Difference between revisions of "Mammary gland" - New World Encyclopedia
| Line 12: | Line 12: | ||
== Development and Hormonal Control == | == Development and Hormonal Control == | ||
| − | The proliferation and differentiation of the mammary gland involves a variety of growth factors and hormones such as estrogen, | + | The proliferation and differentiation of the mammary gland involves a variety of growth factors and hormones such as [[estrogen]], [[progesterone]], and [[prolactin]]. Based on the development of mammary glands in mouse models, researchers at [http://mammary.nih.gov/ NIH's Mammary Genome Anatomy Project] have defined seven stages of growth: embryonic, postnatal, juvenile, puberty, pregnancy, lactation, and involution. |
| − | *'''Embryonic''': Early indication of mammary gland formation is detected in | + | *'''Embryonic''': Early indication of mammary gland formation is detected in [[embryo]]s. Several mammary ducts, and a fat pad to support the development of the mammary epithelium into ductal and lobular units, are present at birth. |
*'''Postnatal''': Mammary ducts elongate and branch isometrically, keeping pace with the body's growth. | *'''Postnatal''': Mammary ducts elongate and branch isometrically, keeping pace with the body's growth. | ||
| − | *'''Juvenile''': The mammary gland's growth rate exceeds the isometric rate it followed previously. Terminal end buds, which are highly proliferative structures located at the tips of ductal branches, penetrate the stromal fat pad and expand greatly. The terminal end buds are composed of two distinct cell types: cap cells and body cells. | + | *'''Juvenile''': The mammary gland's growth rate exceeds the isometric rate it followed previously. Terminal end buds, which are highly proliferative structures located at the tips of ductal branches, penetrate the stromal fat pad and expand greatly. The terminal end buds are composed of two distinct cell types: cap cells and body cells. The cap cells make up the outermost layer of the end bud and actually interact with the surrounding stroma, whereas the body cells fill the interior of the end bud. During this juvenile period, a large amount of [[apoptosis]] (programmed cell death) occurs in the body cells of the end buds. Interestingly, researchers have observed that apoptosis is an important mechanism in ductal [[morphogenesis]] (differentiation and growth of the organ). |
| − | *'''Puberty''': Although mammary glands exist in both sexes, they remain rudimentary until [[puberty]] when, in response to [[ovarian]] hormones, they begin to develop in the female. | + | *'''Puberty''': Although mammary glands exist in both sexes, they remain rudimentary until [[puberty]] when, in response to [[ovarian]] hormones, they begin to develop in the female. Estrogen promotes formation, while [[testosterone]] inhibits it. Estrogen stimulates proliferation of the ductal system within the stroma and elongation of the ducts into spherical masses of cells that will become secretory alveoli during pregnancy. |
*'''Pregnancy''': About 50 percent of the total growth of the mammary glands occurs during pregnancy until term. Under the influences of estrogen and other [[placental]] hormones, mammary ducts undergo a period of extensive and rapid branching and differentiation. The mammary epithelium also expands vastly in order to fill in the stroma between the ducts. However, milk secretion is repressed by high concentrations of circulating [[sex]] [[steroids]], primarily [[progesterone]]. [[Colostrum]], also called "foremilk," is the thin yellowish fluid rich in antibodies and minerals that is secreted by the mammary glands during late pregnancy and the first few days after giving birth. Colostrum precedes true milk secretion. | *'''Pregnancy''': About 50 percent of the total growth of the mammary glands occurs during pregnancy until term. Under the influences of estrogen and other [[placental]] hormones, mammary ducts undergo a period of extensive and rapid branching and differentiation. The mammary epithelium also expands vastly in order to fill in the stroma between the ducts. However, milk secretion is repressed by high concentrations of circulating [[sex]] [[steroids]], primarily [[progesterone]]. [[Colostrum]], also called "foremilk," is the thin yellowish fluid rich in antibodies and minerals that is secreted by the mammary glands during late pregnancy and the first few days after giving birth. Colostrum precedes true milk secretion. | ||
