – as an addiction. Moreover, reward cross-sensitization between amphetamine and sexual activity, meaning that exposure to one increases the desire for both, has been shown to occur preclinically and clinically as a dopamine dysregulation syndrome; ΔFosB expression is required for this cross-sensitization effect, which intensifies with the level of ΔFosB expression.[10]
Reviews of preclinical studies indicate that long-term frequent and excessive consumption of high fat or sugar foods can produce an addiction (food addiction).[10]
Excessive and compulsive Internet use has also been studied, revealing it to be a behavioral addiction with serious psychosocial consequences:
The growing number of researches on Internet addiction indicates that Internet addiction is a psychosocial disorder and its characteristics are as follows: tolerance, withdrawal symptoms, affective disorders, and problems in social relations. Internet usage creates psychological, social, school and/or work difficulties in a person's life. Eighteen percent of study participants were considered to be pathological Internet users, whose excessive use of the Internet was causing academic, social, and interpersonal problems. Excessive Internet use may create a heightened level of psychological arousal, resulting in little sleep, failure to eat for long periods, and limited physical activity, possibly leading to the user experiencing physical and mental health problems such as depression, OCD, low family relationships and anxiety.[114]
Studies on Internet addiction reveal the same fundamental brain changes seen in other addictions.[115][116]
Another growing area is social media addiction. Researchers found that not only is social media (particularly Facebook) itself potentially addictive, those who use it may also be at greater risk for substance abuse.[117]
Treatment
Behavioral addiction is a treatable condition.[118] Treatment options include psychotherapy and psychopharmacotherapy (medications) or a combination of both. Cognitive behavioral therapy (CBT) is the most common form of psychotherapy used in treating behavioral addictions; it focuses on identifying patterns that trigger compulsive behavior and making lifestyle changes to promote healthier behaviors. While CBT does not cure behavioral addiction, it does help with coping with the condition in a healthy way.
Currently, there are no medications approved for treatment of behavioral addictions in general, but some medications used for treatment of drug addiction may also be beneficial with specific behavioral addictions.[113] Any unrelated psychiatric disorders should be kept under control, and differentiated from the contributing factors that cause the addiction.
Epidemiology
Due to cultural variations, the proportion of individuals who develop a drug or behavioral addiction within a specified time period (i.e., the prevalence) varies over time, by country, and across national population demographics (e.g., by age group, socioeconomic status, etc.).[86]
Asia
The prevalence of alcohol dependence is not as high as is seen in other regions. In Asia, not only socioeconomic factors but also biological factors influence drinking behavior.[119]
Europe and Oceania
A 2017 report noted that Eastern Europe had the highest mortality rates for alcohol and illicit drugs, while Oceania had the highest tobacco mortality rates.[120]
United States
Addiction is widespread in the United States. According to a 2017 poll conducted by the Pew Research Center, almost half of US adults know a family member or close friend who has struggled with a drug addiction at some point in their life.[121]
In spite of the massive overall economic cost to society, which is greater than the cost of diabetes and all forms of cancer combined, most doctors in the US lack the training to effectively address a drug addiction.[19] In 2016, it was reported that only about ten percent, or a little over 2 million, receive any form of treatments, and those that do generally do not receive evidence-based care. A major milestone was reached on March 14, 2016, when the American Board of Medical Specialties (ABMS) formally announced recognition of the field of Addiction Medicine as a medical subspecialty:
This landmark event, more than any other, recognizes addiction as a preventable and treatable disease, helping to shed the stigma that has long plagued it. It sends a strong message to the public that American medicine is committed to providing expert care for this disease and services designed to prevent the risky substance use that precedes it.[122]
In 2019, opioid addiction was acknowledged as a national crisis in the United States. American drug companies were found to have flooded the country with prescription pain pills from 2006 through 2012, despite being aware that they were addictive and that they were fueling addiction and overdoses.[123]
South America
The realities of opioid use and abuse in Latin America may be deceptive if observations are limited to epidemiological findings. According to the Inter-American Commission on Drug Abuse Control, consumption of heroin is low in most Latin American countries, although Colombia is the area's largest opium producer. Mexico, because of its border with the United States, has the highest incidence of use.[124]
Notes
- ↑ 1.0 1.1 What is the definition of addiction? American Society of Addiction Medicine. Retrieved June 4, 2020.
