|
|
| (84 intermediate revisions by 2 users not shown) |
| Line 1: |
Line 1: |
| − | '''Working on —[[User:Jennifer Tanabe|Jennifer Tanabe]] ([[User talk:Jennifer Tanabe|talk]]) 20:38, 21 March 2020 (UTC)'''
| + | {{Images OK}}{{Submitted}}{{Approved}}{{Copyedited}} |
| | | | |
| − | <references group="The U.S. Nursing Workforce in 2018 and Beyond Journal of Nursing Regulation , Volume 8, Issue 4, S3 - S6" />
| |
| | {{Redirect|Nurse|}} | | {{Redirect|Nurse|}} |
| | | | |
| | {{Infobox Occupation | | {{Infobox Occupation |
| | | name= Nurse | | | name= Nurse |
| − | | image= British woman tending to a baby.jpg | + | | image= [[File:British woman tending to a baby.jpg|225px]] |
| | | caption= A British nurse caring for a baby | | | caption= A British nurse caring for a baby |
| | | official_names= Nurse | | | official_names= Nurse |
| Line 16: |
Line 15: |
| | Qualifications in terms of statutory regulations according to national, state, or provincial legislation in each country | | Qualifications in terms of statutory regulations according to national, state, or provincial legislation in each country |
| | | employment_field= | | | employment_field= |
| − |
| + | </br> |
| | *[[Hospital]] | | *[[Hospital]] |
| | *[[Clinic]] | | *[[Clinic]] |
| Line 22: |
Line 21: |
| | *[[Research]] | | *[[Research]] |
| | *[[Education]] | | *[[Education]] |
| − | | + | | related_occupation=</br> |
| − | | related_occupation= | |
| − | | |
| | *[[Medicine]] | | *[[Medicine]] |
| | }} | | }} |
| | | | |
| − | '''Nursing''' is a profession within the [[health care]] sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and [[quality of life (healthcare)|quality of life]]. Nurses may be differentiated from other [[health care providers]] by their [[nursing theory|approach to patient care]], [[nurse education|training]], and [[scope of practice]]. Nurses practice in many [[List of nursing specialties|specialties]] with differing levels of [[medical prescription|prescription authority]]. Many nurses provide care within the ordering scope of [[physician]]s, and this traditional role has shaped the public image of nurses as care providers. However, nurse practitioners are permitted by most jurisdictions to practice independently in a variety of settings. Since the [[Post-war|postwar]] period, nurse education has undergone a process of diversification towards [[Nursing credentials and certifications|advanced and specialized credentials]], and many of the traditional regulations and provider roles are changing.<ref>Coulehan J. L., Block M. R. (2005): The Medical Interview: Mastering skills for clinical practice, 5th Ed. F. A. Davis. {{ISBN|0-8036-1246-X}}. {{OCLC|232304023}}.</ref><ref>Dunphy L. M., Winland-Brown J. E. (2011): Primary care: The art and science of advanced practice nursing. F.A. Davis. {{ISBN|9780803626478}}.</ref> | + | '''Nursing''' is a profession within the [[health care]] sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and [[quality of life (healthcare)|quality of life]]. Nurses may be differentiated from other [[health care providers]] by their [[nursing theory|approach to patient care]], [[nurse education|training]], and [[scope of practice]]. Many nurses provide care within the ordering scope of [[physician]]s, and this traditional role has shaped the public image of nurses as care providers. |
| | + | {{toc}} |
| | + | Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient's family, and other team members that focuses on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of a multidisciplinary health care team such as therapists, medical practitioners, and dietitians. In some countries, including the United States and the United Kingdom, advanced practice nurses, such as clinical nurse specialists and nurse practitioners, diagnose health problems and prescribe medications and other therapies. Nurses fulfill a vital function in human society, providing health care both interdependently, such as with physicians, and independently as nursing professionals. |
| | | | |
| − | Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient's family, and other team members that focuses on treating illness to improve quality of life. In the United States and the United Kingdom, advanced practice nurses, such as clinical nurse specialists and nurse practitioners, diagnose health problems and prescribe medications and other therapies, depending on individual state regulations. Nurses may help coordinate the patient care performed by other members of a multidisciplinary health care team such as therapists, medical practitioners, and dietitians. Nurses provide care both interdependently, for example, with physicians, and independently as nursing professionals.
| + | ==Definition== |
| | + | Although nursing practice varies both through its various specialties and countries, these nursing organizations offer the following definitions: |
| | + | <blockquote> |
| | + | Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or well, and in all settings. Nursing includes the promotion of health, prevention of illness, and the care of ill, disabled and dying people. Advocacy, promotion of a safe environment, research, participation in shaping health policy and in patient and health systems management, and education are also key nursing roles. ([[International Council of Nurses]])<ref>[https://www.icn.ch/nursing-policy/nursing-definitions Definition of Nursing] ''ICN'', 2002. Retrieved April 1, 2020.</ref></blockquote> |
| | | | |
| | + | <blockquote>The use of clinical judgment in the provision of care to enable people to improve, maintain, or recover health, to cope with health problems, and to achieve the best possible quality of life, whatever their disease or disability, until death. ([[Royal College of Nursing]])<ref>Helen Scott, [https://www.magonlinelibrary.com/doi/abs/10.12968/bjon.2002.11.21.10922 RCN's definition of nursing: what makes nursing unique?] ''British Journal of Nursing'' 11(21) (September 27, 2013). Retrieved April 1, 2020. </ref></blockquote> |
| | | | |
| − | ==History==
| + | <blockquote>Nursing is the protection, promotion, and optimization of health and abilities; prevention of illness and injury; alleviation of suffering through the diagnosis and treatment of human responses; and advocacy in health care for individuals, families, communities, and populations. ([[American Nurses Association]])<ref>[https://www.nursingworld.org/practice-policy/scope-of-practice/ Scope of practice defined in nursing] ''ANA''. Retrieved April 1, 2020.</ref></blockquote> |
| − | {{Main article|History of nursing|Timeline of nursing history}}
| |
| | | | |
| − | ===Traditional===
| + | <blockquote>The unique function of the nurse is to assist the individual, sick or well, in the performance of those activities contributing to health or its recovery (or to peaceful death) that he would perform unaided if he had the necessary strength, will or knowledge. ([[Virginia Avenel Henderson]])<ref> Angelo Gonzalo, [https://nurseslabs.com/virginia-hendersons-need-theory/ Virginia Henderson: Nursing Need Theory] ''Nurseslabs''. Retrieved April 1, 2020.</ref></blockquote> |
| − | Nursing historians face the challenge of determining whether care provided to the sick or injured in antiquity was nursing care.<ref name="OLYNN2007">{{cite book|last1=O'Lynn|first1=CE|editor1-last=O'Lynn|editor1-first=CE|editor2-last=Tranbarger|editor2-first=RE|title=Men in Nursing: History, Challenges, and Opportunities|date=2007|publisher=Springer Pub.|location=New York|isbn=9780826103499|pages=6–8|chapter=History of men in nursing: a review}}</ref> In the fifth century B.C.E., for example, the [[Hippocratic Collection]] in places describes skilled care and observation of patients by male "attendants," who may have been early nurses.<ref name="LEVINE1965">{{cite journal|last1=Levine|first1=EB|last2=Levine|first2=ME|title=Hippocrates, father of nursing, too?|journal=The American Journal of Nursing|date=1965|volume=65|issue=12|pages=86–8|pmid=5319739|doi=10.1097/00000446-196512000-00022}}</ref> Around 600 BC in India, it is recorded in [[Sushruta Samhita]], Book 3, Chapter V about the role of the nurse as "the different parts or members of the body as mentioned before including the skin, cannot be correctly described by one who is not well versed in anatomy. Hence, any one desirous of acquiring a thorough knowledge of anatomy should prepare a dead body and carefully, observe, by dissecting it, and examine its different parts."
| |
| | | | |
| − | Before the foundation of modern nursing, members of religious orders such as [[nuns]] and [[monks]] often provided nursing-like care.<ref name="BLOY">{{cite web|last=Bloy|first=M|url=http://www.victorianweb.org/history/crimea/florrie.html|title=Florence Nightingale (1820–1910)|website=The Victorian Web|accessdate=2014-11-24}}</ref> Examples exist in [[Christianity|Christian]],<ref name="FERNGREN2009">{{cite book|last1=Ferngren|first1=GB|title=Medicine & health care in early Christianity|date=2009|publisher=Johns Hopkins University Press|location=Baltimore|isbn=9780801895227|page=121}}</ref> [[Islamic]]<ref name="SACHEDINA2009">{{cite book|last1=Sachedina|first1=Abdulaziz|title=Islamic biomedical ethics: principles and application|date=2009|publisher=Oxford University Press|location=Oxford|isbn=9780195378504|pages=93–94}}</ref> and [[Buddhist]]<ref name="DEBARY2011">{{cite book|editor1-last=de Bary|editor1-first=WT|title=The Buddhist tradition in India, China & Japan|date=2011|publisher=Vintage eBooks|location=New York|isbn=9780307778796|pages=35–36|edition=Unabridged.}}</ref> traditions amongst others. [[Phoebe (biblical figure)|Phoebe]], mentioned in [[Epistle to the Romans|Romans]] 16 has been described in many sources as "the first visiting nurse".<ref name="EGENES2009">{{cite book|last1=Egenes|first1=KJ|editor1-last=Halstead|editor1-first=J|editor2-last=Roux|editor2-first=G|title=Issues and Trends in Nursing: Essential Knowledge for Today and Tomorrow|date=2009|publisher=Jones and Bartlett|location=Sudbury, MA|isbn=9780763752255|page=[https://archive.org/details/issuestrendsinnu0000unse/page/2 2]|chapter=History of nursing|chapter-url=https://archive.org/details/issuestrendsinnu0000unse/page/2}}</ref><ref name="STRIEPE1992">{{cite journal|last1=Striepe|first1=JM|title=Reclaiming the church's healing role|journal=Journal of Christian Nursing|date=1992|volume=10|issue=1|pages=4–7|doi=10.1097/00005217-199310010-00002|pmid=8418284}}</ref> These traditions were influential in the development of the [[ethos]] of modern nursing. The religious roots of modern nursing remain in evidence today in many countries. One example in the [[United Kingdom]] is the use of the historical title "sister" to refer to a senior nurse in the past.<ref name="WAND2004">{{cite journal|last1=Wand|first1=T|title=The 'Sister' title: past the use by date?|journal=Collegian|date=January 2004|volume=11|issue=1|pages=35–39|doi=10.1016/S1322-7696(08)60442-4}}</ref>
| + | ==History== |
| | + | Nursing historians face the challenge of determining whether care provided to the sick or injured in antiquity was nursing care.<ref>Chad E. O'Lynn and Russell E. Tranbarger (eds.), ''Men in Nursing: History, Challenges, and Opportunities'' (Springer Publishing Company, 2006, ISBN 978-0826102218).</ref> In the fifth century B.C.E., for example, [[Hippocrates]] describes the giving of skilled care and observation of patients by "attendants," who could be considered as early nurses.<ref>Edwin B. Levine and Myra E. Levine, [https://journals.lww.com/ajnonline/Abstract/1965/12000/HIPPOCRATES,_Father_of_Nursing,_Too_.22.aspx Hippocrates, father of nursing, too?] ''The American Journal of Nursing'' 65(12) (December 1965):86-88. Retrieved March 30, 2020.</ref> |
| | | | |
| − | During the [[Reformation]] of the 16th century, [[Protestant]] reformers shut down the monasteries and convents, allowing a few hundred municipal hospices to remain in operation in northern Europe. Those nuns who had been serving as nurses were given pensions or told to get married and stay home.<ref>{{cite book|last1=Leonard|first1=AE|chapter=Female religious orders|page=244|editor1-last=Hsia|editor1-first=RP|title=A Companion to the Reformation World|date=2008|publisher=Blackwell Publishers|location=Oxford|isbn=978-1405149624|edition=1st paperback}}</ref> Nursing care went to the inexperienced as traditional caretakers, rooted in the Roman Catholic Church, were removed from their positions. The nursing profession suffered a major setback for approximately 200 years.<ref>{{cite book|last1=Lundy|first1=KS|editor1-last=Masters|editor1-first=K|title=Role Development in Professional Nursing Practice|date=2014|publisher=Jones & Bartlett Learning|location=Burlington, MA|isbn=9781449681982|pages=11–12|edition=3rd|chapter=A history of health care and nursing}}</ref>
| + | Before the foundation of modern nursing, members of religious orders such as [[nuns]] and [[monks]] often provided nursing-like care. These are found, for example, in [[Christianity|Christian]],<ref>Gary B. Ferngren, ''Medicine and Health Care in Early Christianity'' (Johns Hopkins University Press, 2016, ISBN 978-1421420066).</ref> [[Islamic]]<ref>Abdulaziz Sachedina, ''Islamic Biomedical Ethics: Principles and Application '' (Oxford University Press, 2009, ISBN 978-0195378504).</ref> and [[Buddhist]]<ref>William Theodore de Bary, ''The Buddhist Tradition: In India, China and Japan'' (Vintage, 1972, ISBN 978-0394716961). </ref> traditions. These traditions were influential in the development of the [[ethos]] of modern nursing. |
| | | | |
| − | ===19th century===
| + | During the [[Reformation]] of the sixteenth century, [[Protestant]] reformers shut down the [[monasteries]] and [[convent]]s, allowing a few hundred municipal [[hospice]]s to remain in operation in northern Europe. Nursing care went to the inexperienced as traditional caretakers, rooted in the [[Roman Catholic]] Church, were removed from their positions. As a result, the nursing profession suffered a major setback for approximately 200 years.<ref>Kathleen Masters, ''Role Development in Professional Nursing Practice'' (Jones & Bartlett Learning, 2018, ISBN 978-1284152913). </ref> |
| − | [[File:Сестры Крестовоздвиженской общины, Севастополь, 1855.jpg|upright|thumb|Russian Sisters of Mercy in the Crimea, 1854-1855]] | |
| − | During the [[Crimean War]] the [[Princess Charlotte of Württemberg|Grand Duchess Elena Pavlovna]] issued the call for women to join the Order of Exaltation of the Cross (Krestodvizhenskaya obshchina) for the year of service in the military hospitals. The first section of twenty-eight "sisters", headed by Aleksandra Petrovna Stakhovich, the Directress of the Order, went off to the Crimea early in November 1854.<ref>[https://www.jstor.org/stable/2492652?seq=1 Russian Sisters of Mercy in the Crimea, 1854-1855]</ref>
| |
| | | | |
| − | [[File:Florence Nightingale (H Hering NPG x82368).jpg|225px|thumb|[[Florence Nightingale]] was an influential figure in the development of modern nursing. No uniform had been created when Nightingale was employed during the [[Crimean War]]. Often considered the first nurse theorist, Nightingale linked health with five environmental factors:(1) pure or fresh air, (2) pure water, (3) efficient drainage, (4) cleanliness, and (5) light, especially direct sun light. Deficiencies in these five factors resulted in lack of health or illness.<ref>Professional Nursing Practice: Concepts and perspective, Koernig & Hayes, sixth edition, 2011, p.100, {{ISBN|978-0-13-508090-0}}</ref> Both the role of nursing and education were first defined by Nightingale.]] | + | ===Nineteenth century=== |
| | + | [[File:Сестры Крестовоздвиженской общины, Севастополь, 1855.jpg|250px|thumb|Russian Sisters of Mercy in the Crimea, 1854-1855]] |
| | + | During the [[Crimean War]] the [[Grand Duchess Elena Pavlovna]] issued the call for women to join the Order of Exaltation of the Cross (Krestodvizhenskaya obshchina) for the year of service in the military hospitals. The first section of twenty-eight "sisters," headed by Aleksandra Petrovna Stakhovich, the Directress of the Order, went off to the Crimea early in November 1854.<ref>John Shelton Curtiss, Russian Sisters of Mercy in the Crimea, 1854-1855 ''Slavic Review'' 25(1) (March 1966): 84-100. </ref> |
| | | | |
| − | [[Florence Nightingale]] laid the foundations of professional nursing after the [[Crimean War]].<ref name="WINKEL2009">{{cite journal|last1=Winkel|first1=W|title=Florence Nightingale|journal=Epidemiology|date=2009|volume=20|issue=2|pages=311|doi=10.1097/EDE.0b013e3181935ad6|pmid=19234417}}</ref> Her ''[[Notes on Nursing]]'' (1859) became popular. The Nightingale model of professional education, having set up the [[Florence Nightingale Faculty of Nursing and Midwifery|first school of nursing]] that is connected to a continuously operating hospital and medical school, spread widely in Europe and North America after 1870.<ref name="Quinn">{{cite book|last=Quinn|first=Shawna M.|title=Agnes Warner and the Nursing Sisters of the Great War|url=http://www.gooselane.com/media/741.pdf|publisher=Goose Lane editions and the New Brunswick Military Heritage Project |date=2010|isbn=978-0-86492-633-3|accessdate=2014-11-29|url-status=dead|archiveurl=https://web.archive.org/web/20150924023052/http://www.gooselane.com/media/741.pdf|archivedate=2015-09-24|df=dmy-all}}</ref> Nightingale was also a pioneer of the graphical presentation of [[statistics|statistical]] [[data]].<ref>{{cite news|last1=Bostridge|first1=Mark|title=Florence Nightingale: the Lady with the Lamp|url=https://www.bbc.co.uk/history/british/victorians/nightingale_01.shtml|publisher=BBC|date=26 October 2017}}</ref> | + | [[File:Florence Nightingale (H Hering NPG x82368).jpg|200px|thumb|[[Florence Nightingale]] was an influential figure in the development of modern nursing. No uniform had been created when Nightingale was employed during the [[Crimean War]]. Both the role of nursing and education were first defined by Nightingale.]] |
| | | | |
| − | Other important nurses in the development of the profession include:
| + | [[Florence Nightingale]] laid the foundations of professional nursing after the [[Crimean War]].<ref>Warren Winkelstein, Jr., [https://journals.lww.com/epidem/fulltext/2009/03000/Florence_Nightingale__Founder_of_Modern_Nursing.25.aspx Florence Nightingale: Founder of Modern Nursing and Hospital Epidemiology] ''Epidemiology'' 20(2) (March 2009): 311. Retrieved April 2, 2020.</ref> From 1870, having set up the first school of nursing connected to a continuously operating hospital and medical school, the Nightingale model of professional education spread widely in Europe and North America.<ref>Shawna M. Quinn, ''Agnes Warner and the Nursing Sisters of the Great War'' (Goose Lane Editions, 2010, ISBN 978-0864926333).</ref> Often considered the first nurse theorist, Nightingale linked health with five environmental factors:(1) pure or fresh air, (2) pure water, (3) efficient drainage, (4) cleanliness, and (5) light, especially direct sun light. Deficiencies in these five factors resulted in lack of health or illness.<ref>Kathy Blais and Janice S. Hayes, ''Professional Nursing Practice: Concepts and Perspectives'' (Pearson, 2015, ISBN 978-0133801316).</ref> Nightingale was also a pioneer of the graphical presentation of [[statistics|statistical]] [[data]].<ref>Mark Bostridge, [https://www.bbc.co.uk/history/british/victorians/nightingale_01.shtml Florence Nightingale: the Lady with the Lamp|] ''BBC'', February 17, 2011. Retrieved April 2, 2020.</ref> |
| − | *[[Agnes Hunt]] from [[Shropshire]] was the first orthopedic nurse and was pivotal in the emergence of the orthopedic hospital The Robert Jones & Agnes Hunt Hospital in Oswestry, Shropshire.