*'''Lactation''': Lactation, the manufacturing and secretion of milk, is induced by a decrease in estrogen and progesterone levels. Mammary epithelial proliferation carries on until early lactation, contributing to about the 20 percent of total mammary growth that occurs during the beginning of lactation. During lactation, milk is secreted more or less continuously into the alveolar spaces and stored there until the baby's suckling brings about the contraction of the myoepithelial cells. The hormones involved in the maintenance of lactation are [[prolactin]], [[insulin]], and [[glucocorticoid]]. | *'''Lactation''': Lactation, the manufacturing and secretion of milk, is induced by a decrease in estrogen and progesterone levels. Mammary epithelial proliferation carries on until early lactation, contributing to about the 20 percent of total mammary growth that occurs during the beginning of lactation. During lactation, milk is secreted more or less continuously into the alveolar spaces and stored there until the baby's suckling brings about the contraction of the myoepithelial cells. The hormones involved in the maintenance of lactation are [[prolactin]], [[insulin]], and [[glucocorticoid]]. | ||
*'''Involution''': After weaning, when the baby is no longer in need of nourishment through suckling, lactation ceases, and the mammary gland involutes. During involution [[gene]] [[expression]] of the milk-manufacturing protein is suspended, mammary alveolar structures collapse, and secretory epithelial cells are removed through apoptosis and [[phagocytosis]]. | *'''Involution''': After weaning, when the baby is no longer in need of nourishment through suckling, lactation ceases, and the mammary gland involutes. During involution [[gene]] [[expression]] of the milk-manufacturing protein is suspended, mammary alveolar structures collapse, and secretory epithelial cells are removed through apoptosis and [[phagocytosis]]. | ||
| − | During each | + | During each pregnancy, the above developmental sequence repeats itself as described. |
== Lactogenesis: The Transition from Pregnancy to Lactation== | == Lactogenesis: The Transition from Pregnancy to Lactation== | ||
| − | Lactogenesis is defined as the onset of milk secretion. Based on studies done by Hartmann (1973) and Linzell and | + | Lactogenesis is defined as the onset of milk secretion. Based on studies done by Hartmann (1973) and Linzell and colleagues (Fleet et al, 1975), lactogenesis has been divided into two stages. The first stage of lactogenesis is when the gland becomes differentiated enough to secrete small quantities of specific milk components such as [[casein]] and [[lactose]]. Lactogenesis Stage Two occurs after [[parturition]] (childbirth) and has to do with the onset of copious milk secretion. A completely differentiated mammary epithelium is necessary for Stage Two to occur. In humans, this highest stage of differentiation is reached around mid-pregnancy. |
| − | Although mammary epithelial cells are primarily responsible for converting precursors from the blood and [[interstitial fluid]] (fluid in the spaces between the tissue cells) into milk constituents and transporting them to the alveoli where milk is stored, other cells are also involved in milk production. As has already been mentioned, myoepithelial cells contract to eject milk from the breast. Additional types of cells are found within the stroma in which the mammary ducts and alveoli are embedded. Mammary stroma contains | + | Although mammary epithelial cells are primarily responsible for converting precursors from the blood and [[interstitial fluid]] (fluid in the spaces between the tissue cells) into milk constituents and transporting them to the alveoli where milk is stored, other cells are also involved in milk production. As has already been mentioned, myoepithelial cells contract to eject milk from the breast. Additional types of cells are found within the stroma in which the mammary ducts and alveoli are embedded. Mammary stroma contains [[fibroblast]]s, [[adipocyte]]s, [[plasma cell]]s, and [[blood vessel]]s. Fibroblasts are cells that give rise to connective tissue, adipocytes are cells specialized for the storage of fat, and plasma cells are the [[antibody]]-secreting cells of the [[immune]] system. Blood vessels comprise the [[arteries]], [[veins]], and [[capillaries]] through which blood circulates. Specifically though, stromal fibroblasts and adipocytes have been found to be the source of [[growth factors]] such as [[hepatic growth factor]] and [[IGF-1]], and are also responsible for the production of the [[enzyme]] [[lipoprotein lipase]] which is important in milk [[lipid]] synthesis. Plasma cells are more specifically responsible for producing [[immunoglobulins]] (specific antibodies) that make their way into the milk during lactation. The mammary epithelium is therefore the master integrator that coordinates the activities of a variety of cells in order to produce the nutrient-rich milk. |