- ↑ 2.0 2.1 2.2 2.3 Eric Nestler, Steven Hyman, and Robert Malenka, Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (McGraw-Hill, 2008, ISBN 978-0071481274).
- ↑ Sara B. Taylor, Candace R. Lewis, and M. Foster Olive, The Neurocircuitry of Illicit Psychostimulant Addiction: Acute and Chronic Effects in Humans Subst Abuse Rehabil 8(4) (2013):29-43. Retrieved June 4, 2020.
- ↑ G.A. Marlatt, J.S. Baer, D.M. Donovan, and D.R. Kivlahan, Addictive Behaviors: Etiology and Treatment Annu Rev Psychol 39 (1988): 223–252. Retrieved June 11, 2020.
- ↑ Constance Holden, 'Behavioral' Addictions: Do They Exist? Science 294(5544) (2001): 980–982. Retrieved June 11, 2020.
- ↑ 6.0 6.1 6.2 6.3 Alfred J. Robison and Eric J. Nestler, Transcriptional and Epigenetic Mechanisms of Addiction Nat Rev Neurosci 12(11) (2011):623-637. Retrieved June 11, 2020.
- ↑ 7.0 7.1 7.2 Kenneth Blum et al., Sex, Drugs, and Rock ‘N’ Roll: Hypothesizing Common Mesolimbic Activation as a Function of Reward Gene Polymorphisms Psychoactive Drugs 44(1) (2012):38–55. Retrieved June 11, 2020.
- ↑ Meredith E. Gansner, Gaming Addiction in ICD-11: Issues and Implications Psychiatric Times, September 12, 2019. Retrieved June 11, 2020.
- ↑ Substance-Related and Addictive Disorders Mental Health Gateway. Retrieved June 11, 2020.
- ↑ 10.00 10.01 10.02 10.03 10.04 10.05 10.06 10.07 10.08 10.09 10.10 10.11 Christopher M. Olsen, Natural Rewards, Neuroplasticity, and Non-Drug Addictions Neuropharmacology 61(7) (2011): 1109–1122. Retrieved June 11, 2020.
- ↑ Steven E. Hyman, Robert C. Malenka, and Eric J. Nestler, Neural mechanisms of addiction: the role of reward-related learning and memory Annual review of neuroscience 29 (2006):565–598. Retrieved June 11, 2020.
- ↑ E.J. Nestler, M. Barrot, and D.W. Self, DeltaFosB: A Sustained Molecular Switch for Addiction Proc Natl Acad Sci U S A 98(20) (2001):11042-22046. Retrieved June 11, 2020.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 13.8 13.9 Eric J. Nestler, Cellular basis of memory for addiction Dialogues Clin Neurosci 15(4) (2013): 431–443. Retrieved June 4, 2020.
- ↑ 14.0 14.1 Gaetano Di Chiara and Valentina Bassareo, Reward System and Addiction: What Dopamine Does and Doesn't Do Current Opinion in Pharmacology 7(1) (2007):69–76. Retrieved June 11, 2020.
- ↑ Judson A. Brewer and Marc N. Potenza, The neurobiology and genetics of impulse control disorders: Relationships to drug addictions Biochemical Pharmacology 75(1) (2008):63–75. Retrieved June 11, 2020.
- ↑ Jean-Antoine Girault and Paul Greengard, The Neurobiology of Dopamine Signaling Archives of Neurology 61(5) (2004):641–644. Retrieved June 11, 2020.
- ↑ 17.0 17.1 17.2 17.3 American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5 (American Psychiatric Publishing, 2013, ISBN 978-0890425558).