| |
| − | *[[Agnes Jones]], who established a nurse training regime at the [[Brownlow Hill infirmary]], Liverpool, in 1865.
| |
| − | *[[Linda Richards]], who established quality [[nursing schools]] in the United States and Japan, and was officially the first professionally trained nurse in the US, graduating in 1873 from the ''[[New England Hospital for Women and Children]]'' in Boston.
| |
| − | *[[Clara Barton|Clarissa Harlowe "Clara" Barton]], a pioneer American teacher, patent clerk, nurse, and humanitarian, and the founder of the American Red Cross.
| |
| − | * Saint [[Marianne Cope]], a Sister of St. Francis who opened and operated some of the first general hospitals in the United States, instituting cleanliness standards which influenced the development of America's modern hospital system.<ref>[http://edition.cnn.com/2012/10/20/health/saint-marianne-cope/index.html?hpt=hp_t3 Mother Marianne becomes an American saint – CNN.com]. Edition.cnn.com. Retrieved on 2013-07-28.</ref>
| |
| | | | |
| − | Catholic orders such as [[Little Sisters of the Poor]], [[Sisters of Mercy]], [[Sisters of St. Mary]], [[Franciscan Alliance, Inc.|St. Francis Health Services, Inc.]] and [[Sisters of Charity]] built hospitals and provided nursing services during this period.{{citation needed|date=November 2014}} In turn, the modern deaconess movement began in Germany in 1836.<ref name="NAUMANN2008">{{cite book|last1=Naumann|first1=CD|title=In the footsteps of Phoebe: a Complete History of the Deaconess Movement in the Lutheran Church—Missouri Synod|date=2008|publisher=Concordia Pub. House|location=St. Louis, MO|isbn=9780758608314|page=4}}</ref> Within a half century, there were over 5,000 deaconesses in Europe.<ref name="BLACKMORE2007">{{cite book|editor1-last=Blackmore|editor1-first=H|title=The Beginning of Women's Ministry: the Revival of the Deaconess in the Nineteenth-century Church of England|date=2007|url=https://books.google.com/books?id=8LQxO03zXygC&pg=PA131|publisher=Boydell Press|location=Woodbridge|isbn=978-1-84383-308-6}}</ref>
| + | The following were also important in the development of the nursing profession in the nineteenth century: |
| | | | |
| − | Formal use of nurses in the modern military began in the latter half of the nineteenth century. Nurses saw active duty in the [[First Boer War]], the Egyptian Campaign (1882), <ref>{{cite web|title=Our History|url=http://www.army.mod.uk/army-medical-services/qaranc/9910.aspx|publisher=British Army Website|accessdate=2011-10-31|url-status=dead|archiveurl=https://web.archive.org/web/20111028190846/http://www.army.mod.uk/army-medical-services/qaranc/9910.aspx|archivedate=2011-10-28|df=dmy-all}}</ref> and the [[Mahdist War|Sudan Campaign]] (1883).<ref>{{Cite web|title = History of the School of Nursing |publisher= University of Maryland School of Nursing|url = https://www.nursing.umaryland.edu/about/community/museum/virtual-tour/foundation/|access-date = 2016-01-19}}</ref>
| + | *[[Agnes Jones]], of Fahan, County Donegal, Ireland became the first trained Nursing Superintendent of Liverpool Workhouse Infirmary at Brownlow Hill in 1865, and established a nurse training regime there.<ref> Steven Horton, [http://liverpoolhiddenhistory.co.uk/agnes-jones/ Agnes Jones] ''Liverpool Hidden History'', February 18, 2018. Retrieved April 2, 2020.</ref> |
| | + | *[[Linda Richards]], who was the first professionally trained nurse in the US graduated in 1873 from the ''[[New England Hospital for Women and Children]]'' in Boston, established quality [[nursing schools]] in the United States and Japan. She served as the first president of the American Society of Superintendents of Training Schools in 1894, which was the first professional organization for nurses.<ref> [https://www.aahn.org/richards Linda A.J. Richards 1841 - 1930] ''American Association for the History of Nursing''. Retrieved April 2, 2020.</ref> |
| | + | *[[Clara Barton|Clarissa Harlowe "Clara" Barton]], a pioneer American teacher, patent clerk, nurse, and humanitarian, and the founder of the American [[Red Cross]].<ref>[https://www.redcross.org/about-us/who-we-are/history/clara-barton.html Founder Clara Barton] ''The American National Red Cross''. Retrieved April 2, 2020.</ref> |
| | + | * Saint [[Marianne Cope]], a Sister of St. Francis who opened and operated some of the first general hospitals in the United States, instituting cleanliness standards which influenced the development of America's modern hospital system.<ref>Jen Christensen, [https://edition.cnn.com/2012/10/20/health/saint-marianne-cope/index.html?hpt=hp_t3 Mother Marianne becomes an American saint] ''CNN'', October 22, 2012. Retrieved April 2, 2020.</ref> |
| | + | *[[Agnes Hunt]] from [[Shropshire]] was the first orthopedic nurse and was pivotal in the emergence of the The Robert Jones and Agnes Hunt Orthopaedic Hospital in Oswestry, Shropshire, UK.<ref> Hospital History ''The Robert Jones and Agnes Hunt Orthopaedic Hospital''.</ref> |
| | | | |
| − | ===20th century===
| + | Catholic orders such as [[Little Sisters of the Poor]], [[Sisters of Mercy]], [[Sisters of St. Mary]], [[Franciscan Alliance, Inc.|St. Francis Health Services, Inc.]], and [[Sisters of Charity]] built hospitals and provided nursing services during this period. |
| − | {{Further information|Women in nursing}}
| |
| − | [[File:RedCrossNursen.jpg|thumb|left|A recruiting poster for Australian nurses from [[World War I]]]] | |
| | | | |
| − | Hospital-based training came to the fore in the early 1900s, with an emphasis on practical experience. The Nightingale-style school began to disappear. Hospitals and physicians saw women in nursing as a source of free or inexpensive labor. Exploitation of nurses was not uncommon by employers, physicians, and educational providers.<ref name=CHIN2008>{{cite book|last1=Chin|first1=PL|last2=Kramer|first2=MK|title=Integrated Theory and Knowledge Development in Nursing|date=2008|publisher=Mosby Elsevier|location=St. Louis|isbn=9780323052702|pages=[https://archive.org/details/integratedtheory0000chin/page/33 33–34]|edition=7th|url=https://archive.org/details/integratedtheory0000chin/page/33}}</ref>
| + | ===Twentieth century=== |
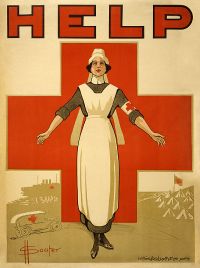
| | + | [[File:RedCrossNursen.jpg|thumb|right|200px|A recruiting poster for Australian nurses from [[World War I]]]] |
| | | | |
| − | Many nurses saw active duty in [[World War I]], but the profession was transformed during the [[World War II|Second World War]]. British nurses of the Army Nursing Service were part of every overseas campaign.<ref>{{cite web|title=QA World War Two Nursing|url=http://www.qaranc.co.uk/qa_world_war_two_nursing.php|publisher=qaranc.co.uk|accessdate=2011-10-31}}</ref> More nurses volunteered for service in the US [[United States Army|Army]] and [[United States Navy|Navy]] than any other occupation.<ref>D'Ann Campbell, ''Women at War with America: Private Lives in a Patriotic Era'' (1984) ch 2</ref><ref>Philip A. Kalisch and Beatrice J. Kalisch, ''American Nursing: A History'' (4th ed. 2003)</ref> The Nazis had their own Brown Nurses, 40,000 strong.<ref>Bronny Rebekah McFarland-Icky, ''Nurses in Nazi Germany'' (Princeton University Press, 1999)</ref> Two dozen German Red Cross nurses were awarded the [[Iron Cross]] for heroism under fire.<ref>Gordon Williamson, ''World War II German Women's Auxiliary Services'' (2003) pp 34–36</ref>
| + | Hospital-based training came to the fore in the early 1900s, with an emphasis on practical experience. The Nightingale-style school began to disappear. |
| | | | |
| − | The modern era saw the development of undergraduate and post-graduate [[Nurse education|nursing degrees]]. Advancement of nursing research and a desire for association and organization led to the formation of a wide variety of [[professional organizations]] and [[nursing journal|academic journals]]. Growing recognition of nursing as a distinct academic discipline was accompanied by an awareness of the need to define the [[Nursing theory|theoretical basis]] for practice.<ref name=ALLIGOOD2013>{{cite book|last1=Alligood|first1=MR|editor1-last=Alligood|editor1-first=MR|editor2-last=Tomey|editor2-first=AM|title=Nursing Theorists and their Work|date=2013|publisher=Mosby/Elsevier|location=Maryland Heights, MO|isbn=9780323056410|pages=5–6|edition=7th|chapter=Introduction to nursing theory}}</ref>
| + | Many nurses saw active duty in [[World War I]], but the profession was transformed during the [[World War II|Second World War]]. British nurses of the Army Nursing Service were part of every overseas campaign.<ref>[https://qaranc.co.uk/qa_world_war_two_nursing.php QA World War Two Nursing] ''Qaranc''. Retrieved April 2, 2020. </ref> More nurses volunteered for service in the US [[United States Army|Army]] and [[United States Navy|Navy]] than any other occupation.<ref>Philip A. Kalisch and Beatrice J. Kalisch, ''American Nursing: A History'' (LWW, 2003, ISBN 978-0781739696).</ref> The Nazis had their own Brown Nurses, 40,000 strong.<ref>Bronny Rebekah McFarland-Icky, ''Nurses in Nazi Germany'' (Princeton University Press, 1999, 978-0691006659).</ref> Two dozen German Red Cross nurses were awarded the [[Iron Cross]] for heroism under fire.<ref>Gordon Williamson, ''World War II German Women's Auxiliary Services'' (Osprey Publishing, 2003, ISBN 978-1841764078).</ref> |
| | | | |
| − | In the 19th and early 20th century, nursing was considered a women's profession, just as doctoring was a men's profession. With increasing expectations of workplace equality during the late 20th century, nursing became an officially [[Gender marking in job titles|gender-neutral]] profession, though in practice the percentage of male nurses remains well below that of female [[physician]]s in the early 21st century.<ref>{{Cite web|title = Total Number of Professionally Active Nurses, by Gender|url = http://kff.org/other/state-indicator/total-number-of-professionally-active-nurses-by-gender/#table|website = kff.org|access-date = 2016-01-19|language = en-US}}</ref><ref>{{Cite web|title = Distribution of Physicians by Gender|url = http://kff.org/other/state-indicator/physicians-by-gender/|website = kff.org|access-date = 2016-01-19|language = en-US}}</ref>
| + | Since the [[Post-war|postwar]] period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles have been changing.<ref>Lynne M. Dunphy, Jill E. Winland-Brown, Brian Oscar Porter, and Debera J. Thomas, ''Primary Care: Art and Science of Advanced Practice Nursing - An Interprofessional Approach'' (F.A. Davis Company, 2019, ISBN 978-0803667181).</ref> |
| | + | [[File:Male Nurses- Life at Runwell Hospital, Wickford, Essex, 1943 D14313.jpg|thumb|right|225px|A nurse at Runwell Hospital, Wickford, Essex, in 1943]] |
| | + | The modern era saw the development of undergraduate and post-graduate [[Nurse education|nursing degrees]]. Advancement of nursing research and a desire for association and organization led to the formation of a wide variety of [[professional organizations]] and academic journals in the field. Growing recognition of nursing as a distinct academic discipline was accompanied by an awareness of the need to define the [[Nursing theory|theoretical basis]] for practice.<ref>Martha Raile Alligood, ''Nursing Theorists and Their Work'' (Mosby, 2013, ISBN 978-0323091947).</ref> |
| | | | |
| − | ==Definition==
| + | In the nineteenth and early twentieth century, nursing was considered a women's profession, just as doctoring was a men's profession. With increasing expectations of workplace equality during the late twentieth century, nursing became an officially gender-neutral profession. In practice, however, the percentage of male nurses remained well below that of female [[physician]]s in the early twenty-first century. |
| − | | |
| − | Although nursing practice varies both through its various specialties and countries, these nursing organizations offer the following definitions:
| |
| − | | |
| − | {{Quote | Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or well, and in all settings. Nursing includes the promotion of health, prevention of illness, and the care of ill, disabled and dying people. Advocacy, promotion of a safe environment, research, participation in shaping health policy and in patient and health systems management, and education are also key nursing roles. | [[International Council of Nurses]]<ref name="ICN"/>}}
| |
| − | | |
| − | {{Quote|The use of clinical judgment in the provision of care to enable people to improve, maintain, or recover health, to cope with health problems, and to achieve the best possible quality of life, whatever their disease or disability, until death.|[[Royal College of Nursing]] (2003) <ref>{{cite web |url=https://www.rcn.org.uk/professional-development/publications/pub-004768 |title=Defining nursing 2014 |publisher=[[Royal College of Nursing]] (RCN) |date=22 December 2014 |accessdate=2016-10-08}}</ref>}}
| |
| − | | |
| − | {{Quote|Nursing is the protection, promotion, and optimization of health and abilities; prevention of illness and injury; alleviation of suffering through the diagnosis and treatment of human responses; and advocacy in health care for individuals, families, communities, and populations.|[[American Nurses Association]]<ref>[https://www.nursingworld.org/practice-policy/scope-of-practice/ ANA Considering Nursing] Retrieved Dec 2018</ref>|source=}}
| |
| − | | |
| − | {{Quote|The unique function of the nurse is to assist the individual, sick or well, in the performance of those activities contributing to health or its recovery (or to peaceful death) that he would perform unaided if he had the necessary strength, will or knowledge.|[[Virginia Avenel Henderson]]<ref>[http://www.contemporarynurse.com/archives/vol/5/issue/3/article/3027/virginia-henderson-a-contemporary-nurse-18971996 Contemporary Nurse Virginia Henderson] {{webarchive|url=https://web.archive.org/web/20090914053915/http://www.contemporarynurse.com/archives/vol/5/issue/3/article/3027/virginia-henderson-a-contemporary-nurse-18971996 |date=14 September 2009 }} Retrieved July 2009</ref>}}
| |
| | | | |
| | ==As a profession== | | ==As a profession== |
| − | [[File:Indonesian nurse examines patient.JPG|thumb|A nurse in Indonesia examining a patient]]
| + | Nurses care for individuals of all ages and cultural backgrounds who are healthy and ill in a [[Holistic health|holistic]] manner based on the individual's physical, emotional, psychological, intellectual, social, and spiritual needs. The profession combines physical science, social science, nursing theory, and technology in caring for those individuals. The authority for the practice of nursing is based upon a social contract that delineates professional rights and responsibilities as well as mechanisms for public accountability. In almost all countries, nursing practice is defined and governed by law, and entrance to the profession is regulated at the national or state level. |
| − | [[File:ASC Leiden - Coutinho Collection - 10 04 - Nurses in Ziguinchor hospital, Senegal - 1973.tif|thumb|A nurse treating a patient with burns, [[Ziguinchor]] [[PAIGC]] hospital, 1973]]
| |
| − | The authority for the practice of nursing is based upon a social contract that delineates professional rights and responsibilities as well as mechanisms for public accountability. In almost all countries, nursing practice is defined and governed by law, and entrance to the profession is regulated at the national or state level.