| − | Before actual | + | Before actual lactogenesis, in the early post-partum period, the mammary gland secretes colostrum. This fluid is composed of high concentrations of immunoglobulins and the protective protein [[lactoferrin]], which retards bacterial and fungal growth. In species such as [[ruminants]] (cattle, sheep, goats, deer, giraffes etc.) that lack transplancental transport of immunoglobulins, colostrum provides immune protection to the young while their immune system begins to mature. In humans however, where transplancental transport of immunoglobulins does occur, colostrum in the early post-partum period is important in protecting mucosal surfaces from infection, especially under conditions where optimal sanitation cannot be maintained. |
| − | The composition of human milk during the first week post-partum undergoes a progression of changes. These events begin with the closure of [[tight junctions]] between epithelial cells. The first chemical changes to occur in the production of mature milk is the decrease in [[sodium]] (Na) and [[chloride]] (Cl) concentrations and an increase in lactose | + | The composition of human milk during the first week post-partum undergoes a progression of changes. These events begin with the closure of [[tight junctions]] between epithelial cells. The first chemical changes to occur in the production of mature milk is the decrease in [[sodium]] (Na) and [[chloride]] (Cl) concentrations and an increase in lactose concentration. These modifications are largely complete by 72 hours postpartum (Neville et al, 1991). With the closure of tight junctions, paracellular pathways are blocked, and lactose, made by epithelial cells, can no longer pass into the plasma, while sodium and chloride can no longer pass from the interstitial fluid into the alveolar sacs. The next change is a transient increase in the rates of [[secretory Immunoglobulin A (sIgA)]] and lactoferrin secretion. The concentration of these two important protective proeteins comprise as much as ten percent by weight of the milk. Then, starting about 36 hours postpartum, there is a ten-fold increase in milk volume from about 50 ml/day to 500 ml/day. This volume increase is brought about by a massive increase in the rates of synthesis and secretion of most of the components of mature milk including lactose, casein, [[alpha-lactalbumin]], lipid, [[calcium]], [[potassium]], etc. Finally, the concentrations of sIgA and lactoferrin fall rapidly after about 48 hours due to a decrease in their absolute rate of secretion, and dilution as milk volume secretion increases. |
| − | The profound and rapid series of changes in the activity of differentiated mammary cells that is lactogenesis is complete by about day | + | The profound and rapid series of changes in the activity of differentiated mammary cells that is lactogenesis is complete by about day five postpartum. It is becoming increasingly clear to scientists that breast milk is the most appropriate source of [[nutrition]] up to the age of six months. Most components of human milk including lactoferrin, growth factors, [[long chain polyunsaturated fatty acids]], [[bile salt stimulated lipase]], and [[anti-infectious oligossacchardies and glycoconjugates]] are not duplicated in the cow's milk often used as an alternative. |
==Oxytocin and Milk Ejection== | ==Oxytocin and Milk Ejection== | ||
| − | Milk is ejected from the breast by the contraction of myoepithelial cells which form a basket-like network around the alveoli where the milk is stored. In order for myoepithelial cells to contract and expell milk from the alveoli into the ducts and the sub-areolar sinuses, the cells must be activated by the hormone oxytocin. Oxytocin is carried through the blood stream to the | + | Milk is ejected from the breast by the contraction of myoepithelial cells which form a basket-like network around the alveoli where the milk is stored. In order for myoepithelial cells to contract and expell milk from the alveoli into the ducts and the sub-areolar sinuses, the cells must be activated by the hormone oxytocin. Oxytocin is carried through the blood stream to the mammary gland where it interacts with specific receptors on myoepithelial cells, signaling their shortening and widening of the ducts to allow free flow of milk to the nipple. The release of oxytocin into the [[blood stream]] however, is caused by the baby's suckling. In humans, milk ejection can be noted subjectively by the mother as a "tingling sensation" in the breast. The myoepithelial contractions causing this sensation last about one minute and occur with a frequency of four to ten contractions per ten minutes. |