- ↑ Substance Abuse and Mental Health Services Administration,Substance Use Disorders Impact of the DSM-IV to DSM-5 Changes on the National Survey on Drug Use and Health, 2016. Retrieved June 11, 2020.
- ↑ 19.0 19.1 Dennis Tartaglia, American Board of Medical Specialties Recognizes the New Subspecialty of Addiction Medicine American Board of Addiction Medicine, March 14, 2016. Retrieved June 11, 2020.
- ↑ United Nations Office on Drugs and Crime, International Narcotics Control Board Report: 2013 (United Nations, 2014, ISBN 978-9211482744).
- ↑ Drug addiction (substance use disorder) Mayo Clinic. Retrieved June 12, 2020.
- ↑ Thomas Insel, Transforming Diagnosis National Institute of Mental Health, April 29, 2013. Retrieved June 12, 2020.
- ↑ William H. Hampton, Italia M. Hanik, and Ingrid R. Olson, Substance Abuse and White Matter: Findings, Limitations, and Future of Diffusion Tensor Imaging Research Drug and Alcohol Dependence 197(4) (2019):288–298. Retrieved June 12, 2020.
- ↑ 24.0 24.1 (February 2013) The neurocircuitry of illicit psychostimulant addiction: acute and chronic effects in humans. Subst. Abuse Rehabil. 4: 29–43.
- ↑ (October 2000)Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA 284 (13): 1689–95.
- ↑ (2006). Evidence-Based Practice in Psychology and Behavior Analysis. The Behavior Analyst Today 7 (3): 335–350.
- ↑ (1998). An update on empirically validated therapies. Clinical Psychology 49: 5–14.
- ↑ (2015). [Psychosocial Treatment of Addictive Disorders – An Overview of Psychotherapeutic Options and their Efficacy]. Fortschr Neurol Psychiatr 83 (4): 201–10.
- ↑ (February 2016) Sex Differences in Behavioral Dyscontrol: Role in Drug Addiction and Novel Treatments. Front. Psychiatry 6: 175.
- ↑ 30.0 30.1 30.2 30.3 (September 2013) Exercise as a novel treatment for drug addiction: a neurobiological and stage-dependent hypothesis. Neurosci Biobehav Rev 37 (8): 1622–44.
- ↑ 31.0 31.1 (2015). Exercise-based treatments for substance use disorders: evidence, theory, and practicality. Am J Drug Alcohol Abuse 41 (1): 7–15.
- ↑ 32.0 32.1 (July 2015) Sex differences in drug addiction and response to exercise intervention: From human to animal studies. Front. Neuroendocrinol. 40: 24–41.
- ↑ (July 2012) Opioid addiction and abuse in primary care practice: a comparison of methadone and buprenorphine as treatment options. Journal of the National Medical Association 104 (7–8): 342–50.
- ↑ 34.0 34.1 American Psychiatric Association. (2002). American Psychiatric Association practice guidelines for the treatment of psychiatric disorders.. The Association. ISBN 0-89042-320-2. OCLC 48656105.
- ↑ Massachusetts. Center for Health Information and Analysis, issuing body.. Access to substance use disorder treatment in Massachusetts. OCLC 911187572.
- ↑ Holt, Dr. Harry (2019-07-15). Stigma Associated with Opioid Use Disorder and Medication Assisted Treatment.
- ↑ (May 2013) Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995-2009. American Journal of Public Health 103 (5): 917–22.
- ↑ Administration (US), Substance Abuse and Mental Health Services (November 2016). EARLY INTERVENTION, TREATMENT, AND MANAGEMENT OF SUBSTANCE USE DISORDERS. US Department of Health and Human Services.
- ↑ Sachdeva A, Choudhary M, Chandra M. (Sep 2015) "Alcohol Withdrawal Syndrome: Benzodiazepines and Beyond." PMID: 26500991
- ↑ (December 2006) New pharmacological approaches for the treatment of alcoholism. Expert Opinion on Pharmacotherapy 7 (17): 2341–53.