| |
| − | | |
| − | The aim of the nursing community worldwide is for its professionals to ensure quality care for all, while maintaining their credentials, code of [[Nursing ethics|ethics]], standards, and competencies, and continuing their education.<ref name="ICN">[http://www.icn.ch/abouticn.htm International Council of Nurses] Retrieved August 2007</ref> There are a number of educational paths to becoming a professional nurse, which vary greatly worldwide; all involve extensive study of [[nursing theory]] and practice as well as training in clinical skills.
| |
| − | | |
| − | Nurses care for individuals of all ages and cultural backgrounds who are healthy and ill in a [[Holistic health|holistic]] manner based on the individual's physical, emotional, psychological, intellectual, social, and spiritual needs. The profession combines physical science, social science, nursing theory, and technology in caring for those individuals. | |
| − | | |
| − | To work in the nursing profession, all nurses hold one or more credentials depending on their [[scope of practice]] and [[nurse education|education]]. In the United States, a [[Licensed Practical Nurse]] (LPN) works independently or with a [[Registered Nurse]] (RN). The most significant difference between an LPN and RN is found in the requirements for entry to practice, which determines entitlement for their scope of practice. RNs provide scientific, psychological, and technological knowledge in the care of patients and families in many health care settings. RNs may earn additional [[Nursing credentials and certifications|credentials]] or [[academic degree|degrees]].
| |
| − | | |
| − | In the United States, multiple educational paths will qualify a candidate to sit for the licensure examination as an RN. The [[#Associate Degree in Nursing|Associate Degree in Nursing]] (ADN) is awarded to the nurse who has completed a two-year undergraduate academic degree awarded by community colleges, junior colleges, technical colleges, and bachelor's degree-granting colleges and universities upon completion of a course of study usually lasting two years. It is also referred to as Associate in Nursing (AN), Associate of Applied Science in Nursing (AAS), or Associate of Science in Nursing (ASN).<ref>{{Cite web|title = Associate Degree in Nursing (ADN/ASN)|url = http://www.collegeatlas.org/associate-degree-in-nursing.html|website = collegeatlas.org|accessdate = 2015-10-29}}</ref> The [[#Bachelor of Science in Nursing|Bachelor of Science in Nursing]] (BSN) is awarded to the nurse who has earned an American four-year academic degree in the science and principles of nursing, granted by a tertiary education university or similarly accredited school. After completing either the LPN or either RN education programs in the United States, graduates are eligible to sit for a licensing examination to become a nurse, the passing of which is required for the nursing license. The [[National Council Licensure Examination|National Licensure Examination]] (NCLEX) test is a standardized exam (including multiple choice, select all that apply, fill in the blank and "hot spot" questions) that nurses take to become licensed. It costs two-hundred dollars to take the NCLEX. It examines a nurses ability to properly care for a client. Study books and practice tests are available for purchase.<ref>{{Cite web|title = NCLEX Exam {{!}} National Council Licensure Examination|url = http://www.allnursingschools.com/nursing-careers/article/nclex-exam/|website = allnursingschools.com|accessdate = 2015-10-29}}</ref>
| |
| − | | |
| − | Some nurses follow the traditional role of working in a hospital setting. Other options include: pediatrics, neonatal, maternity, OBGYN, geriatrics, ambulatory, and nurse anesthetists and informatics ([[eHealth]]). There are many other options nurses can explore depending on the type of degree and education acquired. RNs may also pursue different roles as [[advanced practice nurse]]s.
| |
| − | | |
| − | Nurses are not doctors' assistants. This is possible in certain situations, but nurses more often are independently caring for their patients or assisting other nurses.<ref>{{Cite web|title = 5 Myths about Registered Nurses – Ameritech College of Healthcare|url = http://ameritech.edu/blog/5-myths-registered-nurses-busted/|website = Ameritech College of Healthcare|publisher = |accessdate = 2015-10-15}}</ref> RNs treat patients, record their medical history, provide emotional support, and provide follow-up care. Nurses also help doctors perform diagnostic tests. Nurses are almost always working on their own or with other nurses. Nurses will assist doctors in the emergency room or in trauma care when help is needed.<ref>{{Cite web|title = Registered Nurse (RN) Career and Job Information|url = http://www.careerprofiles.info/nurse-career.html|website = careerprofiles.info|accessdate = 2015-10-15}}</ref>
| |
| − | | |
| − | ===Gender issues===
| |
| − | {{Main article|Men in nursing}}
| |
| − | [[File:Male Nurses- Life at Runwell Hospital, Wickford, Essex, 1943 D14313.jpg|thumb|right|upright=0.9|A nurse at Runwell Hospital, Wickford, Essex, in 1943]]
| |
| − | | |
| − | Despite equal opportunity legislation, nursing has continued to be a female-dominated profession.<ref>{{cite journal|title=BM 2004;328:141–142 (17 January) |pmc=314508 |pmid=14726342 |doi=10.1136/bmj.328.7432.141 |volume=328 |issue=7432 |year=2004 |journal=BMJ |pages=141–2 |vauthors=Grant VJ, Robinson E, Muir P }}</ref> For instance, the male-to-female ratio of nurses is approximately 1:19 in Canada and the United States.<ref>{{cite web|author=Patrick Sullivan |url=http://www.cmaj.ca/cgi/content/full/164/12/1738-b?ck=nck |title=Canada Medical Association Journal 12 June 2001; 164 (12) |publisher=Cmaj.ca |date=2001-06-12 |accessdate=2013-09-04}}</ref><ref>[http://bhpr.hrsa.gov/healthworkforce/reports/nursing/samplesurvey00/chapter3.htm 2000 National Sample Survey of Registered Nurses] {{webarchive |url=https://web.archive.org/web/20110422161539/http://bhpr.hrsa.gov/healthworkforce/reports/nursing/samplesurvey00/chapter3.htm |date=22 April 2011 }}</ref> This ratio is represented around the world. Notable exceptions include [[Francophone Africa]], which includes the countries of Benin, Burkina Faso, Cameroon, Chad, Congo, [[Côte d'Ivoire]], the [[Democratic Republic of Congo]], Djibouti, Guinea, Gabon, Mali, Mauritania, Niger, Rwanda, Senegal, and Togo, which all have more male than female nurses.<ref name="MIN">{{cite book|first1=Chad E. |last1=O'Lynn |first2=Russell E. |last2=Tranbarger |title=Men in Nursing: History, Challenges, and Opportunities|url=https://books.google.com/books?id=-Ag7TqTyIC0C&pg=PA225|year=2006|publisher=Springer Publishing Company|isbn=978-0-8261-0349-9|page=225}}</ref> In Europe, in countries such as [[Spain]], [[Portugal]], [[Czech Republic]] and [[Italy]], over 20% of nurses are male.<ref name="MIN"/> In the United Kingdom, 11% of nurses and midwives registered with the Nursing and Midwifery Council (NMC) are male.<ref>{{cite web|url=https://www.nmc.org.uk/globalassets/sitedocuments/annual_reports_and_accounts/equality-and-diversity-report-2015-16.pdf |title=Annual Equality and Diversity Profile, NMC 2015–2016}}</ref> The number of male registered nurses in the United States between 1980 and 2000s doubled.<ref>{{cite news|last1=Weintraub|first1=Arlene|title=Nursing: On the Critical List|agency=Business Week|date=June 3, 2002}}</ref>
| |
| − | | |
| − | Although females are more common, male nurses receive the same pay.<ref>{{Cite web|url = https://www.census.gov/people/io/files/Men_in_Nursing_Occupations.pdf|title = Men in Nursing Occupations|date = February 2013|accessdate = 2015-10-06|website = Census.gov|publisher = American Community Survey|url-status = dead|archiveurl = https://web.archive.org/web/20170713210226/https://www.census.gov/people/io/files/Men_in_Nursing_Occupations.pdf|archivedate = 13 July 2017|df = dmy-all}}</ref>{{contradict inline|Men in nursing#Professional life}}
| |
| | | | |
| − | == Theory and process ==
| + | The aim of the nursing community worldwide is for its professionals to ensure quality care for all, while maintaining their credentials, code of [[Nursing ethics|ethics]], standards, and competencies, and continuing their education. There are a number of educational paths to becoming a professional nurse, which vary greatly worldwide; all involve extensive study of [[nursing theory]] and practice as well as training in clinical skills. |
| | | | |
| − | {{Main article|Nursing theory|Nursing process}}
| + | To work in the nursing profession, all nurses hold one or more credentials depending on their [[scope of practice]] and [[nurse education|education]]. In the United States, a [[Licensed Practical Nurse]] (LPN) will work under the direction of a physician, mid-level practitioner, or [[Registered Nurse]] (RN). RNs provide scientific, psychological, and technological knowledge in the care of patients and families in many health care settings. |
| − | Nursing practice is the actual provision of nursing care. In providing care, nurses implement the [[nursing care plan]] using the [[nursing process]]. This is based around a specific [[nursing theory]] which is selected in consideration with the care setting and the population served. In providing nursing care, the nurse uses both nursing theory and best practice derived from [[nursing research]].<ref name=Weber2014>{{cite book | last = Weber | first = Janet | title = Nurses' handbook of health assessment | publisher = Wolters Kluwer/Lippincott Williams & Wilkins Health | location = Philadelphia | year = 2014 | isbn = 9781451142822 }}</ref>
| |
| | | | |
| − | In general terms, the nursing process is the method used to [[Nursing assessment|assess]] and [[Nursing diagnosis|diagnose]] needs, plan outcomes and interventions, implement interventions, and evaluate the outcomes of the care provided. Like other disciplines, the profession has developed different theories derived from sometimes diverse philosophical beliefs and [[paradigm]]s or [[worldview]]s to help nurses direct their activities to accomplish specific goals. | + | In the United States, multiple educational paths will qualify a candidate to sit for the licensing examination as an RN. The Associate Degree in Nursing (ADN) is awarded to the nurse who has completed a two-year undergraduate academic degree awarded by community colleges, junior colleges, technical colleges, and bachelor's degree-granting colleges and universities upon completion of a course of study usually lasting two years. The Bachelor of Science in Nursing (BSN) is awarded to the nurse who has earned an American four-year academic degree in the science and principles of nursing, granted by a tertiary education university or similarly accredited school. After completing either the LPN or either RN education programs in the United States, graduates are eligible to sit for a licensing examination to become a nurse, the passing of which is required for the nursing license.<ref>[https://www.allnursingschools.com/how-to-become-a-nurse/nclex-exam/ Everything Nurses Need to Know About the NCLEX Licensing Exam]. Retrieved April 2, 2020.</ref> |
| | | | |
| | ==Scope of activities== | | ==Scope of activities== |
| | + | RNs treat patients, record their medical history, provide emotional support, and provide follow-up care. Nurses also help doctors perform diagnostic tests, and may also assist doctors in the emergency room or in trauma care when help is needed.<ref>[https://www.careerprofiles.info/nurse-career.html Registered Nurse (RN)] ''Career Profiles''. Retrieved April 2, 2020.</ref> |
| | | | |
| | ===Activities of daily living assistance=== | | ===Activities of daily living assistance=== |
| − | {{main article|Activities of daily living assistance}}
| |
| | Assisting in activities of daily living (ADL) are skills required in nursing as well as other professions such as [[nursing assistant]]s. This includes assisting in patient mobility, such as moving an activity intolerant patient within bed. For hygiene, this often involves bed baths and assisting with urinary and bowel elimination. | | Assisting in activities of daily living (ADL) are skills required in nursing as well as other professions such as [[nursing assistant]]s. This includes assisting in patient mobility, such as moving an activity intolerant patient within bed. For hygiene, this often involves bed baths and assisting with urinary and bowel elimination. |
| | | | |
| | ===Medication=== | | ===Medication=== |
| − | Nurses do not have the authority to prescribe medications, although there are some exceptions. All medications administered by nurses must be from a medication prescription from a licensed practitioner, such as a [[physician]]. Nurses are legally responsible for the drugs they administer. There may be legal implications when there is an error in a prescription, and the nurse could be expected to have noted and reported the error. In the United States, nurses have the right to refuse any medication administration that they deem to be potentially harmful to the patient.<ref>Taylor, C. R., Lillis, C., LeMone, P., Lynn, P. (2011) Fundamentals of nursing: The art and science of nursing care. Philadelphia: Lippincott Williams & Wilkins, page 735-736.</ref>
| + | All medications administered by nurses must be from a medication prescription from a licensed practitioner, such as a [[physician]]. Nurses do not have the authority to prescribe medications, although there are some exceptions. Nurses are legally responsible for the drugs they administer. There may be legal implications when there is an error in a prescription, and the nurse could be expected to have noted and reported the error. In the United States, nurses have the right to refuse any medication administration that they deem to be potentially harmful to the patient.<ref name=Fundamentals>Carol Taylor, Pamela Lynn, and Jennifer Bartlett, ''Fundamentals of Nursing: The Art and Science of Person-Centered Care'' (LWW, 2018, ISBN 978-1496362179).</ref> |
| − | In the United Kingdom there are some nurses who have taken additional specialist training that allows them to prescribe any medications from their scope of practice.<ref name="rcn">{{cite web|url=https://www.rcn.org.uk/about-us/policy-briefings/pol-1512#tab1|title=RCN factsheet on nurse prescribing in the UK|website=rcn.org.uk|accessdate=July 20, 2019}}</ref> | + | |
| | + | In the United States, credentialed nurse practitioners (NP) can prescribe medication, including controlled substances. However, their degree of independence varies by state: In several states nurse practitioners have the explicit legal authority to prescribe; in others they must have a “collaborative relationship” or “protocol agreement” with a specific, supervising physician in order to prescribe medication.<ref>[https://www.nursepractitionerschools.com/faq/can-np-prescribe-medication/ Can Nurse Practitioners Prescribe Medication?] 'Nurse Practitioner Schools''. Retrieved April 2, 2020.</ref> A number of other countries around the world, including 13 European nations, allow qualified nurses to prescribe medication, some with full prescribing rights and others have restricted prescribing rights.<ref>Claudia B. Maier, [https://human-resources-health.biomedcentral.com/articles/10.1186/s12960-019-0429-6 Nurse prescribing of medicines in 13 European countries] ''Human Resources for Health'' 17 (2019). Retrieved April 2, 2020.</ref> |
| | | | |
| | ===Patient education=== | | ===Patient education=== |
| − | {{see also|Patient education}}
| + | Patient education is the process by which health professionals and others impart information to patients and their caregivers that will alter their health behaviors or improve their health status. The patient's family is often involved in the education. Effective patient education leads to fewer complications and hospital visits.<ref name=Fundamentals/> |
| − | The patient's family is often involved in the education. Effective patient education leads to fewer complications and hospital visits.<ref>Taylor, C. R., Lillis, C., LeMone, P., Lynn, P. (2011) Fundamentals of nursing: The art and science of nursing care. Philadelphia: Lippincott Williams & Wilkins, page 468.</ref> | |
| | | | |
| − | ==Specialties and practice settings== | + | ==Specialties== |
| − | {{Main article|List of nursing specialties}}
| + | Nursing is a very diverse [[health care profession]]. Nurses practice in a wide range of settings; some nurses follow the traditional role of working in a [[hospital]] setting while other work in more specialized settings such as private [[home care|homes]], [[school nursing|schools]], [[long-term care]] facilities, [[pharmaceutical companies]], and as researchers in laboratories, universities, and [[research institutions]]. |
| − | Nursing is the most diverse of all [[:category:health care occupations|health care professions]]. Nurses practice in a wide range of settings but generally nursing is divided depending on the needs of the person being nursed. | |
| | | | |
| − | The major populations are: | + | Generally nursing is divided according to the needs of the patients. The major populations are: |
| | *communities/public | | *communities/public |
| | *family/individual across the lifespan | | *family/individual across the lifespan |
| Line 150: |
Line 118: |
| | | | |
| | There are also specialist areas such as [[cardiac nursing]], [[orthopedic nursing]], [[palliative care]], [[perioperative nursing]], [[obstetrical nursing]], [[oncology nursing]], [[nursing informatics]], [[telenursing]], radiology, and [[emergency nursing]]. | | There are also specialist areas such as [[cardiac nursing]], [[orthopedic nursing]], [[palliative care]], [[perioperative nursing]], [[obstetrical nursing]], [[oncology nursing]], [[nursing informatics]], [[telenursing]], radiology, and [[emergency nursing]]. |
| − |
| |
| − | Nurses practice in a wide range of settings, including hospitals, private [[home care|homes]], [[school nursing|schools]], and [[pharmaceutical companies]]. Nurses work in [[Occupational health nursing|occupational health]] settings<ref>{{cite journal |author1=Draper Elaine |author2=LaDou Joseph |author3=Tennenhouse Dan J | year = 2011 | title = Occupational Health Nursing and the Quest for Professional Authority | url = | journal = New Solutions | volume = 21 | issue = 1| pages = 57–88 | doi=10.2190/ns.21.1.i|pmid=21411426 }}</ref> (also called industrial health settings), free-standing clinics and physician offices, [[nurse-led clinics]], [[long-term care]] facilities and camps. They also work on [[cruise ships]] and in [[Armed Forces|military service]]. Nurses act as advisers and consultants to the health care and insurance industries. Many nurses also work in the [[health advocacy]] and [[patient advocacy]] fields at companies such as [[Health Advocate]], Inc. helping in a variety of clinical and administrative issues.<ref>Schneider, John. "Healthcare advocacy experts aid workers." Miami Herald 31 August 2010</ref> Some are [[lawyer|attorneys]] and others work with attorneys as [[legal nurse consultant]]s, reviewing patient records to assure that adequate care was provided and testifying in court. Nurses can work on a temporary basis, which involves doing shifts without a contract in a variety of settings, sometimes known as ''per diem nursing'', ''agency nursing'' or ''travel nursing''. Nurses work as researchers in laboratories, universities, and [[research institutions]]. Nurses have also been delving into the world of informatics, acting as consultants to the creation of computerized charting programs and other software. Nurse authors publish articles and books to provide essential reference materials.