| − | When the baby suckles the | + | When the baby suckles the mother's nipple, nerve terminals in the areolus (the pigmented area surrounding the nipple) are stimulated and send information about suckling to the [[central nervous system]]: the [[spinal cord]] and the [[brain]]. Once the sensory information passes through the spinal cord, it travels through a part of the brain called the [[hypothalamus]] and then down to the [[pituitary gland]], which releases oxytocin into the blood. The pituitary gland is nestled in a depression at the bottom of the skull just over the back of the roof of the mouth. It is attached by a stalk to the hypothalamus, which is in volved in many homeostatic regulatory systems. The pituitay gland has two distinct parts: the [[posterior pituitary]] and the [[anterior pituitary]]. The posterior pituitary releases two [[peptide]] hormones, one being oxtocin, and other [[antidiuretic hormone]] (ADH). But these two hormones are actually synthesized in neurons in the hypothalamus, and are therefore called "neurohormones". When oxytocin is produced in the hypothalamus, it is packaged in [[vesicles]], and then transported down long extensions of the neurons, called [[axons]] that run from the hypothalamus, through the pituitary stalk, and into the posterior pituitary. There, the vesicles are stored in axon terminals until a [[nerve impulse]], such as the baby's suckling, stimulates their release of oxytocin into the blood stream. Sometimes just the sights and the sounds of the baby can be enough for the mother to secrete oxytocin and release milk from her breasts. |
| − | In addition to its action on the mammary glands, oxytocin causes uterine contractions. When a woman is about to give birth, the contractions of the uterus that deliver the baby are caused by oxytocin released by the posterior pituitary . Furthermore, women who breastfeed their infants soon after delivery often experience uterine cramping. Finally, there is mounting evidence that oxytocin is involved in a positive feedback loop in | + | In addition to its action on the mammary glands, oxytocin causes uterine contractions. When a woman is about to give birth, the contractions of the uterus that deliver the baby are caused by oxytocin released by the posterior pituitary. Furthermore, women who breastfeed their infants soon after delivery often experience uterine cramping. Finally, there is mounting evidence that oxytocin is involved in a positive feedback loop in wich it facilitates the release of prolactin. Prolactin stimulates the production and secretion of milk. |
| − | Emotional input has been found to have an effect on oxytocin release. In 1948 Newtown and Newtown proved that psychological stress and pain decreased milk output (Newton & Newton, 1948). In relaxed, undisturbed women however, oxytocin release begins | + | Emotional input has been found to have an effect on oxytocin release. In 1948 Newtown and Newtown proved that psychological stress and pain decreased milk output (Newton & Newton, 1948). In relaxed, undisturbed women however, oxytocin release begins with the onset of suckling or even before suckling when the infant cries or becomes restless (McNeilly et al., 1983). |
==Breast cancer== | ==Breast cancer== | ||
Revision as of 19:55, 6 August 2006
Mammary glands are the organs in female mammals that produce and secrete milk for the nourishment of newborn mammalian offspring. Milk is a rich substace composed of proteins, lipids, sugars, and water. In general, a gland is a group of cells or an organ that produces a secretion for use elsewhere in the body, in a body cavity, or for elimination from the body. Mammary glands are part of the exocrine system, which is comprised of ducts such as the salivary gland (which secretes saliva) that secrete extrnally. Furthermore, mammary glands are enlarged and modified sweat glands, and are characteristic of the mammalia class which gave the mammary glands their name. Because of its unique developmental aspects and complex regulation by hormones and growth factors, the mammary gland has been especially important for scientists and researchers. Additionally, since the mammary gland is a target of viral, chemical, and physical carcinogens, the organ has allowed for an array of complex models for neoplastic (tumor) development.