- ↑ (October 2006) Choosing the right medication for the treatment of alcoholism. Current Psychiatry Reports 8 (5): 383–88.
- ↑ (July 2004) Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: a systematic review. Addiction 99 (7): 811–28.
- ↑ (November 2005) Medications for treating alcohol dependence. American Family Physician 72 (9): 1775–80.
- ↑ (December 2010) Opioid antagonists for alcohol dependence. The Cochrane Database of Systematic Reviews (12): CD001867.
- ↑ (April 2010) Cognitive function as an emerging treatment target for marijuana addiction. Exp Clin Psychopharmacol 18 (2): 109–19.
- ↑ (August 2013) Molecular mechanisms of cannabinoid addiction. Curr. Opin. Neurobiol. 23 (4): 487–92.
- ↑ 47.0 47.1 (2007). Emerging pharmacotherapies for smoking cessation. Am J Health Syst Pharm 64 (16): 1693–98.
- ↑ 48.0 48.1 (2014) Nicotinic receptor antagonists as treatments for nicotine abuse, Advances in Pharmacology, 513–51. DOI:10.1016/B978-0-12-420118-7.00013-5. ISBN 978-0-12-420118-7.
- ↑ (2000). A comparison of levomethadyl acetate, buprenorphine, and methadone for opioid dependence. N. Engl. J. Med. 343 (18): 1290–97.
- ↑ (2007). Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation. Health Technol Assess 11 (9): 1–171, iii–iv.
- ↑ (2005). Predictors of outcome in LAAM, buprenorphine, and methadone treatment for opioid dependence. Exp Clin Psychopharmacol 13 (4): 293–302.
- ↑ (2006). Addressing the efficacy of dihydrocodeine versus methadone as an alternative maintenance treatment for opiate dependence: A randomized controlled trial. Addiction 101 (12): 1752–59.
- ↑ Qin Bo-Yi (1998). Advances in dihydroetorphine: From analgesia to detoxification. Drug Development Research 39 (2): 131–34. Link
- ↑ (1998). Feasibility of prescribing injectable heroin and methadone to opiate-dependent drug users: associated health gains and harm reductions. Med. J. Aust. 168 (12): 596–600.
- ↑ (2007). Pathways into receiving a prescription for diamorphine (heroin) for the treatment of opiate dependence in the United kingdom. Eur Addict Res 13 (3): 144–47.
- ↑ (2007). Pharmacotherapy of dual substance abuse and dependence. CNS Drugs 21 (3): 213–37.
- ↑ Strang J, McCambridge J. (May 2003) "Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study" PMID: 12727768
- ↑ (May 2014) Combination pharmacotherapies for stimulant use disorder: a review of clinical findings and recommendations for future research. Expert Rev Clin Pharmacol 7 (3): 363–74.
- ↑ (September 2013) Efficacy of psychostimulant drugs for amphetamine abuse or dependence. Cochrane Database Syst. Rev. 9 (9): CD009695.
- ↑ (February 2014) Future pharmacological treatments for substance use disorders. Br. J. Clin. Pharmacol. 77 (2): 382–400.
- ↑ 61.0 61.1 (February 2016) "TAARgeting Addiction" – The Alamo Bears Witness to Another Revolution: An Overview of the Plenary Symposium of the 2015 Behavior, Biology and Chemistry Conference. Drug Alcohol Depend. 159: 9–16.
- ↑ 62.0 62.1 (August 2015) Trace amine-associated receptor 1: A promising target for the treatment of psychostimulant addiction. Eur. J. Pharmacol. 761: 345–52.
- ↑ 63.0 63.1 (December 2018) Drug addiction: a curable mental disorder?. Acta Pharmacologica Sinica 39 (12): 1823–1829.
- ↑ 64.0 64.1 64.2 (November 2015) Is immunotherapy an opportunity for effective treatment of drug addiction?. Vaccine 33 (48): 6545–51.