| |
| | | | |
| | ==Occupational hazards== | | ==Occupational hazards== |
| − | [[File:Sleep Deprivation – Shift Work & Long Work Hours Put Nurses at Risk.webm|thumb|A video describing occupational hazards that exist among nurses]]
| + | The fast-paced and unpredictable nature of health care places nurses at risk for injuries and illnesses, including high [[occupational stress]]. Nurses consistently identify stress as a major work-related concern and have among the highest levels of occupational stress when compared to other professions. This stress is caused by the environment, psychosocial stressors, and the demands of nursing, including new technology that must be mastered, the emotional labor involved in nursing, physical labor, [[shift work]], and high workload. This stress puts nurses at risk for short-term and long-term health problems, including [[sleep disorders]], [[major depressive disorder|depression]], [[Death|mortality]], psychiatric disorders, stress-related illnesses, and illness in general. Nurses are at risk of developing [[compassion fatigue]] and moral [[distress (medicine)|distress]], which can worsen mental health. They also have very high rates of [[occupational burnout]] and [[emotional exhaustion]], which increase the risk for illness, medical error, and suboptimal care provision.<ref name=Stress>Rashaun Roberts, Paula L. Grubb, and James W. Grosch, [https://www.medscape.com/viewarticle/765974 Alleviating Job Stress in Nurses] ''Medscape'', June 25, 2012. Retrieved April 2, 2020.</ref> |
| − | Internationally, there is a serious shortage of nurses.<ref>{{cite journal |last1=Buchanan |first1=J. |title=Global nursing shortages |journal=BM |volume=324 |issue=7340 |pages=751–2 |year=2002 |pmid=11923146 |pmc=1122695 |doi=10.1136/bmj.324.7340.751}}</ref> One reason for this shortage is due to the work environment in which nurses practice. In a recent review of the empirical human factors and ergonomic literature specific to nursing performance, nurses were found to work in generally poor environmental conditions. Some countries and states have passed legislation regarding acceptable nurse-to-patient ratios.
| |
| − | | |
| − | The fast-paced and unpredictable nature of health care places nurses at risk for injuries and illnesses, including high [[occupational stress]]. Nursing is a particularly stressful profession, and nurses consistently identify stress as a major work-related concern and have among the highest levels of occupational stress when compared to other professions. This stress is caused by the environment, psychosocial stressors, and the demands of nursing, including new technology that must be mastered, the emotional labor involved in nursing, physical labor, [[shift work]], and high workload. This stress puts nurses at risk for short-term and long-term health problems, including [[sleep disorders]], [[major depressive disorder|depression]], [[Death|mortality]], psychiatric disorders, stress-related illnesses, and illness in general. Nurses are at risk of developing [[compassion fatigue]] and moral [[distress (medicine)|distress]], which can worsen mental health. They also have very high rates of [[occupational burnout]] (40%) and [[emotional exhaustion]] (43.2%). Burnout and exhaustion increase the risk for illness, medical error, and suboptimal care provision.<ref name=":0">{{Cite web|url = http://www.medscape.com/viewarticle/765974|title = Alleviating Job Stress in Nurses|date = 25 June 2012|accessdate = |website = NIOSH: Workplace Safety and Health|publisher = Medscape and NIOSH|last = Roberts|first = Rashaun|last2 = Grubb|first2 = Paula L.|last3 = Grosch|first3 = James W.}}</ref> | |
| | | | |
| − | Nurses are also at risk for violence and abuse in the workplace.<ref>{{cite web |url = http://blogs.cdc.gov/niosh-science-blog/2013/08/12/hcwviolence-prevention/ |title = Free On-line Violence Prevention Training for Nurses |date = 12 August 2013 |first1 = Dan |last1 = Hartley |first2 = Marilyn |last2 = Ridenour |accessdate = 2015-01-15 |publisher = National Institute for Occupational Safety and Health}}</ref> Violence is typically perpetrated by non-staff (e.g. patients or family), whereas abuse is typically perpetrated by other hospital personnel. Of American nurses, 57% reported in 2011 that they had been threatened at work; 17% were physically assaulted.<ref name=":0" /> | + | Nurses are also at risk for violence and abuse in the workplace.<ref>Dan Hartley and Marilyn Ridenour, [https://blogs.cdc.gov/niosh-science-blog/2013/08/12/hcwviolence-prevention/ Free On-line Violence Prevention Training for Nurses] ''National Institute for Occupational Safety and Health'', August 12, 2013. Retrieved April 2, 2020.</ref> Violence is typically perpetrated by non-staff (such as patients or family), whereas abuse is typically perpetrated by other hospital personnel. |
| | | | |
| | ===Prevention=== | | ===Prevention=== |
| − | There are a number of interventions that can mitigate the occupational hazards of nursing. They can be individual-focused or organization-focused. Individual-focused interventions include [[stress management]] programs, which can be customized to individuals. Stress management programs can reduce anxiety, sleep disorders, and other symptoms of stress. Organizational interventions focus on reducing stressful aspects of the work environment by defining stressful characteristics and developing solutions to them. Using organizational and individual interventions together is most effective at reducing stress on nurses.<ref name=":0"/> In some Japanese hospitals, [[Powered_exoskeleton#Medical|powered exoskeletons]] are used.<ref>{{cite news|last1=Gilhooly|first1=Rob|title=Exoskeletons await in work/care closet|url=http://www.japantimes.co.jp/life/2012/06/17/general/exoskeletons-await-in-workcare-closet/#.UhQ2XYZIN8E|accessdate=21 August 2013|work=The Japan Times Online|date=17 June 2012}}</ref> Lumbar supports (ie [[back belt]]s) have also been trialled.<ref>[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2078392/ Interventions to prevent back pain and back injury in nurses: a systematic review]</ref> | + | There are a number of interventions that can mitigate the occupational hazards of nursing. Individual-focused interventions include [[stress management]] programs, which can be customized to individuals, and which can reduce anxiety, sleep disorders, and other symptoms of stress. Physical supports, such as lumbar supports for the back, may also be used to reduce physical injury and alleviate pain.<ref>Anna P. Dawson, Skye N. McLennan, Stefan D. Schiller, Gwendolen A. Jull, Paul W. Hodges, and Simon Stewart, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2078392/ Interventions to prevent back pain and back injury in nurses: a systematic review] ''Occupational and Environmental Medicine'', 64(10) (2007): 642–650. Retrieved April 2, 2020.</ref>.<ref>Anna P. Dawson, Skye N. McLennan, Stefan D. Schiller, Gwendolen A. Jull, Paul W. Hodges, and Simon Stewart, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2078392/ Interventions to prevent back pain and back injury in nurses: a systematic review] ''Occupational and Environmental Medicine'', 64(10) (2007): 642–650. Retrieved April 2, 2020.</ref> Organizational interventions focus on reducing stressful aspects of the work environment by defining stressful characteristics and developing solutions to them. Using organizational and individual interventions together is most effective at reducing stress on nurses.<ref name=Stress/> |
| − | | |
| − | ==Worldwide==
| |
| − | | |
| − | ===Australia===
| |
| − | {{main article|Nursing in Australia}}
| |
| − | Catholic religious institutes were influential in the development of Australian nursing, founding many of Australia's hospitals – the Irish [[Sisters of Charity of Australia|Sisters of Charity]] were first to arrive in 1838 and established [[St Vincent's Hospital, Sydney]] in 1857 as a free hospital for the poor. They and other orders like the [[Sisters of Mercy]], and in aged care the Sisters of the Little Company of Mary and [[Little Sisters of the Poor]] founded hospitals, hospices, research institutes and aged care facilities around Australia.<ref>{{cite web|url=http://national.stvincents.com.au/history.php |archiveurl=https://web.archive.org/web/20100402062826/http://national.stvincents.com.au/history.php |archivedate=2010-04-02 |title=Internet Archive Wayback Machine |date=6 July 2011 |accessdate=2012-07-31}}</ref><ref>{{cite web|url=http://www.littlesistersofthepoor.org.au/ |title=Little Sisters of the Poor Oceania |publisher=Littlesistersofthepoor.org.au |date= |accessdate=2012-07-31}}</ref>
| |
| − | | |
| − | A census in the 1800s found several hundred nurses working in Western Australia during the colonial period of history, this included Aboriginal female servants who cared for the infirm.<ref>"But Westward Look" by author</ref>
| |
| − | | |
| − | The state nursing licensing bodies amalgamated in Australia in 2011 under the federal body AHPRA (Australian Health Practitioner Registration Authority).<ref>{{cite journal|last1=Ralph|first1=Nicholas|last2=Birks|first2=Melanie|last3=Chapman|first3=Ysanne|title=The accreditation of nursing education in Australia|journal=Collegian|date=November 2013|doi=10.1016/j.colegn.2013.10.002|pmid=26285403|volume=22|issue=1|pages=3–7|url=http://eprints.usq.edu.au/25901/14/Ralph_Birks_Coll_SV.pdf}}</ref> Several divisions of nursing license is available and recognized around the country.
| |
| − | *Enrolled nurses may initiate some oral medication orders with a specific competency now included in national curricula but variable in application by agency.
| |
| − | *Registered nurses hold a university degree (enrolled nurses can progress to registered nurse status and do get credit for previous study).
| |
| − | *Nurse practitioners have started emerging from postgraduate programs and work in private practice.
| |
| − | *Mental health nurses must complete further training as advanced mental health practitioners in order to administer client referrals under the ''Mental Health Act''.
| |
| − | | |
| − | Australia enjoys the luxury of a national curriculum for vocational nurses, trained at Technical and Further Education (TAFE) colleges or private Registered Training Organization (RTO). Enrolled and registered nurses are identified by the department of immigration as an occupational area of need, although registered nurses are always in shorter supply, and this increases in proportion with specialization.
| |
| − | | |
| − | In 1986 there were a number of rolling industrial actions around the country, culminating when five thousand Victorian nurses went on strike for eighteen days. The hospitals were able to function by hiring casual staff from each other's striking members, but the increased cost forced a decision in the nurses' favor <ref>[http://www.anu.edu.au/polsci/marx/interventions/rebelwomen/nurses.htm Nurses' militancy stemmed from two different kinds of experiences]. Anu.edu.au (1983-11-19). Retrieved on 2013-07-28.</ref>
| |
| − | | |
| − | ===European Union===
| |
| − | | |
| − | In the European Union, the profession of nurse is regulated. A profession is said to be regulated when access and exercise is subject to the possession of a specific professional qualification. The regulated professions database contains a list of regulated professions for nurse<ref name="europa">{{cite web|url=http://ec.europa.eu/internal_market/qualifications/regprof/index.cfm?action=profession&id_profession=12402&tab=countries|title=Regulated professions database – European Commission|website=ec.europa.eu|accessdate=2017-12-10}}</ref> in the European Union (EU) member states, European Economic Area (EEA) countries, and Switzerland. This list is covered by the Directive 2005/36/EC.