Structure
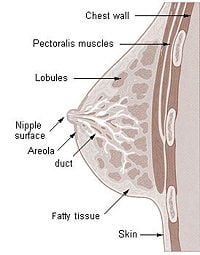
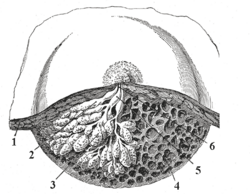
In contrast to most mammalian organs, the mammary gland undergoes most of its development postpubertally, in the adult organism. The mammary gland is made up of two components, the parenchyma, and the surrounding stroma. The parenchyma is the tissue performing the special function of the organ, and the stroma is the connective tissue framework of the organ. The stroma provides a frame of support as well as the material within which the parenchyma can grow and function. The parenchyma consists of the alveoli, grape-like clusters where milk is stored, and 10 to 15 branching ducts, which are tubular canals carrying gladular secretions. Each duct serves a particular lobule. The branching ducts are comprised of two types of cells: inner epithelial cells, which produce milk, and an outer later of myoepithelial cells. Myoepithelial cells are usually large, contractile cells that operate at the base of the secretory cells of glands. The branching, or lactiferous, ducts themselves merge into a primary duct, which drains into the openings of the nipple. This draining is actually the responsibility of the myoepithelial cells, which, when they contract, shorten and widen the ducts, pushing milk through the lactiferous ducts, into the primary duct, and towards the nipple where it collects in the widenings of the ducts, the sinuses. A suckling baby essentially squeezes the milk out of these sinuses. Finally, the nipple is surrounded by an area of pigmented skin, the areola, which contains sebaceous glands (which secrete fat) and sweat glands. The areola is the termination point for the fourth intercostal nerve, which sends sensory information about sucking to the spinal cord and the brain.
Function
The function of the mammary glands in female breasts is to nurture the young by producing milk, which is secreted by the nipples during lactation. However, zoologists point out that no female mammal other than the human has breasts of comparable size when not lactating and that humans are the only primate that have permanently swollen breasts. This suggests that the external form of the breasts is connected to factors other than lactation alone. The mammary glands that secrete the milk from the breasts actually make up a relatively small fraction of the overall breast tissue, and it is commonly assumed by biologists that the breasts serve as a secondary sex characteristic involved in attraction. Others believe that the human breast evolved in order to prevent infants from suffocating while feeding. Since human infants do not have a protruding jaw like other primates, a flat female chest would block the the infant's nose during suckling. According to this theory, as the human jaw recessed over time, the breasts became larger to compensate.
Development and Hormonal Control
The proliferation and differentiation of the mammary gland involves a variety of growth factors and hormones such as estrogen, progesterone, and prolactin. Based on the development of mammary glands in mouse models, researchers at NIH's Mammary Genome Anatomy Project have defined seven stages of growth: embryonic, postnatal, juvenile, puberty, pregnancy, lactation, and involution.
- Embryonic: Early indication of mammary gland formation is detected in embryos. Several mammary ducts, and a fat pad to support the development of the mammary epithelium into ductal and lobular units, are present at birth.
- Postnatal: Mammary ducts elongate and branch isometrically, keeping pace with the body's growth.
- Juvenile: The mammary gland's growth rate exceeds the isometric rate it followed previously. Terminal end buds, which are highly proliferative structures located at the tips of ductal branches, penetrate the stromal fat pad and expand greatly. The terminal end buds are composed of two distinct cell types: cap cells and body cells. The cap cells make up the outermost layer of the end bud and actually interact with the surrounding stroma, whereas the body cells fill the interior of the end bud. During this juvenile period, a large amount of apoptosis (programmed cell death) occurs in the body cells of the end buds. Interestingly, researchers have observed that apoptosis is an important mechanism in ductal morphogenesis (differentiation and growth of the organ).
- Puberty: Although mammary glands exist in both sexes, they remain rudimentary until puberty when, in response to ovarian hormones, they begin to develop in the female. Estrogen promotes formation, while testosterone inhibits it. Estrogen stimulates proliferation of the ductal system within the stroma and elongation of the ducts into spherical masses of cells that will become secretory alveoli during pregnancy.
- Pregnancy: About 50 percent of the total growth of the mammary glands occurs during pregnancy until term. Under the influences of estrogen and other placental hormones, mammary ducts undergo a period of extensive and rapid branching and differentiation. The mammary epithelium also expands vastly in order to fill in the stroma between the ducts. However, milk secretion is repressed by high concentrations of circulating sex steroids, primarily progesterone. Colostrum, also called "foremilk," is the thin yellowish fluid rich in antibodies and minerals that is secreted by the mammary glands during late pregnancy and the first few days after giving birth. Colostrum precedes true milk secretion.