- ↑ (June 2015) The frequency of naive and early-activated hapten-specific B cell subsets dictates the efficacy of a therapeutic vaccine against prescription opioid abuse. J. Immunol. 194 (12): 5926–36.
- ↑ Painter A. (2019) "Researchers working to develop vaccines to fight opioid addiction" Vtnews.vt.edu
- ↑ 67.0 67.1 67.2 67.3 (March 2016) Advances and challenges in pharmacotherapeutics for amphetamine-type stimulants addiction. Eur. J. Pharmacol. 780: 129–35.
- ↑ 68.0 68.1 (February 2016) Neuroimaging markers of glutamatergic and GABAergic systems in drug addiction: Relationships to resting-state functional connectivity. Neurosci Biobehav Rev 61: 35–52.
- ↑ (April 2015) [GABAB receptor as therapeutic target for drug addiction: from baclofen to positive allosteric modulators]. Psychiatr. Pol. 49 (2): 215–23.
- ↑ (January 2015) GABAB receptors as a therapeutic strategy in substance use disorders: focus on positive allosteric modulators. Neuropharmacology 88: 36–47.
- ↑ 71.0 71.1 (February 2015) The Epigenetic Mechanisms of Amphetamine. J. Addict. Prev. 2015 (Suppl 1).
- ↑ 72.0 72.1 72.2 72.3 (February 2015) Regulation of chromatin states by drugs of abuse. Curr. Opin. Neurobiol. 30: 112–21.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedG9a reverses ΔFosB plasticity - ↑ 74.0 74.1 74.2 (January 2014) Epigenetic mechanisms of drug addiction. Neuropharmacology 76 Pt B: 259–68.
- ↑ 75.0 75.1 Primary references involving sodium butyrate:
Template:Bull (April 2013) Class I HDAC inhibition blocks cocaine-induced plasticity by targeted changes in histone methylation. Nat. Neurosci. 16 (4): 434–40.
Template:Bull (July 2015) The histone deacetylase inhibitor sodium butyrate decreases excessive ethanol intake in dependent animals. Addict Biol 20 (4): 676–89.
Template:Bull (April 2015) Inhibition of histone deacetylases facilitates extinction and attenuates reinstatement of nicotine self-administration in rats. PLOS One 10 (4): e0124796. - ↑ (August 2015) Molecular mechanisms of synaptic remodeling in alcoholism. Neurosci. Lett. 601: 11–19.
- ↑ (2016) Effect of add-on valproate on craving in methamphetamine depended patients: A randomized trial. Advanced Biomedical Research 5: 149.
- ↑ Gene Therapy For Addiction: Flooding Brain With 'Pleasure Chemical' Receptors Works On Cocaine, As On Alcohol.
- ↑ Abuse, National Institute on Drug (14 January 2016). Gene Transfer Therapy for Cocaine Addiction Passes Tests in Animals.
- ↑ (2014). Physiologic and metabolic safety of butyrylcholinesterase gene therapy in mice. Vaccine 32 (33): 4155–62.
- ↑ Using Adeno-Associated Virus (AAV) Mediated Sustained Expression of an Anti-methamphetamine Antibody Fragment to Alter Methamphetamine Disposition in Mice.
- ↑ ATTC – Addiction Science Made Easy.
- ↑ 83.0 83.1 83.2 Ferri, Fred (2019). Ferri's Clinical Advisor. Elsevier.
- ↑ (April 2014) Personality traits and vulnerability or resilience to substance use disorders. Trends in Cognitive Sciences 18 (4): 211–7.
- ↑ (2019) Personality Traits and Drug Consumption. A Story Told by Data. Springer, Cham. DOI:10.1007/978-3-030-10442-9. ISBN 978-3-030-10441-2.
- ↑ 86.00 86.01 86.02 86.03 86.04 86.05 86.06 86.07 86.08 86.09 86.10 86.11 86.12 86.13 86.14 86.15 F.M. Vassoler and G. Sadri-Vakili, Mechanisms of transgenerational inheritance of addictive-like behaviors Neuroscience 264 (2014): 198–206. Retrieved May 29, 2020.
