Contact lens
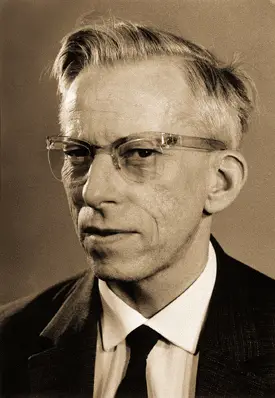
A contact lens (also known simply as a "contact") is a corrective, cosmetic, or therapeutic lens usually placed on the cornea of the eye. Modern contact lenses were invented by the Czech chemist Otto Wichterle, who also invented the first gel used for their production.
Contact lenses usually serve the same corrective purpose as conventional eyeglasses, but are lightweight and virtually invisible — many commercial lenses are tinted a faint blue to make them more visible when immersed in cleaning and storage solutions. Some cosmetic lenses are deliberately colored for altering the appearance of the eye.
People choose to wear contact lenses for various reasons. Many consider their appearance to be more attractive with contact lenses than with glasses. Contact lenses are less affected by wet weather, do not steam up, and provide a wider field of vision. They are more suitable for a number of sporting activities. Additionally, ophthalmological conditions such as keratoconus and aniseikonia may not be accurately corrected with glasses. On the other hand, excessive wear (especially overnight wear) can have adverse effects on the eyes.
History
Leonardo da Vinci is frequently credited with introducing the general principle of contact lenses in his 1508 Codex of the eye, Manual D, where he described a method of directly altering corneal power by submerging the eye in a bowl of water. Leonardo, however, did not suggest his idea be used for correcting vision—he was more interested in learning about the mechanisms of accommodation of the eye.
René Descartes proposed another idea in 1636, in which a glass tube filled with liquid is placed in direct contact with the cornea. The protruding end was to be composed of clear glass, shaped to correct vision; however the idea was unworkable, since it would make blinking impossible.
In 1801, while conducting experiments concerning the mechanisms of accommodation, scientist Thomas Young constructed a liquid-filled "eyecup" which could be considered a predecessor to the contact lens. On the eyecup's base, Young fitted a microscope eyepiece. However, like da Vinci's, Young's device was not intended to correct refraction errors.
In 1823, British astronomer Sir John Herschel suggesting making a mold of a person’s eyes as a way to produce corrective lenses.[1]
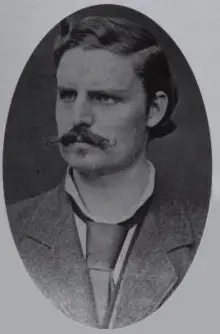
It was not until 1887 that the German physiologist Adolf Eugen Fick constructed and fitted the first successful contact lens. While working in Zürich, he described fabricating afocal scleral contact shells, which rested on the less sensitive rim of tissue around the cornea, and experimentally fitting them: initially on rabbits, then on himself, and lastly on a small group of volunteers. These lenses were made from heavy blown glass and were 18–21mm in diameter. Fick filled the empty space between cornea/callosity and glass with a grape sugar solution. He published his work, "Contactbrille," in the journal Archiv für Augenheilkunde in March 1888.
Fick's lens was large, unwieldy, and could only be worn for a few hours at a time. Glass-blown scleral lenses remained the only form of contact lens until the 1930s when polymethyl methacrylate (PMMA or Perspex/Plexiglas) was developed, allowing plastic scleral lenses to be manufactured for the first time.
In 1936 an optometrist, William Feinbloom introduced plastic lenses, making them lighter and more convenient.[2] These lenses were a combination of glass and plastic.
In the 1950s, the first "corneal" lenses were developed—these were much smaller than the original scleral lenses, as they sat only on the cornea rather than across all of the visible ocular surface. PMMA corneal lenses became the first contact lenses to have mass appeal through the 1960s, as lens designs became more sophisticated with improving manufacturing (lathe) technology.
One important disadvantage of PMMA lenses is that no oxygen is transmitted through the lens to the cornea, which can cause a number of adverse clinical effects. By the end of the 1970s, and through the 1980s and 1990s, a range of oxygen-permeable but rigid materials were developed to overcome this problem. Collectively, these polymers are referred to as "rigid gas permeable" or "RGP" materials or lenses. Although all the above lens types—sclerals, PMMA lenses and RGPs—could be correctly referred to as being "hard" or "rigid," the term hard is now used to refer to the original PMMA lenses which are still occasionally fitted and worn, whereas rigid is a generic term which can be used for all these lens types. That is, hard lenses (PMMA lenses) are a sub-set of rigid lenses. Occasionally, the term "gas permeable" is used to describe RGP lenses, but this is potentially misleading, as soft lenses are also gas permeable in that they allow oxygen to move through the lens to the ocular surface.
The principal breakthrough in soft lenses was made by the Czech chemist Otto Wichterle who published his work "Hydrophilic gels for biological use" in the journal Nature in 1959.[3] This led to the launch of the first soft (hydrogel) lenses in some countries in the 1960s and the first approval of the 'Soflens' material by the United States Food and Drug Administration (FDA) in 1971. These lenses were soon prescribed more often than rigid lenses, mainly due to the immediate comfort of soft lenses; by comparison, rigid lenses require a period of adaptation before full comfort is achieved. The polymers from which soft lenses are manufactured improved over the next 25 years, primarily in terms of increasing the oxygen permeability by varying the ingredients making up the polymers.