- Lactation: Lactation, the manufacturing and secretion of milk, is induced by a decrease in estrogen and progesterone levels. Mammary epithelial proliferation carries on until early lactation, contributing to about the 20 percent of total mammary growth that occurs during the beginning of lactation. During lactation, milk is secreted more or less continuously into the alveolar spaces and stored there until the baby's suckling brings about the contraction of the myoepithelial cells. The hormones involved in the maintenance of lactation are prolactin, insulin, and glucocorticoid.
- Involution: After weaning, when the baby is no longer in need of nourishment through suckling, lactation ceases, and the mammary gland involutes. During involution gene expression of the milk-manufacturing protein is suspended, mammary alveolar structures collapse, and secretory epithelial cells are removed through apoptosis and phagocytosis.
During each pregnancy, the above developmental sequence repeats itself as described.
Lactogenesis: The Transition from Pregnancy to Lactation
Lactogenesis is defined as the onset of milk secretion. Based on studies done by Hartmann (1973) and Linzell and colleagues (Fleet et al, 1975), lactogenesis has been divided into two stages. The first stage of lactogenesis is when the gland becomes differentiated enough to secrete small quantities of specific milk components such as casein and lactose. Lactogenesis Stage Two occurs after parturition (childbirth) and has to do with the onset of copious milk secretion. A completely differentiated mammary epithelium is necessary for Stage Two to occur. In humans, this highest stage of differentiation is reached around mid-pregnancy.
Although mammary epithelial cells are primarily responsible for converting precursors from the blood and interstitial fluid (fluid in the spaces between the tissue cells) into milk constituents and transporting them to the alveoli where milk is stored, other cells are also involved in milk production. As has already been mentioned, myoepithelial cells contract to eject milk from the breast. Additional types of cells are found within the stroma in which the mammary ducts and alveoli are embedded. Mammary stroma contains fibroblasts, adipocytes, plasma cells, and blood vessels. Fibroblasts are cells that give rise to connective tissue, adipocytes are cells specialized for the storage of fat, and plasma cells are the antibody-secreting cells of the immune system. Blood vessels comprise the arteries, veins, and capillaries through which blood circulates. Specifically though, stromal fibroblasts and adipocytes have been found to be the source of growth factors such as hepatic growth factor and IGF-1, and are also responsible for the production of the enzyme lipoprotein lipase which is important in milk lipid synthesis. Plasma cells are more specifically responsible for producing immunoglobulins (specific antibodies) that make their way into the milk during lactation. The mammary epithelium is therefore the master integrator that coordinates the activities of a variety of cells in order to produce the nutrient-rich milk.
Before actual lactogenesis, in the early post-partum period, the mammary gland secretes colostrum. This fluid is composed of high concentrations of immunoglobulins and the protective protein lactoferrin, which retards bacterial and fungal growth. In species such as ruminants (cattle, sheep, goats, deer, giraffes etc.) that lack transplancental transport of immunoglobulins, colostrum provides immune protection to the young while their immune system begins to mature. In humans however, where transplancental transport of immunoglobulins does occur, colostrum in the early post-partum period is important in protecting mucosal surfaces from infection, especially under conditions where optimal sanitation cannot be maintained.
The composition of human milk during the first week post-partum undergoes a progression of changes. These events begin with the closure of tight junctions between epithelial cells. The first chemical changes to occur in the production of mature milk is the decrease in sodium (Na) and chloride (Cl) concentrations and an increase in lactose concentration. These modifications are largely complete by 72 hours postpartum (Neville et al, 1991). With the closure of tight junctions, paracellular pathways are blocked, and lactose, made by epithelial cells, can no longer pass into the plasma, while sodium and chloride can no longer pass from the interstitial fluid into the alveolar sacs. The next change is a transient increase in the rates of secretory Immunoglobulin A (sIgA) and lactoferrin secretion. The concentration of these two important protective proeteins comprise as much as ten percent by weight of the milk. Then, starting about 36 hours postpartum, there is a ten-fold increase in milk volume from about 50 ml/day to 500 ml/day. This volume increase is brought about by a massive increase in the rates of synthesis and secretion of most of the components of mature milk including lactose, casein, alpha-lactalbumin, lipid, calcium, potassium, etc. Finally, the concentrations of sIgA and lactoferrin fall rapidly after about 48 hours due to a decrease in their absolute rate of secretion, and dilution as milk volume secretion increases.