- ↑ Mayfield RD, Harris RA,1, Schuckit MA (May 2008) "Genetic factors influencing alcohol dependence" PMID 18362899
- ↑ 88.0 88.1 (May 1994) A twin-family study of alcoholism in women. Am J Psychiatry 151 (5): 707–15.
- ↑ (2013). Low frequency genetic variants in the μ-opioid receptor (OPRM1) affect risk for addiction to heroin and cocaine. Neuroscience Letters 542: 71–75.
- ↑ (December 2013) Implications of genome wide association studies for addiction: Are our a priori assumptions all wrong?. Pharmacology & Therapeutics 140 (3): 267–79.
- ↑ Genetics of alcoholism. Alcohol Health and Research World: 1–11.
- ↑ Life, Dr. Steven Melemis, I Want to Change My, "The Genetics of Addiction – Is Addiction a Disease?", I Want to Change My Life.
- ↑ Abuse, National Institute on Drug, "Overdose Death Rates", 9 August 2018.
- ↑ 94.0 94.1 Abuse, National Institute on Drug, "What are risk factors and protective factors?".
- ↑ 95.0 95.1 Adverse Childhood Experiences. Substance Abuse and Mental Health Services Administration. Retrieved 26 September 2016.
- ↑ 96.0 96.1 (2011). The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology 214 (1): 17–31.
- ↑ Environmental Risk Factors.
- ↑ (June 2000) The adolescent brain and age-related behavioral manifestations. Neuroscience and Biobehavioral Reviews 24 (4): 417–63.
- ↑ (April 2014) Neurobiology of adolescent substance use and addictive behaviors: treatment implications. Adolescent Medicine 25 (1): 15–32.
- ↑ (1990). Evaluation of the effectiveness of adolescent drug abuse treatment, assessment of risks for relapse, and promising approaches for relapse prevention. The International Journal of the Addictions 25 (9A–10A): 1085–140.
- ↑ (November 2008) Practitioner review: adolescent alcohol use disorders: assessment and treatment issues. Journal of Child Psychology and Psychiatry, and Allied Disciplines 49 (11): 1131–54.
- ↑ Age and Substance Abuse – Alcohol Rehab.
- ↑ 103.0 103.1 103.2 Nationwide Trends. National Institute on Drug Abuse (June 2015). Retrieved 15 December 2017.
- ↑ 104.0 104.1 "Addiction Statistics – Facts on Drug and Alcohol Addiction", AddictionCenter.
- ↑ SAMHSA. Risk and Protective Factors. Substance Abuse and Mental Health Administration.
- ↑ Infographic – Risk Factors of Addiction | Recovery Research Institute.
- ↑ Drug addiction Risk factors – Mayo Clinic.
- ↑ "The Connection Between Mental Illness and Substance Abuse | Dual Diagnosis", Dual Diagnosis.
- ↑ 109.0 109.1 109.2 (2015). Transgenerational Inheritance of Paternal Neurobehavioral Phenotypes: Stress, Addiction, Ageing and Metabolism. Mol. Neurobiol. 53 (9): 6367–76.
- ↑ Dan J. Stein, Eric Hollander, and Barbara O. Rothbaum (eds.), Textbook of Anxiety Disorders (American Psychiatric Publishing, Inc., 2009, ISBN 978-1585622542).
- ↑ (2013). Internet gaming addiction: current perspectives. Psychology Research and Behavior Management 6 (6): 125–137.
- ↑ Is your child a gaming addict?.
- ↑ 113.0 113.1 113.2 Jon E. Grant, Marc N. Potenza, Aviv Weinstein, and David A. Gorelick, Introduction to Behavioral Addictions Am J Drug Alcohol Abuse 36(5) (2010):233-241. Retrieved June 11, 2020.