| |
| − | | |
| − | ===Iran===
| |
| − | See [[Nursing in Iran]]
| |
| − | | |
| − | ===United Kingdom===
| |
| − | | |
| − | {{Main article|Nursing in the United Kingdom}}
| |
| − | | |
| − | To practice lawfully as a registered nurse in the United Kingdom, the practitioner must hold a current and valid registration with the [[Nursing and Midwifery Council]]. The title "Registered Nurse" can only be granted to those holding such registration. This protected title is laid down in the Nurses, Midwives and Health Visitors Act, 1997.<ref name="ACT">United Kingdom Government [http://www.opsi.gov.uk/ACTS/acts1997/1997024.htm Nurses, Midwives and Health Visitors Act, 1997.] London: HMSO, 1997.</ref> From April 2016, nurses in the United Kingdom are expected to revalidate every three years which involves providing evidence of further development and active practice.<ref>{{cite news |url=https://www.theguardian.com/healthcare-network/2016/feb/24/revalidation-nurses-midwives-how-it-works |title=How revalidation will work for nurses and midwives |first=Linda |last=Jackson |work=The Guardian |date=24 February 2016 |accessdate=2016-10-08}}</ref><ref>{{Cite news|url=https://nursingnotes.co.uk/nmc-revalidation-to-begin-in-april-2016/|title=NMC Revalidation to begin in April 2016|date=2015-10-16|work=NursingNotes|access-date=2017-06-01|language=en-GB}}</ref>
| |
| − | | |
| − | ====First and second level====
| |
| − | | |
| − | First-level nurses make up the bulk of the registered nurses in the UK. They were previously known by titles such as Registered General Nurse (RGN), Registered Sick Children's Nurse (RSCN), Registered Mental Nurse (RMN), and Registered Nurse (for the) Mentally Handicapped (RNMH). The titles used now are similar, including Registered Nurse Adult (RNA), Registered Nurse Child (RNC), Registered Nurse Mental Health (RNMH), and Registered Nurse (of) Learning Disabilities (RNLD). Second-level nurse training is no longer provided; however, they are still legally able to practice in the United Kingdom as a registered nurse. Many have now either retired or undertaken conversion courses to become first-level nurses. They are entitled to refer to themselves as registered nurses as their registration is on the Nursing & Midwifery Council register of nurses, although most refer to themselves as Enrolled Nurses (ENs) or State Enrolled Nurses (SENs).
| |
| − | | |
| − | ====Advanced practice====
| |
| − | | |
| − | * '''Nurse practitioners''' – Most of these nurses obtain a minimum of a master's degree and a desired post grad certificate. They often perform roles similar to those of physicians and physician assistants. They can prescribe medications as independent or supplementary prescribers, although they are still legally regulated, unlike physician's assistants. Most Nurse Practitioners (NPs) have referral and admission rights to hospital specialties. They commonly work in [[primary care]] (e.g. General Practitioner (GP) surgeries), [[emergency department| Accident and Emergency (A&E) departments]], or pediatrics although they are increasingly being seen in other areas of practice. In the UK, the title "nurse practitioner" is legally protected.
| |
| − | * '''Specialist community public health nurses''' – traditionally [[district nurse]]s and [[health visitor]]s, this group oversees research and publication activities.
| |
| − | * '''Lecturer-practitioners (also called practice education facilitators)''' – these nurses work both in the National Health Service (NHS), and in universities. They typically work 2–3 days per week in each setting. In university, they train pre-registration student nurses (see below), and often teach on specialist courses post-registration nurses.
| |
| − | * '''Lecturers''' – these nurses are not employed by the NHS. Instead they work full-time in universities, both teaching and performing research.
| |
| − | | |
| − | ====Managers====
| |
| − | | |
| − | Many nurses who have worked in clinical settings for a long time choose to leave clinical nursing and join the ranks of the NHS management. This used to be seen as a natural career progression for those who had reached ward management positions, however with the advent of specialist nursing roles (see above), this has become a less attractive option.
| |
| − | | |
| − | Nonetheless, many nurses fill positions in the senior management structure of NHS organizations, some even as board members. Others choose to stay a little closer to their clinical roots by becoming clinical nurse managers or ''[[Matron|modern matrons]]''.
| |
| − | | |
| − | ====Nurse education====
| |
| − | | |
| − | =====Pre-registration=====
| |
| − | | |
| − | To become a registered nurse, one must complete a program recognised by the [[Nursing and Midwifery Council]] (NMC). Currently, this involves completing a [[academic degree|degree]], available from a range of [[:Category:Nursing schools in the United Kingdom|universities offering these courses]], in the chosen branch specialty (see below), leading to both an academic award and professional registration as a 1st level registered nurse. Such a course is a 50/50 split of learning in university (i.e. through lectures, assignments and examinations) and in practice (i.e. supervised patient care within a hospital or community setting).
| |
| − | | |
| − | These courses are three (occasionally four) years' long. The first year is known as the common foundation program (CFP), and teaches the basic knowledge and skills required of all nurses. Skills included in the CFP may include communication, taking observations, administering medication and providing personal care to patients. The remainder of the program consists of training specific to the student's chosen branch of nursing. These are:
| |
| − | | |
| − | * Adult nursing.
| |
| − | * Child nursing.
| |
| − | * Mental health nursing.
| |
| − | * Learning disabilities nursing.
| |
| − | | |
| − | As of 2013, the Nursing and Midwifery Council will require all new nurses qualifying in the UK to hold a degree qualification.<ref name="http://www.nmc-uk.org/Get-involved/Consultations/Past-consultations/By-year/Pre-registration-nursing-education-Phase-2/Changes-to-pre-registration-nursing-programmes-FAQs-/">{{cite web |url=http://www.nmc-uk.org/Get-involved/Consultations/Past-consultations/By-year/Pre-registration-nursing-education-Phase-2/Changes-to-pre-registration-nursing-programmes-FAQs-/ |title=Changes to pre-registration nursing programmes: FAQs | Nursing and Midwifery Council |publisher=Nmc-uk.org |date=20 April 2010 |accessdate=2011-08-21 |url-status=dead |archiveurl=https://web.archive.org/web/20110727073118/http://www.nmc-uk.org/Get-involved/Consultations/Past-consultations/By-year/Pre-registration-nursing-education-Phase-2/Changes-to-pre-registration-nursing-programmes-FAQs-/ |archivedate=27 July 2011 |df=dmy-all }}</ref> However, those nurses who hold a diploma, or even a certificate in nursing are still able to legally practice in the UK, although they are able to undertake university modules to obtain enough credits to top up to a degree.
| |
| − | | |
| − | [[Midwifery]] training is similar in length and structure, but is sufficiently different that it is not considered a branch of nursing. There are shortened (18 month) programs to allow nurses already qualified in the adult branch to hold dual registration as a nurse and a midwife. Shortened courses lasting 2 years also exist for graduates of other disciplines to train as nurses. This is achieved by more intense study and a shortening of the common foundation program.<ref name="NMC">Nursing and Midwifery Council [http://www.nmc.org.uk Pre-registration training.] London: NMC, 2003.</ref>
| |
| − | | |
| − | {{As of|2016}} student nurses in England and Wales can apply for a [[bursary]] from the government to support them during their nurse training, and may also be eligible for a student loan, although there has been speculation that this will not be available in the future.<ref name="nursingtimes">{{cite web|url=https://www.nursingtimes.net/news/education/bursary-system-unsustainable-claims-minister-03-10-2016/|title=Student bursary system 'unsustainable', claims minister in response to editors | News|website=Nursing Times|accessdate=2017-12-10}}</ref> Student nurses in Scotland still receive a standard bursary which is not means tested, and their tuition fees continue to be paid – however, they are not eligible for student loans.
| |
| − | | |
| − | Before Project 2000, nurse education was the responsibility of hospitals and was not based in universities; hence many nurses who qualified prior to these reforms do not hold an academic award.
| |
| − | | |
| − | =====Post-registration=====
| |
| − | | |
| − | After the point of initial registration, there is an expectation that all qualified nurses will continue to update their skills and knowledge. The Nursing and Midwifery Council insists on a minimum of 35 hours of education every three years, as part of its post registration education and practice (PREP) requirements.<ref name="http://www.nmc-uk.org/Nurses-and-midwives/Advice-by-topic/A/Advice/Post-Registration-Education-and-Practice-Prep-requirements-for-midwives/">{{cite web |url=http://www.nmc-uk.org/Nurses-and-midwives/Advice-by-topic/A/Advice/Post-Registration-Education-and-Practice-Prep-requirements-for-midwives/ |title=Post Registration Education and Practice (Prep) requirements for midwives | Nursing and Midwifery Council |publisher=Nmc-uk.org |accessdate=2011-08-21 |url-status=dead |archiveurl=https://web.archive.org/web/20101126092059/http://www.nmc-uk.org/Nurses-and-midwives/Advice-by-topic/A/Advice/Post-Registration-Education-and-Practice-Prep-requirements-for-midwives/ |archivedate=26 November 2010 |df=dmy-all }}</ref>
| |
| − | | |
| − | There are also opportunities for many nurses to gain additional clinical skills after qualification. [[Cannulation]], [[venipuncture]], [[Intravenous therapy|intravenous drug therapy]] and [[urinary catheterization|male catheterization]] are the most common, although there are many others (such as [[Advanced Life Support|advanced life support]]), which some nurses undertake.
| |
| − | | |
| − | Many nurses who qualified with a diploma choose to upgrade their qualification to a degree by studying part-time. Many nurses prefer this option to gaining a degree initially, as there is often an opportunity to study in a specialist field as a part of this upgrading. Financially, in England, it was also much more lucrative, as diploma students get the full bursary during their initial training, and employers often pay for the degree course as well as the nurse's salary.<ref name="Nursing and Midwifery Education, 2007">Nursing and Midwifery Education, 2007</ref>
| |
| − | | |
| − | To become specialist nurses (such as nurse consultants, nurse practitioners etc.) or nurse educators, some nurses undertake further training above bachelor's degree level. Master's degrees exist in various healthcare related topics, and some nurses choose to study for PhDs or other higher academic awards. [[District nurse]]s and [[health visitor]]s are also considered specialist nurses, and to become such they must undertake specialist training. This is a one-year full-time degree.
| |
| − | | |
| − | All newly qualifying [[district nurse]]s and [[health visitor]]s are trained to prescribe from the Nurse Prescribers' Formulary, a list of medications and dressings typically useful to those carrying out these roles. Many of these (and other) nurses will also undertake training in independent and supplementary prescribing, which allows them (as of 1 May 2006) to prescribe almost any drug in the [[British National Formulary]]. This has been the cause of a great deal of debate in both medical and nursing circles.<ref name="BFN">{{cite web|url=http://bnf.org/bnf/index.htm|title=BNF Publications|author=BNF Publications|publisher=}}</ref>
| |
| − | | |
| − | ===Canada===
| |
| − | | |
| − | {{Main article|Nursing in Canada}}
| |
| − | | |
| − | ====History====
| |
| − | | |
| − | Canadian nursing dates back to 1639 in [[Quebec]] with the Augustine nuns.<ref name="test">[http://www.cna-nurses.ca/CNA/nursing/certification/specialties/default_e.aspx Link text] {{webarchive|url=https://web.archive.org/web/20111229233442/http://www.cna-nurses.ca/cna/nursing/certification/specialties/default_e.aspx |date=29 December 2011 }}.</ref> These nuns were trying to open a mission that cared for the spiritual and physical needs of patients. The establishment of this mission created the first nursing apprenticeship training in North America.<ref name="test" /> In the nineteenth century, some Catholic orders of nursing were trying to spread their message across Canada. Most nurses were female and only had an occasional consultation with a physician. Towards the end of the nineteenth century, hospital care and medical services had been improved and expanded. Much of this was due to Nightingale's influence. In 1874 the first formal nursing training program was started at the General and Marine Hospital in St. Catharines in Ontario.<ref name="test" />
| |
| − | | |
| − | ====Education====
| |
| − | All Canadian nurses and prospective nurses are heavily encouraged by the [[Canadian Nurses Association]] to continue their education to receive a [[bachelor's degree]]. This degree may result in better patient outcomes.{{citation needed|date=March 2019}} All Canadian provinces and territories, with the exception of the [[Yukon]] and [[Quebec]], require that all nurses have a bachelor's degree.<ref name="test" /> The length of time generally required to obtain this degree is four years. However, some Canadian universities offer a condensed program that is two years in length.<ref name="test" />
| |
| − | | |
| − | Nursing specialty certification is available through the [[Canadian Nurses Association]] in 22 practice areas,<ref name="test" /> including:
| |
| − | *cardiovascular nursing
| |
| − | *community health nursing
| |
| − | *[[critical care nursing]]
| |
| − | *pediatric critical care nursing
| |
| − | *emergency nursing
| |
| − | *gastroenterology nursing
| |
| − | *[[gerontological nursing]]
| |
| − | *hospice palliative care nursing
| |
| − | *medical-surgical nursing
| |
| − | *neonatal nursing
| |
| − | *nephrology nursing
| |
| − | *neuroscience nursing
| |
| − | *occupational health nursing
| |
| − | *oncology nursing
| |
| − | *[[orthopedic nursing]]
| |
| − | *pediatric nursing
| |
| − | *peri-anesthesia nursing
| |
| − | *perinatal nursing
| |
| − | *peri-operative nursing
| |
| − | *psychiatric and mental health nursing
| |
| − | *rehabilitation nursing
| |
| − | *wound, ostomy and continence nursing
| |
| − | | |
| − | Nursing specialty certification generally requires practice experience and passing a test that is based on competencies for that specific medical or surgical domain in which nursing care is provided. The certification in gerontological nursing, which involves providing care to the elderly, is offered to not only RNs and NPs but also LPNs.
| |
| − | | |
| − | === Israel ===
| |
| − | Nurses in Israel have a wide variety of responsibilities, including hospital care, patient education, wound care, prenatal monitoring, midwifery, and well-baby clinics.
| |
| − | | |
| − | ===Japan===
| |
| − | | |
| − | {{main article|Nursing in Japan}}
| |
| − | | |
| − | ====History====
| |
| − | Nursing was not an established part of Japan's healthcare system until 1899 with the Midwives Ordinance.<ref name="nurse">{{cite web|title=Nursing in Japan – Overview of Japanese Nursing System|url=http://www.nurse.or.jp/jna/english/nursing/system.html|accessdate=25 February 2018|website=nurse.or.jp}}</ref> From there the Registered Nurse Ordinance came into play in 1915. This established a legal substantiation to registered nurses all over Japan. A new law geared towards nurses was created during [[World War II]]: the ''Public Health Nurse, Midwife and Nurse Law'', established in 1948.<ref name="test" /> It established educational requirements, standards and licensure. There has been a continued effort to improve nursing in Japan. In 1992 the Nursing Human Resource Law was passed.<ref name="test" /> This law created the development of new university programs for nurses. Those programs were designed to raise the education level of the nurses so that they could be better suited for taking care of the public.
| |
| − | | |
| − | ====Types of nurses====
| |
| − | | |
| − | Japan only recognizes four types of nursing and they are [[Public Health Nursing]], [[Midwifery]], Registered Nursing and Assistant Nursing.
| |
| − | | |
| − | =====Public health=====
| |
| − | | |
| − | This type of nursing is designed to help the public and is also driven by the public's needs. The goals of public health nurses are to monitor the spread of disease, keep vigilant watch for environmental hazards, educate the community on how to care for and treat themselves, and train for community disasters.
| |
| − | | |
| − | =====Midwifery=====
| |
| − | | |
| − | Nurses that are involved with midwifery are independent of any organization. A [[midwife]] takes care of a pregnant woman during labour and postpartum. They assist with things like breastfeeding and caring for the child.
| |
| − | | |
| − | =====Nursing Assistant=====
| |
| − | | |
| − | Individuals who are assistant nurses follow orders from a registered nurse. They report back to the licensed nurse about a patient's condition. Assistant nurses are always supervised by a licensed registered nurse.
| |
| − | | |
| − | ====Education====
| |
| − | | |
| − | In 1952 Japan established the first nursing university in the country.<ref name="test" /> An [[Associate of Science in Nursing|associate degree]] was the only level of certification for years. Soon people began to want nursing degrees at a higher level of education. Soon the [[Bachelor of Science in Nursing|Bachelor's Degree in Nursing]] (BSN) was established. Currently, Japan offers [[Doctorate in Nursing|doctorate]]-level degrees of nursing in a good number of its universities.
| |
| − | | |
| − | There are three ways that an individual could become a registered nurse in Japan. After obtaining a high school degree the person could go to a nursing university for four years and earn a bachelor's degree, go to a junior nursing college for three years or go to a nursing school for three years.<ref name="test" /> Regardless of where the individual attends school they must take the national exam. Those who attended a nursing university have a bit of an advantage over those who went to a nursing school. They can take the national exam to be a registered nurse, public health nurse or midwife. In the cases of becoming a midwife or a public health nurse, the student must take a one-year course in their desired field after attending a nursing university and passing the national exam to become a registered nurse. The nursing universities are the best route for someone who wants to become a nurse in Japan.<ref name="test" /> They offer a wider range of general education classes and they also allow for a more rigid teaching style of nursing. These nursing universities train their students to be able to make critical and educated decisions when they are out in the field. Physicians are the ones who are teaching the potential nurses because there are not enough available nurses to teach students. This increases the dominance that physicians have over nurses.