The profound and rapid series of changes in the activity of differentiated mammary cells that is lactogenesis is complete by about day five postpartum. It is becoming increasingly clear to scientists that breast milk is the most appropriate source of nutrition up to the age of six months. Most components of human milk including lactoferrin, growth factors, long chain polyunsaturated fatty acids, bile salt stimulated lipase, and anti-infectious oligossacchardies and glycoconjugates are not duplicated in the cow's milk often used as an alternative.
Oxytocin and Milk Ejection
Milk is ejected from the breast by the contraction of myoepithelial cells which form a basket-like network around the alveoli where the milk is stored. In order for myoepithelial cells to contract and expell milk from the alveoli into the ducts and the sub-areolar sinuses, the cells must be activated by the hormone oxytocin. Oxytocin is carried through the blood stream to the mammary gland where it interacts with specific receptors on myoepithelial cells, signaling their shortening and widening of the ducts to allow free flow of milk to the nipple. The release of oxytocin into the blood stream however, is caused by the baby's suckling. In humans, milk ejection can be noted subjectively by the mother as a "tingling sensation" in the breast. The myoepithelial contractions causing this sensation last about one minute and occur with a frequency of four to ten contractions per ten minutes.
When the baby suckles the mother's nipple, nerve terminals in the areolus (the pigmented area surrounding the nipple) are stimulated and send information about suckling to the central nervous system: the spinal cord and the brain. Once the sensory information passes through the spinal cord, it travels through a part of the brain called the hypothalamus and then down to the pituitary gland, which releases oxytocin into the blood. The pituitary gland is nestled in a depression at the bottom of the skull just over the back of the roof of the mouth. It is attached by a stalk to the hypothalamus, which is in volved in many homeostatic regulatory systems. The pituitay gland has two distinct parts: the posterior pituitary and the anterior pituitary. The posterior pituitary releases two peptide hormones, one being oxtocin, and other antidiuretic hormone (ADH). But these two hormones are actually synthesized in neurons in the hypothalamus, and are therefore called "neurohormones". When oxytocin is produced in the hypothalamus, it is packaged in vesicles, and then transported down long extensions of the neurons, called axons that run from the hypothalamus, through the pituitary stalk, and into the posterior pituitary. There, the vesicles are stored in axon terminals until a nerve impulse, such as the baby's suckling, stimulates their release of oxytocin into the blood stream. Sometimes just the sights and the sounds of the baby can be enough for the mother to secrete oxytocin and release milk from her breasts.
In addition to its action on the mammary glands, oxytocin causes uterine contractions. When a woman is about to give birth, the contractions of the uterus that deliver the baby are caused by oxytocin released by the posterior pituitary. Furthermore, women who breastfeed their infants soon after delivery often experience uterine cramping. Finally, there is mounting evidence that oxytocin is involved in a positive feedback loop in wich it facilitates the release of prolactin. Prolactin stimulates the production and secretion of milk.
Emotional input has been found to have an effect on oxytocin release. In 1948 Newtown and Newtown proved that psychological stress and pain decreased milk output (Newton & Newton, 1948). In relaxed, undisturbed women however, oxytocin release begins with the onset of suckling or even before suckling when the infant cries or becomes restless (McNeilly et al., 1983).
Breast cancer
As described above, the cells of mammary glands can easily be induced to grow and multiply by hormones. If this growth runs out of control, cancer results. Almost all instances of breast cancer originate in the lobules or ducts of the mammary glands.
Other mammals
The development of the mammary glands in mammals other than humans follows the same sequence of events as listed above, however the duration of each stage varies from one speices to another. The location and external form of the mammary glands differ in varying species. Nipples and glands can occur anywhere along the two milk lines: two roughly-parallel lines along the front of the body. Milk lines are easily seen on cats and dogs where there are from 3 to 5 pairs of nipples following the two lines. Generally, most mammals develop mammary glands in pairs along these lines, with a number approximating the number of young typically birthed at a time. Male mammals typically have rudimentary mammary glands and nipples, with a few exceptions: male rats and mice don't have nipples, and male horses lack nipples and mammary glands.