- ↑ Seyyed Salman Alavi, Mohammad Reza Maracy, Fereshte Jannatifard, and Mehdi Eslami, The effect of psychiatric symptoms on the internet addiction disorder in Isfahan's University students J Res Med Sci. 16(6) (2011):793–800. Retrieved June 11, 2020.
- ↑ Fuchun Lin, Yan Zhou, Yasong Du, Lindi Qin, Zhimin Zhao, Jianrong Xu, and Hao Lei, Abnormal White Matter Integrity in Adolescents with Internet Addiction Disorder: A Tract-Based Spatial Statistics Study PLoS One 7(1) (2012). Retrieved June 11, 2020.
- ↑ Sang Hee Kim, Sang-Hyun Baik, Chang Soo Park, Su Jin Kim, Sung Won Choi, and Sang Eun Kim, Reduced Striatal Dopamine D2 Receptors in People With Internet Addiction Neuroreport 22(8) (2011):407-411. Retrieved June 11, 2020.
- ↑ Craving Facebook? UAlbany Study Finds Social Media to be Potentially Addictive, Associated with Substance Abuse News Center, University at Albany, State University of New York, December 9, 2014. Retrieved June 11, 2020.
- ↑ Jon Grant, Impulse Control Disorders: A Clinician's Guide to Understanding and Treating Behavioral Addictions (W. W. Norton & Company, 2008, ISBN 978-0393705218).
- ↑ Chiao-Chicy Chen and Shih-Jiun Yin, Alcohol abuse and related factors in Asia Int. Rev. Psychiatry 20(5) (2008):425-433. PubMed Retrieved May 29, 2020.
- ↑ Amy Peacock et al., Global Statistics on Alcohol, Tobacco and Illicit Drug Use: 2017 Status Report Addiction 113(10) (2018):1905-1926. Retrieved June 11, 2020.
- ↑ John Gramlich, Nearly half of Americans have a family member or close friend who's been addicted to drugs Pew Research Center, October 26, 2017. Retrieved June 11, 2020.
- ↑ Nora Volkow, A Major Step Forward for Addiction Medicine National Institute on Drug Abuse, March 31, 2016. Retrieved June 11, 2020.
- ↑ Katelyn Newman, Amid Opioid Crisis, Large Drug Companies Pushed 76 Billion Pain Pills Across U.S. US News & World Report, July 17, 2019. Retrieved June 11, 2020.
- ↑ Pacurucu Castillo, José Marcelo, Adrián Hernández, and Renato D. Alarcón, World Opioid and Substance Use Epidemic: A Latin American Perspective Psychiatry Online.org, January 24, 2019. Retrieved June 11, 2020.
ReferencesISBN links support NWE through referral fees
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. American Psychiatric Publishing, 2013. ISBN 978-0890425558
- Grant, Jon. Impulse Control Disorders: A Clinician's Guide to Understanding and Treating Behavioral Addictions. W. W. Norton & Company, 2008. ISBN 978-0393705218
- Nestler, Eric, Steven Hyman, and Robert Malenka. Molecular Neuropharmacology: A Foundation for Clinical Neuroscience. McGraw-Hill, 2008. ISBN 978-0071481274
- Stein, Dan J., Eric Hollander, and Barbara O. Rothbaum (eds.). Textbook of Anxiety Disorders. American Psychiatric Publishing, Inc., 2009. ISBN 978-1585622542
- Szalavitz, Maia. Unbroken Brain. Picador, 2017. ISBN 978-1250116444
- United Nations Office on Drugs and Crime. International Narcotics Control Board Report: 2013. United Nations, 2014. ISBN 978-9211482744
External links
All links retrieved
- The Science of Addiction: Genetics and the Brain
- Nora Volkow, Why do our brains get addicted? TEDMED.
- Kyoto Encyclopedia of Genes and Genomes (KEGG) signal transduction pathways:
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.
Cite error: <ref> tags exist for a group named "note", but no corresponding <references group="note"/> tag was found