| |
| | | | |
| − | Students that attend a nursing college or just a nursing school receive the same degree as one who graduated from a nursing university would, but they do not have the same educational background. The classes offered at nursing colleges and nursing schools are focused on more practical aspects of nursing. These institutions do not offer many general education classes, so students who attend these schools will solely be focusing on their nursing educations while they are in school. Students who attend a nursing college or school do have the opportunity to become a [[midwife]] or a public health nurse. They have to go through a training institute for their desired field after graduating from the nursing school or college.<ref name="test" /> Japanese nurses never have to renew their licenses. Once they have passed their exam, they have their license for life.<ref name="test" />
| + | ===Shortage of nurses=== |
| − | | + | Internationally, there is a serious shortage of nurses.<ref>James Buchan, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1122695/ Global nursing shortages] ''BMJ'' 324(7340) (2002): 751–752. Retrieved April 2, 2020.</ref> One reason for this shortage is due to the work environment in which nurses practice. In a recent review of the empirical human factors and ergonomic literature specific to nursing performance, nurses were found to work in generally poor environmental conditions. Some countries and states have passed legislation regarding acceptable nurse-to-patient ratios. |
| − | ====Today==== | |
| − | | |
| − | Like the United States, Japan is in need of more nurses. The driving force behind this need is the fact that country is aging and needs more medical care for its people. However, the number of available nurses does not seem to be increasing. Nurses face poor working conditions and low social status, and there is a cultural idea that married women quit their jobs for family responsibilities.<ref name="nurse2">{{ref web|title=Nursing in Japan – Working conditions in Japan|url=http://www.nurse.or.jp/jna/english/nursing/employment.html|accessdate=25 February 2018|website=nurse.or.jp}}</ref> On average, Japanese nurses make around 280,000 yen a month, and it is one of the higher paying jobs. However, physicians make twice as much as nurses.<ref name="worldsalaries">{{cite web|title=Professional Nurse Salaries – International Comparison
| |
| − | |url=http://www.worldsalaries.org/professionalnurse.shtml|website=worldsalaries.org|accessdate=25 February 2018}}</ref> Similar to other cultures, the Japanese people view nurses as subservient to physicians. According to the [[American Nurses Association]] article on Japan, "nursing work has been described using negative terminology such as 'hard, dirty, dangerous, low salary, few holidays, minimal chance of marriage and family, and poor image.'"
| |
| − | | |
| − | There are organizations that unite Japanese nurses like the [[Japanese Nursing Association]] (JNA); the JNA is a professional organization and not a union. Members of the JNA lobby politicians and produces publications about nursing. According to the American Nurses Association's article on Japan, the JNA "works toward the improvement in nursing practice through many activities including the development of a policy research group to influence policy development, a code of ethics for nurses, and standards of nursing practice." The JNA also provides certification for specialists in mental health, oncology and community health. <ref name="test" /> There are other organizations, including some that categorize nurses by specialty, like emergency nursing or disaster nursing. One of the older unions that relates to nursing is the Japanese Federation of Medical Workers Union, which was created in 1957.<ref name="test" /> It is a union that includes physicians as well as nurses. This organization was involved with the '''Nursing Human Resource Law'''.<ref name="test" />
| |
| − | | |
| − | ===Spain===
| |
| − | See [[Nursing in Spain]]
| |
| − | | |
| − | ===Taiwan===
| |
| − | {{main article|nursing in Taiwan}}
| |
| − | *In [[Taiwan]], the [[Ministry of Health and Welfare (Taiwan)|Ministry of Health and Welfare]] is in charge of the regulation of nursing.<ref>{{cite web|url=http://www.mohw.gov.tw/EN/Ministry/Index.aspx|title=Ministry of Health and Welfare|publisher=}}</ref> The Taiwan Union of Nurses Association (TUNA) is the union unit in Taiwan, fighting for nurses on payment and working time issues.<ref>{{cite web|url=http://www.nurse.org.tw/English/Default.aspx|title=中華民國護理師護士公會全國聯合會|publisher=}}</ref>
| |
| − | | |
| − | ===United States===
| |
| − | | |
| − | [[File:Poston, Arizona. Registered nurse, Mrs. Edythe Sasser, is assisited by Yoshiko Konatsu, nurse's aid . . . - NARA - 537104.jpg|thumb|Two nurses in Arizona, 1943]]
| |
| − | {{Main article|Nursing in the United States|History of nursing in the United States}}
| |
| − | In the US, scope of practice is determined by the state or territory in which a nurse is licensed. Each state has its own laws, rules, and regulations governing nursing care. Usually the making of such rules and regulations is delegated to a state [[board of nursing]], which performs day-to-day administration of these rules, licenses for nurses and nursing assistants, and makes decisions on nursing issues. In some states, the terms "nurse" or "nursing" may only be used in conjunction with the practice of a [[registered nurse]] (RN) or [[Licensed Practical Nurse|licensed practical or vocational nurse]] (LPN/LVN).
| |
| − | | |
| − | In the hospital setting, registered nurses often delegate tasks to LPNs and [[unlicensed assistive personnel]].
| |
| − | | |
| − | RNs are not limited to employment as bedside nurses. They are employed by physicians, attorneys, insurance companies, governmental agencies, community/public health agencies, private industry, school districts, ambulatory surgery centers, among others. Some registered nurses are independent consultants who [[self-employed|work for themselves]], while others work for large manufacturers or chemical companies. Research nurses conduct or assist in the conduct of research or evaluation (outcome and process) in many areas such as biology, psychology, human development, and health care systems.
| |
| − | | |
| − | Many employers offer flexible work schedules, child care, educational benefits, and bonuses. About 21 percent of registered nurses are union members or covered by union contract.<ref name="United States Department of Labor Bureau of Labor Statistics">United States Department of Labor Bureau of Labor Statistics</ref>
| |
| − | | |
| − | Nursing is the nation's largest health care profession. In 2017, there were more than 4,015,250 registered nurses and 922,196 licensed practical nurses nationwide.<ref>The U.S. Nursing Workforce in 2018 and Beyond
| |
| − | | |
| − | Journal of Nursing Regulation , Volume 8, Issue 4, S3 - S6</ref> Of all licensed RNs, 2.6 million or 84.8% are employed in nursing. Nurses comprise the largest single component of hospital staff, are the primary providers of hospital patient care, and deliver most of the nation's long-term care. The primary pathway to professional nursing, as compared to technical-level practice, is the four-year Bachelor of Science in Nursing (BSN) degree. Registered nurses are prepared either through a BSN program; a three-year associate degree in nursing; or a three-year hospital training program, receiving a hospital diploma. All take the same state licensing exam. (The number of diploma programs has declined steadily—to less than 10 percent of all basic RN education programs—as nursing education has shifted from hospital-operated instruction into the college and university system.)
| |
| − | | |
| − | ====Educational and licensure requirements====
| |
| − | | |
| − | =====Diploma in Nursing=====
| |
| − | {{main article|Diploma in Nursing}}
| |
| − | The oldest method of nursing education is the hospital-based diploma program, which lasts approximately three years. Students take between 30 and 60 credit hours in [[anatomy]], [[physiology]], [[microbiology]], [[nutrition]], [[chemistry]], and other subjects at a college or university, then move on to intensive nursing classes. Until 1996, most RNs in the US were initially educated in nursing by diploma programs.<ref name="ANA">American Nurses Association. [http://www.ana.org/readroom/fsdemogr2.htm#education "Nursing Facts: Today's Registered Nurse – Numbers and Demographics"] Washington, D.C., American Nurses Association, 2006.</ref> According to the Health Services Resources Administration's 2000 Survey of Nurses only six percent of nurses who graduated from nursing programs in the United States received their education at a Diploma School of Nursing.<ref name="HRSA">Health Resources and Service Administration. [https://drive.google.com/open?id=1AZtwzmPYp5WulkjaX9vqKZn_TxgcFM8E "Findings from the National Sample Survey Of Registered Nurses"] Washington, D.C., U.S. Department of Health and Human Services Health Resources and Service Administration Bureau of Health Professions Division of Nursing, 2000.</ref>
| |
| − | | |
| − | =====Associate Degree in Nursing=====
| |
| − | {{main article|Associate of Science in Nursing}}
| |
| − | The most common initial nursing education is a two-year [[Associate Degree in Nursing]] (Associate of Applied Science in Nursing, Associate of Science in Nursing, Associate Degree in Nursing), a [[community college|two-year college]] degree referred to as an ADN. Some four-year colleges and universities also offer the ADN. Associate degree nursing programs have prerequisite and corequisite courses (which may include English, Math and Human Anatomy and Physiology) and ultimately stretch out the degree-acquiring process to about three years or greater.
| |
| − | | |
| − | =====Bachelor of Science in Nursing=====
| |
| − | {{main article|Bachelor of Science in Nursing}}
| |
| − | The third method is to obtain a [[Bachelor of Science in Nursing]] (BSN), a four-year degree that also prepares nurses for graduate-level education. For the first two years in a BSN program, students usually obtain general education requirements and spend the remaining time in nursing courses. In some new programs the first two years can be substituted for an active LPN license along with the required general studies. Advocates for the ADN and diploma programs state that such programs have an on the job training approach to educating students, while the BSN is an [[academic degree]] that emphasizes research and [[nursing theory]]. Some states require a specific amount of clinical experience that is the same for both BSN and ADN students. A BSN degree qualifies its holder for administrative, research, consulting and teaching positions that would not usually be available to those with an ADN, but is not necessary for most patient care functions. Nursing schools may be accredited by either the [[Accreditation Commission for Education in Nursing]] (ACEN) or the [[Commission on Collegiate Nursing Education]] (CCNE).
| |
| − | | |
| − | =====Graduate education=====
| |
| − | {{Further information|Master of Science in Nursing|Doctor of Nursing Practice}}
| |
| − | | |
| − | Advanced education in nursing is done at the master's and doctoral levels. It prepares the graduate for specialization as an [[advanced practice registered nurse]] (APRN) or for advanced roles in leadership, management, or education. The [[clinical nurse leader]] (CNL) is an advanced generalist who focuses on the improvement of quality and safety outcomes for patients or patient populations from an administrative and staff management focus. Doctoral programs in nursing prepare the student for work in nursing education, health care administration, clinical research, public policy, or advanced clinical practice. Most programs confer the PhD in nursing or [[Doctor of Nursing Practice]] (DNP).
| |
| − | | |
| − | [[Advanced practice registered nurse]] (APRN)
| |
| − | | |
| − | Areas of advanced nursing practice include that of a [[nurse practitioner]] (NP), a certified [[nurse midwife]] (CNM), a [[nurse anesthetist|certified registered nurse anesthetist]] (CRNA), or a [[clinical nurse specialist]] (CNS). Nurse practitioners and CNSs work assessing, diagnosing and treating patients in fields as diverse as [[family practice]], women's health care, [[emergency nursing]], acute/critical care, [[psychiatry]], [[geriatrics]], or [[pediatrics]], additionally, a CNS usually works for a facility to improve patient care, do research, or as a staff educator.
| |
| − | | |
| − | ====Licensure examination====
| |
| − | | |
| − | Completion of any one of these three educational routes allows a graduate nurse to take the [[NCLEX-RN]], the test for [[nurse licensure|licensure]] as a registered nurse, and is accepted by every state as an adequate indicator of minimum competency for a new graduate. However, controversy exists over the appropriate entry-level preparation of RNs. Some professional organizations believe the BSN should be the sole method of RN preparation and ADN graduates should be licensed as "technical nurses" to work under the supervision of BSN graduates. Others feel the on-the-job experiences of diploma and ADN graduates makes up for any deficiency in theoretical preparation.
| |
| − | | |
| − | ====Shortage in the United States====
| |
| − | {{Main article|Nursing shortage}}
| |
| − | RNs are the largest group of health care workers in the United States, with about 2.7 million employed in 2011.<ref name="bls.gov">[http://www.bls.gov/oes/current/oes291111.htm Bureau of Labor Statistics – Registered Nurses] {{webarchive |url=https://web.archive.org/web/20120811044058/http://www.bls.gov/oes/current/oes291111.htm |date=11 August 2012 }}</ref> It has been reported{{By whom|date=July 2012}} that the number of new graduates and foreign-trained nurses is insufficient to meet the [[demand]] for registered nurses; this is often referred to as the [[nursing shortage]] and is expected{{By whom|date=July 2012}} to increase for the foreseeable future. There are data to support the idea that the nursing shortage is a voluntary shortage.{{Citation needed|date=July 2012}} In other words, nurses are leaving nursing of their own volition. In 2006 it was estimated that approximately 1.8 million nurses chose not to work as a nurse. The Bureau of Labor Statistics (BLS) reported that 296,900 healthcare jobs were created in 2011. RNs make up the majority of the healthcare work force, therefore these positions will be filled primarily by nurses. The BLS also states that by 2020, there will be 1.2 million nursing job openings due to an increase in the workforce, and replacements.<ref>Rosseter, 2012.</ref>
| |
| − | | |
| − | =====Causes=====
| |
| − | {{Crystal|section|date=July 2012}}
| |
| − | The International Council of Nursing (ICN), the largest international health professional organization in the world, recognizes the shortage of nurses as a growing crisis in the world. This shortage impacts the healthcare of everyone worldwide. One of the many reasons is that nurses who pursue to become nurses do so very late in their lives. This leads to a non-lengthy employment time. A national survey prepared by the Federation of Nurses and Health Professionals in 2001 found that one in five nurses plans to leave the profession within five years because of unsatisfactory working conditions, including low pay, severe under staffing, high stress, physical demands, mandatory overtime, and irregular hours. Approximately 29.8 percent of all nursing jobs are found in hospitals.<ref name="bls.gov"/> However, because of administrative cost cutting, increased nurse's workload, and rapid growth of outpatient services, hospital nursing jobs will experience slower than average growth. Employment in home care and nursing homes is expected{{By whom|date=July 2012}} to grow rapidly. Though more people are living well into their 80s and 90s, many need the kind of long-term care available at a nursing home. Many nurses will also be needed to help staff the growing number of out-patient facilities, such as HMOs (Health Maintenance Organizations), group medical practices, and ambulatory surgery centers. Nursing specialties will be in great demand. There are, in addition, many part-time employment possibilities.<ref name="isbn0-8160-6587-X">{{cite book |title=Nursing (Ferguson's Careers in Focus) |publisher=Ferguson |location=New York, N.Y. |year=2006 |page=[https://archive.org/details/careersinfocusnu0000unse_l8r2/page/188 188] |isbn=978-0-8160-6587-5 |url=https://archive.org/details/careersinfocusnu0000unse_l8r2/page/188 }}</ref><ref name="Nardi, Deena A. 2013">Nardi, Deena A., and Charlene C. Gyurko. "The Global Nursing Faculty Shortage: Status and Solutions for Change." (2013): 1–11. Web. 28 Jan. 2015.</ref>
| |
| − | | |
| − | Levsey, Campbell, and Green voiced their concern about the shortage of nurses, citing Fang, Wilsey-Wisniewski, & Bednash, 2006, who state that over 40,000 qualified nursing applicants were turned away in the 2005–2006 academic year from baccalaureate nursing programs due to a lack of masters and doctoral qualified faculty, and that this number was increased over 9,000 from 32,000 qualified but rejected students from just two years earlier. Several strategies have been offered to mitigate this shortage including; Federal and private support for experienced nurses to enhance their education, incorporating more hybrid/blended nursing courses, and using simulation in lieu of clinical (hospital) training experiences.<ref name="Nardi, Deena A. 2013"/><ref>{{cite journal | last1=Fang | first1=D. | last2=Wilsey-Wisniewski | first2=S.J. | last3=Bednash | first3=G.D. | year = 2006 | title = 2005–2006 enrollment and graduations in baccalaureate and graduate programs in nursing. Washington, DC: American Association of Colleges of Nursing. Levsey, K.R., Campbell, D., & Green, A. (2007). Yesterday, Today, and Tomorrow; Challenges in Securing Federal Support for Graduate Nurses | url = | journal = Journal of Nursing Education | volume = 46 | issue = 4| pages = 176–183 }}</ref>
| |
| − | | |
| − | Furthermore, there is a shortage of academically qualified instructors to teach at schools of nursing worldwide. The serious need for educational capacity is not being met, which is the underlying most important preparation resource for the nurses of tomorrow. The decrease in faculty everywhere is due to many factors including decrease in satisfaction with the workforce, poor salaries, and reduction in full-time equivalent. Throughout the span of 6 years the nursing faculty shortage has been written about an increasing amount. There is no clear consensus or an organized plan on how to fix the ongoing issue.<ref>Nardi, Deena A., and Charlene C. Gyurko. "The Global Nursing Faculty Shortage: Status and Solutions for Change." (2013): 1–11. Web. 28 Jan. 2015</ref>
| |
| − | | |
| − | ====Continuing education====
| |
| − | With health care knowledge growing steadily, nurses can stay ahead of the curve through continuing education. Continuing education classes and programs enable nurses to provide the best possible care to patients, advance nursing careers, and keep up with Board of Nursing requirements. The American Nurses Association and the American Nursing Credentialing Center are devoted to ensuring nurses have access to quality continuing education offerings. Continuing education classes are calibrated to provide enhanced learning for all levels of nurses. Many States also regulate Continuing Nursing Education. Nursing licensing boards requiring Continuing Nursing Education (CNE) as a condition for licensure, either initial or renewal, accept courses provided by organizations that are accredited by other state licensing boards, by the American Nursing Credentialing Center (ANCC), or by organizations that have been designated as an approver of continuing nursing education by ANCC.<ref>{{cite web|url=http://www.nursecredentialing.org/AccredContactHoursFAQ|title=FAQs: Contact Hours (CNE Credit)|publisher=}}</ref> There are some exceptions to this rule including the state of California, Florida and Kentucky. National Healthcare Institute<ref name="nhinstitute">{{cite web|url=http://www.nhinstitute.com|title=Continuing Education for Nurses and Medics|website=NHI|accessdate=2017-12-10}}</ref> has created a list to assist nurses in determining their CNE credit hours requirements. While this list is not all inclusive, it offers details on how to contact nursing licensing boards directly.<ref name="http://www.nursingworld.org/">{{cite web|url=http://www.nursingworld.org/ |title=American Nurses Association |publisher=Nursingworld.org |accessdate=2011-08-21}}</ref><ref name="http://www.NHInstitute.org/">{{cite web|url=http://www.nhinstitute.com/item/education-requirements-by-board-of-nursing.html|title=National Healthcare Institute Continuing Education Requirements by Board of Nursing |publisher=NHInstitute.com |accessdate=2012-02-14}}</ref>
| |
| − | | |
| − | ====Board certification====
| |
| − | {{main article|Nursing credentials and certifications}}
| |
| − | | |
| − | Professional nursing organizations, through their certification boards, have voluntary certification exams to demonstrate clinical competency in their particular specialty. Completion of the prerequisite work experience allows an RN to register for an examination, and passage gives an RN permission to use a professional designation after their name. For example, passage of the American Association of Critical-care Nurses specialty exam allows a nurse to use the initials 'CCRN' after his or her name. Other organizations and societies have similar procedures.