Although mammary glands may look different in varying species, the mechanisms of milk production are remarkably similar. Yet, although the biochemical processes involved are funcdamentally the same in all mammals, differences in their relative rates, and in the products synthesized, result in milks whose composition differs widely from species to species. The temporal pattern of milk ejections also vary to a high degree amongst mammals. One the one hand, the rabbit nurses once daily, ejecting 250 grams of milk in two to five minutes in reponse to a single spurt of oxytocin. On the other hand, the rat nurses her littler on average about half an hour everyday. Humans fall between these two extremes.
Because mammary glands are true protein factories, several companies have constructed transgenic animals, mainly goats and cows, to produce proteins for pharmaceutical use. Complex glycoproteins such as monoclonal antibodies or antithrombin cannot be produced by genetically engineered bacteria. Moreover, production in live mammals is much cheaper than the use of mammalian cell cultures.
The presence of more than two nipples is known as polythelia and the presence of more than two complex mammary glands as polymastia.)
Mammary tumor
Breast cancer arises in humans from ductal cells altered in the terminal portions of the mammary tree. The development of the disease starts with an intitial intraductal epithelial hyperplasia (abnormal increase in the number of cells) and progresses to obstruction or closure of the duct. The most extreme atypical hyperplasia in humans is referred to as "intraductal carcinoma in situ". Intraductal carcinoma in situ is followed by locally invasive coarconoma and subsequent metastasis (cancer growth elsewhere in the body) to the lungs, bones, and liver. There are many differences between breast cancer in humans and mammary tumors in animals including tumor type, malignancy, and treatment options.
Mammary tumors are a common finding in middle-aged (5-10 years) female dogs who are not spayed (to surgically remove the ovaries), but they are rare in male dogs and cats of either gender. The mammary glands in dogs are associated with their nipples and extend from the underside of the chest to the groin on both sides of the midline. A female puppy spayed before her first heat cycle will probably never develop a mammary tumor of any kind. The incidence of tumor development in this group is roughly zero. If the female puppy experiences one heat cycle before spaying, the incidence rises to seven percent (still quite low). If she experiences more than one heat cycle, the risk is driven up to one in four. Although the risk of unspayed females developing mammary tumors is very high, approximately 50 percent of tumors are benign, and 50 percent are malignant. From the group of malignant mammary tumors, 50 percent have been found to have receptors for either estrogen or progesterone. This indicates that the presence of these hormones promotes the growth of these tumors. Benign tumors also have also been found to have female hormone receptors. These findings demonstrate that spaying is important even if a tumor has already developed. Malignant mammary tumors are divided into four classes: fibroadenoma, mixed mammary tumor", adenocarcinoma, and inflammatory carcinoma:
- Fibroadenoma: a benign tumor that does not necessitate treatment
- Mixed Mammary Tumor: tumor composed of a mix if epithelial cells that line glandular tissue and mesenchymal cells that make up the non-gladular regions ("mixed" does not mean that the tumor is a mix of benign and malignant cells; the tumor may be either benign or malignant, and a biopsy will differentiate).
- Adenocarcinoma: tumor that originating in gladular tissue and behaves malignantly . Adenocarcinomas can be “tubular” or “papillary” (resembling the nipple) depending on that gland cells that it arises from.
- Inflamatory Carcinoma: highly malignant tumor that generates inflammation locally with ulceration, pus, and discomfort. This fatal tumor type accounts for less than five percent of mammary tumors.
In contrast to the 50 percent of malignant mammary tumors in female dogs, over 85% of mammary tumors in cats are malignant with aggressive biologic behavior (they are locally invasive and metastasize to sites such as the lymph nodes and lungs).
External links
- Comparative Mammary Gland Anatomy by W. L. Hurley
- On the anatomy of the breast by Sir Astley Paston Cooper (1840). Numerous drawings, in the public domain.
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.
http://www.breastfeeding.com/reading_room/breasts_shaped_babies.html