| |
| − | | |
| − | The [[American Nurses Credentialing Center]], the credentialing arm of the [[American Nurses Association]], is the largest nursing credentialing organization and administers more than 30 specialty examinations.<ref name="ANCC">American Nurses Credentialing Center. [http://www.ana.org/ancc/cert/index.html "ANCC Certification"] Washington, D.C., American Nurses Association, '''2006'''.</ref>
| |
| − | | |
| − | ===India===
| |
| − | The Nursing education is governed in [[India]] by the central body [[Indian Nursing Council]] and its norms are implemented through respective State Nursing council such as [[Kerala Nurses and Midwives Council]].
| |
| − | | |
| − | === Colombia ===
| |
| | | | |
| | ==Notes== | | ==Notes== |
| Line 404: |
Line 134: |
| | | | |
| | ==References== | | ==References== |
| − | *{{cite web |author=Rosseter, R. |date=6 August 2012 |title= Media Relations/ Nursing Shortage |publisher= American Association of Colleges of Nursing |url=http://www.aacn.nche.edu/media-relations/fact-sheets/nursing-shortage}} | + | *Alligood, Martha Raile. ''Nursing Theorists and Their Work''. Mosby, 2013. ISBN 978-0323091947 |
| − | | + | *Blais, Kathy, and Janice S. Hayes. ''Professional Nursing Practice: Concepts and Perspectives''. Pearson, 2015. ISBN 978-0133801316 |
| − | | + | * D'Antonio, Patricia. ''American Nursing: A History of Knowledge, Authority, and the Meaning of Work''. Johns Hopkins University Press, 2010. ISBN 978-0801895654 |
| − | * Advanced Practice and Leadership in Radiology Nursing. Springer Publishing. (2020). {{ISBN|978-3-030-32678-4}} | + | *de Bary, William Theodore. ''The Buddhist Tradition: In India, China and Japan''. Vintage, 1972. ISBN 978-0394716961 |
| − | *{{cite encyclopedia|isbn = 978-0826107503|title = Encyclopedia of Nursing Research|edition=3rd|editor-last1 = Fitzpatrick|editor-first1 = Joyce J.|editor-first2=Meredith |editor-last2=Kazer|date = 2011-08-24|last1 = Fitzpatrick|first1 = Joyce J.}} | + | *Dunphy, Lynne M., Jill E. Winland-Brown, Brian Oscar Porter, and Debera J. Thomas. ''Primary Care: Art and Science of Advanced Practice Nursing - An Interprofessional Approach''. F.A. Davis Company, 2019. ISBN 978-0803667181 |
| − | * {{cite journal|doi=10.1080/1362704X.2016.1203090|title=The Nurse's Uniform as Ethopoietic Fashion|journal=Fashion Theory|volume=21|issue=5|pages=523–552|year=2017|last1=Hardy|first1=Susan|last2=Corones|first2=Anthony}}
| + | *Ferngren, Gary B. ''Medicine and Health Care in Early Christianity''. Johns Hopkins University Press, 2016. ISBN 978-1421420066 |
| − | * Longe, Jacqueline, ed. ''Gale Encyclopedia of Nursing and Allied Health'' (6 vol. 2013) | + | *Henderson, Virginia. ''The Nature of Nursing''. National League for Nursing Press, 1991. ISBN 978-0887374944 |
| − | | + | *Kalisch, Philip A., and Beatrice J. Kalisch. ''American Nursing: A History''. LWW, 2003. ISBN 978-0781739696 |
| − | * Bullough, Vern L. and Bonnie Bullough. ''The Emergence of Modern Nursing'' (2nd ed. 1972) | + | *McFarland-Icky, Bronny Rebekah. ''Nurses in Nazi Germany''. Princeton University Press, 1999. 978-0691006659 |
| − | * D'Antonio, Patricia. ''American Nursing: A History of Knowledge, Authority, and the Meaning of Work'' (2010), 272pp. | + | *Masters, Kathleen. ''Role Development in Professional Nursing Practice''. Jones & Bartlett Learning, 2018. ISBN 978-1284152913 |
| − | * Dock, Lavinia Lloyd. ''A Short history of nursing from the earliest times to the present day'' (1920) [https://books.google.com/books?id=IqC09J62exQC full text online]; abbreviated version of her four volume ''A History of Nursing'' [https://books.google.com/books?id=uiJtAAAAMAAJ vol 3 online] | + | *Nightingale, Florence. ''Notes on Nursing: What It Is, and What It Is Not''. IndoEuropeanPublishing, 2019. ISBN 978-1644390887 |
| − | * Donahue, M. Patricia. ''Nursing, The Finest Art: An Illustrated History'' (3rd ed. 2010), includes over 400 illustrations; 416pp; [https://www.amazon.com/dp/032305305X/ excerpt and text search] | + | *O'Lynn, Chad E., and Russell E. Tranbarger (eds.). ''Men in Nursing: History, Challenges, and Opportunities''. Springer Publishing Company, 2006. ISBN 978-0826102218 |
| − | * Fairman, Julie and Joan E. Lynaugh. ''Critical Care Nursing: A History'' (2000) [https://www.amazon.com/Critical-Care-Nursing-History-Caregiving/dp/0812215362/ excerpt and text search] | + | *Quinn, Shawna M. ''Agnes Warner and the Nursing Sisters of the Great War''. Goose Lane Editions, 2010. ISBN 978-0864926333 |
| − | * Judd, Deborah. ''A History of American Nursing: Trends and Eras'' (2009) 272pp [https://www.amazon.com/dp/0763759511/ excerpt and text search] | + | *Roux, Gayle. ''Issues and Trends in Nursing: Essential Knowledge for Today and Tomorrow''. Jones & Bartlett Learning, 2008. ISBN 978-0763752255 |
| − | * Kalisch, Philip A., and Beatrice J. Kalisch. '' Advance of American Nursing'' (3rd ed 1995) ; 4th ed 2003 is titled, ''American Nursing: A History'' | + | *Sachedina, Abdulaziz. ''Islamic Biomedical Ethics: Principles and Application ''. Oxford University Press, 2009. ISBN 978-0195378504 |
| − | * Snodgrass, Mary Ellen. ''Historical Encyclopedia of Nursing'' (2004), 354pp; from ancient times to the present | + | *Williamson, Gordon. ''World War II German Women's Auxiliary Services''. Osprey Publishing, 2003. ISBN 978-1841764078 |
| | | | |
| | ==External links== | | ==External links== |
| | + | All links retrieved November 16, 2022. |
| | + | * [https://www.rcn.org.uk/ Royal College of Nursing (RCN)] |
| | + | * [https://www.icn.ch/ International Council of Nurses (ICN)] |
| | + | * [https://www.nursingworld.org/ana/ American Nurses Association (ANA)] |
| | + | * [https://www.registerednursing.org/nursing-careers/ Nursing Careers & Specialties for RNs] |
| | | | |
| − | * [http://library.uncg.edu/dp/wv/itemSearch.aspx?t=1&k=nurse UNCG Library Betty H. Carter Women Veterans Historical Project: Nurse]
| + | {{Health care}} |
| − | * {{Cite EB1911|wstitle=Nursing |short=x}}
| |
| − | | |
| − | {{Medicine}}
| |
| − | | |
| | | | |
| | + | [[Category:Health care]] |
| | [[Category:Medicine]] | | [[Category:Medicine]] |
| | {{Credits|Nursing|946154225}} | | {{Credits|Nursing|946154225}} |
"Nurse" redirects here.
| Nurse
|

A British nurse caring for a baby
|
| Occupation |
|---|
| Names | Nurse |
|---|
| Activity sectors | Nursing |
|---|
| Description |
|---|
| Competencies | Caring for general well-being of patients |
|---|
| Education required | Qualifications in terms of statutory regulations according to national, state, or provincial legislation in each country |
|---|
Fields of
employment |
|
|---|
| Related jobs |
Medicine |
|---|
Nursing is a profession within the health care sector focused on the care of individuals, families, and communities so they may attain, maintain, or recover optimal health and quality of life. Nurses may be differentiated from other health care providers by their approach to patient care, training, and scope of practice. Many nurses provide care within the ordering scope of physicians, and this traditional role has shaped the public image of nurses as care providers.
Nurses develop a plan of care, working collaboratively with physicians, therapists, the patient, the patient's family, and other team members that focuses on treating illness to improve quality of life. Nurses may help coordinate the patient care performed by other members of a multidisciplinary health care team such as therapists, medical practitioners, and dietitians. In some countries, including the United States and the United Kingdom, advanced practice nurses, such as clinical nurse specialists and nurse practitioners, diagnose health problems and prescribe medications and other therapies. Nurses fulfill a vital function in human society, providing health care both interdependently, such as with physicians, and independently as nursing professionals.
Definition
Although nursing practice varies both through its various specialties and countries, these nursing organizations offer the following definitions:
Nursing encompasses autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or well, and in all settings. Nursing includes the promotion of health, prevention of illness, and the care of ill, disabled and dying people. Advocacy, promotion of a safe environment, research, participation in shaping health policy and in patient and health systems management, and education are also key nursing roles. (International Council of Nurses)[1]
The use of clinical judgment in the provision of care to enable people to improve, maintain, or recover health, to cope with health problems, and to achieve the best possible quality of life, whatever their disease or disability, until death. (Royal College of Nursing)[2]
Nursing is the protection, promotion, and optimization of health and abilities; prevention of illness and injury; alleviation of suffering through the diagnosis and treatment of human responses; and advocacy in health care for individuals, families, communities, and populations. (American Nurses Association)[3]
The unique function of the nurse is to assist the individual, sick or well, in the performance of those activities contributing to health or its recovery (or to peaceful death) that he would perform unaided if he had the necessary strength, will or knowledge. (Virginia Avenel Henderson)[4]
History
Nursing historians face the challenge of determining whether care provided to the sick or injured in antiquity was nursing care.[5] In the fifth century B.C.E., for example, Hippocrates describes the giving of skilled care and observation of patients by "attendants," who could be considered as early nurses.[6]
Before the foundation of modern nursing, members of religious orders such as nuns and monks often provided nursing-like care. These are found, for example, in Christian,[7] Islamic[8] and Buddhist[9] traditions. These traditions were influential in the development of the ethos of modern nursing.
During the Reformation of the sixteenth century, Protestant reformers shut down the monasteries and convents, allowing a few hundred municipal hospices to remain in operation in northern Europe. Nursing care went to the inexperienced as traditional caretakers, rooted in the Roman Catholic Church, were removed from their positions. As a result, the nursing profession suffered a major setback for approximately 200 years.[10]
Nineteenth century

Russian Sisters of Mercy in the Crimea, 1854-1855
During the Crimean War the Grand Duchess Elena Pavlovna issued the call for women to join the Order of Exaltation of the Cross (Krestodvizhenskaya obshchina) for the year of service in the military hospitals. The first section of twenty-eight "sisters," headed by Aleksandra Petrovna Stakhovich, the Directress of the Order, went off to the Crimea early in November 1854.[11]

Florence Nightingale was an influential figure in the development of modern nursing. No uniform had been created when Nightingale was employed during the
Crimean War. Both the role of nursing and education were first defined by Nightingale.
Florence Nightingale laid the foundations of professional nursing after the Crimean War.[12] From 1870, having set up the first school of nursing connected to a continuously operating hospital and medical school, the Nightingale model of professional education spread widely in Europe and North America.[13] Often considered the first nurse theorist, Nightingale linked health with five environmental factors:(1) pure or fresh air, (2) pure water, (3) efficient drainage, (4) cleanliness, and (5) light, especially direct sun light. Deficiencies in these five factors resulted in lack of health or illness.[14] Nightingale was also a pioneer of the graphical presentation of statistical data.[15]
The following were also important in the development of the nursing profession in the nineteenth century:
- Agnes Jones, of Fahan, County Donegal, Ireland became the first trained Nursing Superintendent of Liverpool Workhouse Infirmary at Brownlow Hill in 1865, and established a nurse training regime there.[16]
- Linda Richards, who was the first professionally trained nurse in the US graduated in 1873 from the New England Hospital for Women and Children in Boston, established quality nursing schools in the United States and Japan. She served as the first president of the American Society of Superintendents of Training Schools in 1894, which was the first professional organization for nurses.[17]
- Clarissa Harlowe "Clara" Barton, a pioneer American teacher, patent clerk, nurse, and humanitarian, and the founder of the American Red Cross.[18]
- Saint Marianne Cope, a Sister of St. Francis who opened and operated some of the first general hospitals in the United States, instituting cleanliness standards which influenced the development of America's modern hospital system.[19]
- Agnes Hunt from Shropshire was the first orthopedic nurse and was pivotal in the emergence of the The Robert Jones and Agnes Hunt Orthopaedic Hospital in Oswestry, Shropshire, UK.[20]
Catholic orders such as Little Sisters of the Poor, Sisters of Mercy, Sisters of St. Mary, St. Francis Health Services, Inc., and Sisters of Charity built hospitals and provided nursing services during this period.
Twentieth century
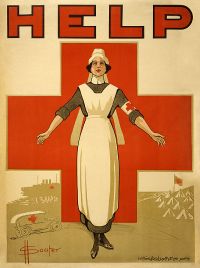
A recruiting poster for Australian nurses from
World War IHospital-based training came to the fore in the early 1900s, with an emphasis on practical experience. The Nightingale-style school began to disappear.
Many nurses saw active duty in World War I, but the profession was transformed during the Second World War. British nurses of the Army Nursing Service were part of every overseas campaign.[21] More nurses volunteered for service in the US Army and Navy than any other occupation.[22] The Nazis had their own Brown Nurses, 40,000 strong.[23] Two dozen German Red Cross nurses were awarded the Iron Cross for heroism under fire.[24]
Since the postwar period, nurse education has undergone a process of diversification towards advanced and specialized credentials, and many of the traditional regulations and provider roles have been changing.[25]

A nurse at Runwell Hospital, Wickford, Essex, in 1943
The modern era saw the development of undergraduate and post-graduate nursing degrees. Advancement of nursing research and a desire for association and organization led to the formation of a wide variety of professional organizations and academic journals in the field. Growing recognition of nursing as a distinct academic discipline was accompanied by an awareness of the need to define the theoretical basis for practice.[26]
In the nineteenth and early twentieth century, nursing was considered a women's profession, just as doctoring was a men's profession. With increasing expectations of workplace equality during the late twentieth century, nursing became an officially gender-neutral profession. In practice, however, the percentage of male nurses remained well below that of female physicians in the early twenty-first century.
As a profession
Nurses care for individuals of all ages and cultural backgrounds who are healthy and ill in a holistic manner based on the individual's physical, emotional, psychological, intellectual, social, and spiritual needs. The profession combines physical science, social science, nursing theory, and technology in caring for those individuals. The authority for the practice of nursing is based upon a social contract that delineates professional rights and responsibilities as well as mechanisms for public accountability. In almost all countries, nursing practice is defined and governed by law, and entrance to the profession is regulated at the national or state level.
The aim of the nursing community worldwide is for its professionals to ensure quality care for all, while maintaining their credentials, code of ethics, standards, and competencies, and continuing their education. There are a number of educational paths to becoming a professional nurse, which vary greatly worldwide; all involve extensive study of nursing theory and practice as well as training in clinical skills.
To work in the nursing profession, all nurses hold one or more credentials depending on their scope of practice and education. In the United States, a Licensed Practical Nurse (LPN) will work under the direction of a physician, mid-level practitioner, or Registered Nurse (RN). RNs provide scientific, psychological, and technological knowledge in the care of patients and families in many health care settings.
In the United States, multiple educational paths will qualify a candidate to sit for the licensing examination as an RN. The Associate Degree in Nursing (ADN) is awarded to the nurse who has completed a two-year undergraduate academic degree awarded by community colleges, junior colleges, technical colleges, and bachelor's degree-granting colleges and universities upon completion of a course of study usually lasting two years. The Bachelor of Science in Nursing (BSN) is awarded to the nurse who has earned an American four-year academic degree in the science and principles of nursing, granted by a tertiary education university or similarly accredited school. After completing either the LPN or either RN education programs in the United States, graduates are eligible to sit for a licensing examination to become a nurse, the passing of which is required for the nursing license.[27]
Scope of activities
RNs treat patients, record their medical history, provide emotional support, and provide follow-up care. Nurses also help doctors perform diagnostic tests, and may also assist doctors in the emergency room or in trauma care when help is needed.[28]
Activities of daily living assistance
Assisting in activities of daily living (ADL) are skills required in nursing as well as other professions such as nursing assistants. This includes assisting in patient mobility, such as moving an activity intolerant patient within bed. For hygiene, this often involves bed baths and assisting with urinary and bowel elimination.
Medication
All medications administered by nurses must be from a medication prescription from a licensed practitioner, such as a physician. Nurses do not have the authority to prescribe medications, although there are some exceptions. Nurses are legally responsible for the drugs they administer. There may be legal implications when there is an error in a prescription, and the nurse could be expected to have noted and reported the error. In the United States, nurses have the right to refuse any medication administration that they deem to be potentially harmful to the patient.[29]
In the United States, credentialed nurse practitioners (NP) can prescribe medication, including controlled substances. However, their degree of independence varies by state: In several states nurse practitioners have the explicit legal authority to prescribe; in others they must have a “collaborative relationship” or “protocol agreement” with a specific, supervising physician in order to prescribe medication.[30] A number of other countries around the world, including 13 European nations, allow qualified nurses to prescribe medication, some with full prescribing rights and others have restricted prescribing rights.[31]
Patient education
Patient education is the process by which health professionals and others impart information to patients and their caregivers that will alter their health behaviors or improve their health status. The patient's family is often involved in the education. Effective patient education leads to fewer complications and hospital visits.[29]
Specialties
Nursing is a very diverse health care profession. Nurses practice in a wide range of settings; some nurses follow the traditional role of working in a hospital setting while other work in more specialized settings such as private homes, schools, long-term care facilities, pharmaceutical companies, and as researchers in laboratories, universities, and research institutions.
Generally nursing is divided according to the needs of the patients. The major populations are:
- communities/public
- family/individual across the lifespan
- adult-gerontology
- pediatrics
- neonatal
- women's health/gender-related
- mental health
- informatics (eHealth)
- acute care hospitals
- ambulatory settings (physician offices, urgent care settings, camps, etc)
- school/college infirmaries
There are also specialist areas such as cardiac nursing, orthopedic nursing, palliative care, perioperative nursing, obstetrical nursing, oncology nursing, nursing informatics, telenursing, radiology, and emergency nursing.
Occupational hazards
The fast-paced and unpredictable nature of health care places nurses at risk for injuries and illnesses, including high occupational stress. Nurses consistently identify stress as a major work-related concern and have among the highest levels of occupational stress when compared to other professions. This stress is caused by the environment, psychosocial stressors, and the demands of nursing, including new technology that must be mastered, the emotional labor involved in nursing, physical labor, shift work, and high workload. This stress puts nurses at risk for short-term and long-term health problems, including sleep disorders, depression, mortality, psychiatric disorders, stress-related illnesses, and illness in general. Nurses are at risk of developing compassion fatigue and moral distress, which can worsen mental health. They also have very high rates of occupational burnout and emotional exhaustion, which increase the risk for illness, medical error, and suboptimal care provision.[32]
Nurses are also at risk for violence and abuse in the workplace.[33] Violence is typically perpetrated by non-staff (such as patients or family), whereas abuse is typically perpetrated by other hospital personnel.
Prevention
There are a number of interventions that can mitigate the occupational hazards of nursing. Individual-focused interventions include stress management programs, which can be customized to individuals, and which can reduce anxiety, sleep disorders, and other symptoms of stress. Physical supports, such as lumbar supports for the back, may also be used to reduce physical injury and alleviate pain.[34].[35] Organizational interventions focus on reducing stressful aspects of the work environment by defining stressful characteristics and developing solutions to them. Using organizational and individual interventions together is most effective at reducing stress on nurses.[32]
Shortage of nurses
Internationally, there is a serious shortage of nurses.[36] One reason for this shortage is due to the work environment in which nurses practice. In a recent review of the empirical human factors and ergonomic literature specific to nursing performance, nurses were found to work in generally poor environmental conditions. Some countries and states have passed legislation regarding acceptable nurse-to-patient ratios.
Notes
- ↑ Definition of Nursing ICN, 2002. Retrieved April 1, 2020.
- ↑ Helen Scott, RCN's definition of nursing: what makes nursing unique? British Journal of Nursing 11(21) (September 27, 2013). Retrieved April 1, 2020.
- ↑ Scope of practice defined in nursing ANA. Retrieved April 1, 2020.
- ↑ Angelo Gonzalo, Virginia Henderson: Nursing Need Theory Nurseslabs. Retrieved April 1, 2020.
- ↑ Chad E. O'Lynn and Russell E. Tranbarger (eds.), Men in Nursing: History, Challenges, and Opportunities (Springer Publishing Company, 2006, ISBN 978-0826102218).
- ↑ Edwin B. Levine and Myra E. Levine, Hippocrates, father of nursing, too? The American Journal of Nursing 65(12) (December 1965):86-88. Retrieved March 30, 2020.
- ↑ Gary B. Ferngren, Medicine and Health Care in Early Christianity (Johns Hopkins University Press, 2016, ISBN 978-1421420066).
- ↑ Abdulaziz Sachedina, Islamic Biomedical Ethics: Principles and Application (Oxford University Press, 2009, ISBN 978-0195378504).
- ↑ William Theodore de Bary, The Buddhist Tradition: In India, China and Japan (Vintage, 1972, ISBN 978-0394716961).
- ↑ Kathleen Masters, Role Development in Professional Nursing Practice (Jones & Bartlett Learning, 2018, ISBN 978-1284152913).
- ↑ John Shelton Curtiss, Russian Sisters of Mercy in the Crimea, 1854-1855 Slavic Review 25(1) (March 1966): 84-100.
- ↑ Warren Winkelstein, Jr., Florence Nightingale: Founder of Modern Nursing and Hospital Epidemiology Epidemiology 20(2) (March 2009): 311. Retrieved April 2, 2020.
- ↑ Shawna M. Quinn, Agnes Warner and the Nursing Sisters of the Great War (Goose Lane Editions, 2010, ISBN 978-0864926333).
- ↑ Kathy Blais and Janice S. Hayes, Professional Nursing Practice: Concepts and Perspectives (Pearson, 2015, ISBN 978-0133801316).
- ↑ Mark Bostridge, Florence Nightingale: the Lady with the Lamp| BBC, February 17, 2011. Retrieved April 2, 2020.
- ↑ Steven Horton, Agnes Jones Liverpool Hidden History, February 18, 2018. Retrieved April 2, 2020.
- ↑ Linda A.J. Richards 1841 - 1930 American Association for the History of Nursing. Retrieved April 2, 2020.
- ↑ Founder Clara Barton The American National Red Cross. Retrieved April 2, 2020.
- ↑ Jen Christensen, Mother Marianne becomes an American saint CNN, October 22, 2012. Retrieved April 2, 2020.
- ↑ Hospital History The Robert Jones and Agnes Hunt Orthopaedic Hospital.
- ↑ QA World War Two Nursing Qaranc. Retrieved April 2, 2020.
- ↑ Philip A. Kalisch and Beatrice J. Kalisch, American Nursing: A History (LWW, 2003, ISBN 978-0781739696).
- ↑ Bronny Rebekah McFarland-Icky, Nurses in Nazi Germany (Princeton University Press, 1999, 978-0691006659).
- ↑ Gordon Williamson, World War II German Women's Auxiliary Services (Osprey Publishing, 2003, ISBN 978-1841764078).
- ↑ Lynne M. Dunphy, Jill E. Winland-Brown, Brian Oscar Porter, and Debera J. Thomas, Primary Care: Art and Science of Advanced Practice Nursing - An Interprofessional Approach (F.A. Davis Company, 2019, ISBN 978-0803667181).
- ↑ Martha Raile Alligood, Nursing Theorists and Their Work (Mosby, 2013, ISBN 978-0323091947).
- ↑ Everything Nurses Need to Know About the NCLEX Licensing Exam. Retrieved April 2, 2020.
- ↑ Registered Nurse (RN) Career Profiles. Retrieved April 2, 2020.
- ↑ 29.0 29.1 Carol Taylor, Pamela Lynn, and Jennifer Bartlett, Fundamentals of Nursing: The Art and Science of Person-Centered Care (LWW, 2018, ISBN 978-1496362179).
- ↑ Can Nurse Practitioners Prescribe Medication? 'Nurse Practitioner Schools. Retrieved April 2, 2020.
- ↑ Claudia B. Maier, Nurse prescribing of medicines in 13 European countries Human Resources for Health 17 (2019). Retrieved April 2, 2020.
- ↑ 32.0 32.1 Rashaun Roberts, Paula L. Grubb, and James W. Grosch, Alleviating Job Stress in Nurses Medscape, June 25, 2012. Retrieved April 2, 2020.
- ↑ Dan Hartley and Marilyn Ridenour, Free On-line Violence Prevention Training for Nurses National Institute for Occupational Safety and Health, August 12, 2013. Retrieved April 2, 2020.
- ↑ Anna P. Dawson, Skye N. McLennan, Stefan D. Schiller, Gwendolen A. Jull, Paul W. Hodges, and Simon Stewart, Interventions to prevent back pain and back injury in nurses: a systematic review Occupational and Environmental Medicine, 64(10) (2007): 642–650. Retrieved April 2, 2020.
- ↑ Anna P. Dawson, Skye N. McLennan, Stefan D. Schiller, Gwendolen A. Jull, Paul W. Hodges, and Simon Stewart, Interventions to prevent back pain and back injury in nurses: a systematic review Occupational and Environmental Medicine, 64(10) (2007): 642–650. Retrieved April 2, 2020.
- ↑ James Buchan, Global nursing shortages BMJ 324(7340) (2002): 751–752. Retrieved April 2, 2020.
References
ISBN links support NWE through referral fees
- Alligood, Martha Raile. Nursing Theorists and Their Work. Mosby, 2013. ISBN 978-0323091947
- Blais, Kathy, and Janice S. Hayes. Professional Nursing Practice: Concepts and Perspectives. Pearson, 2015. ISBN 978-0133801316
- D'Antonio, Patricia. American Nursing: A History of Knowledge, Authority, and the Meaning of Work. Johns Hopkins University Press, 2010. ISBN 978-0801895654
- de Bary, William Theodore. The Buddhist Tradition: In India, China and Japan. Vintage, 1972. ISBN 978-0394716961
- Dunphy, Lynne M., Jill E. Winland-Brown, Brian Oscar Porter, and Debera J. Thomas. Primary Care: Art and Science of Advanced Practice Nursing - An Interprofessional Approach. F.A. Davis Company, 2019. ISBN 978-0803667181
- Ferngren, Gary B. Medicine and Health Care in Early Christianity. Johns Hopkins University Press, 2016. ISBN 978-1421420066
- Henderson, Virginia. The Nature of Nursing. National League for Nursing Press, 1991. ISBN 978-0887374944
- Kalisch, Philip A., and Beatrice J. Kalisch. American Nursing: A History. LWW, 2003. ISBN 978-0781739696
- McFarland-Icky, Bronny Rebekah. Nurses in Nazi Germany. Princeton University Press, 1999. 978-0691006659
- Masters, Kathleen. Role Development in Professional Nursing Practice. Jones & Bartlett Learning, 2018. ISBN 978-1284152913
- Nightingale, Florence. Notes on Nursing: What It Is, and What It Is Not. IndoEuropeanPublishing, 2019. ISBN 978-1644390887
- O'Lynn, Chad E., and Russell E. Tranbarger (eds.). Men in Nursing: History, Challenges, and Opportunities. Springer Publishing Company, 2006. ISBN 978-0826102218
- Quinn, Shawna M. Agnes Warner and the Nursing Sisters of the Great War. Goose Lane Editions, 2010. ISBN 978-0864926333
- Roux, Gayle. Issues and Trends in Nursing: Essential Knowledge for Today and Tomorrow. Jones & Bartlett Learning, 2008. ISBN 978-0763752255
- Sachedina, Abdulaziz. Islamic Biomedical Ethics: Principles and Application . Oxford University Press, 2009. ISBN 978-0195378504
- Williamson, Gordon. World War II German Women's Auxiliary Services. Osprey Publishing, 2003. ISBN 978-1841764078
External links
All links retrieved November 16, 2022.
| Health care |
|---|
| | General | | | | Professions | | | | Settings | Assisted living • Clinic • Hospital • Nursing home • Medical school • Pharmacy school | | | Care | Acute • Chronic • End-of-life • Hospice • Overutilization • Palliative • Primary • Self • Total | | | Skills / Training | Cultural competence • Diagnosis • Education • Universal precautions |
|
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article
in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.