In 1999, an important development was the launch of the first silicone hydrogels onto the market. These new materials encapsulated the benefits of silicone — which has extremely high oxygen permeability — with the comfort and clinical performance of the conventional hydrogels that had been used for the previous 30 years. These lenses were initially advocated primarily for extended (overnight) wear although more recently, daily (no overnight) wear silicone hydrogels have been launched.
By the beginning of the twenty-first century about 125 million people used contact lenses worldwide (2 percent), including as many as 38 million in the United States[4] The numbers continue to increase, with the number worldwide reaching over 150 million by 2020.[5]
Types of contact lenses
Contact lenses are classified in various ways:
By function
Corrective contact lenses A corrective contact lens is a lens designed to improve vision. In many people, there is a mismatch between the refractive power of the eye and the length of the eye, leading to a refraction error. A contact lens neutralizes this mismatch and allows for correct focusing of light onto the retina. Conditions correctable with contact lenses include near (or short) sightedness (myopia), far (or long) sightedness (hypermetropia), astigmatism and presbyopia. Recently there has been renewed interest in orthokeratology, the correction of myopia by deliberate overnight flattening of the cornea, leaving the eye without contact lens or eyeglasses correction during the day. Contact wearers must usually take their contacts out every night or every few days, depending on the brand and style of the contact. However, many choose to leave these contacts in for longer periods of time than as prescribed. While this has no effect on the wearer in the short term, if the contact is left in for months at a time, eye infections and other eye problems have been reported, especially with old-fashioned "hard" contact lens models. A contact wearer may leave soft, daytime use contacts in for a week with no adverse affects, however.
For those with certain color deficiencies, a red-tinted "X-Chrom" contact lens may be used. Although the lens does not restore normal color vision, it allows some colorblind individuals to distinguish colors better.[6][7]
ChromaGen lenses have been used and these have been shown to have some limitations with vision at night although otherwise producing significant improvements in color vision.[8]
Later work that used these ChromaGen lenses with dyslexics in a randomized, double-blind, placebo controlled trial showed highly significant improvements in reading ability over reading without the lenses [9] This system has been granted FDA approval in the United States, which is reassuring to patients, and so its scientific approach has been correctly validated.
Cosmetic contact lenses - A cosmetic contact lens is designed to change the appearance of the eye. These lenses may also correct the vision, but some blurring or obstruction of vision may occur as a result of the color or design. In the United States, the FDA frequently calls non-corrective cosmetic contact lenses decorative contact lenses.[10]
Theatrical contact lenses are a type of cosmetic contact lens that are used primarily in the entertainment industry to make the eye appear pleasing, unusual or unnatural in appearance, most often in horror and zombie movies, where lenses can make one's eyes appear demonic, cloudy and lifeless, or even to make the pupils of the wearer appear dilated to simulate the natural appearance of the pupils under the influence of various illicit drugs.[11] These lenses have been used by Wes Borland, Richard Z. Kruspe, Val Kilmer, Marilyn Manson, Twiztid, World Wrestling Entertainment (WWE) wrestlers Kane, Rey Mysterio and Viscera, Ray Park as Darth Maul and Ian McDiarmid as Darth Sidious in Star Wars, Vin Diesel as Riddick in Pitch Black, and Dark Funeral vocalist Emperor Magus Caligula. Orlando Bloom wore blue cosmetic contact lenses for his role as the elf-prince Legolas Greenleaf in The Lord of the Rings trilogy. Recently, contact lenses using patterns of tomoe to simulate the Sharingan have become popular with fans of the anime Naruto.
Scleral lenses cover the white part of the eye (that is, sclera) and are used in many theatrical lenses. Due to their size, these lenses are difficult to insert and do not move very well within the eye. They may also hamper the vision as the lens has a small area for the user to see through. As a result they generally cannot be worn for more than 3 hours as they can cause temporary vision disturbances.
Similar lenses have more direct medical applications. For example, some lenses can give the iris an enlarged appearance, or mask defects such as absence (aniridia) or damage (dyscoria) to the iris.
Therapeutic contact lenses Soft lenses are often used in the treatment and management of non-refractive disorders of the eye. A bandage contact lens protects an injured or diseased cornea from the constant rubbing of blinking eyelids thereby allowing it to heal. They are used in the treatment of conditions including bullous keratopathy, dry eyes, corneal ulcers and erosion, keratitis, corneal edema, descemetocele, corneal ectasis, Mooren's ulcer, anterior corneal dystrophy, and neurotrophic keratoconjunctivitis. Contact lenses to deliver drugs to the eye have also been developed.[12]
By constructional material
The first contact lenses were made of glass, which caused eye irritation, and were not able to be worn for extended periods of time. But when William Feinbloom introduced lenses made from polymethyl methacrylate (PMMA or Perspex/Plexiglas), contacts became much more convenient. These PMMA lenses are commonly referred to as "hard" lenses (this term is not used for other types of contacts).
However, PMMA lenses have their own side effects: no oxygen is transmitted through the lens to the cornea, which can cause a number of adverse clinical events. In the late 1970s, and through the 1980s and 1990s, improved rigid materials — which were also oxygen-permeable — were developed. Collectively, these polymers are referred to as rigid gas permeable or 'RGP' materials or lenses.
Rigid lenses offer a number of unique properties. In effect, the lens is able to replace the natural shape of the cornea with a new refracting surface. This means that a regular (spherical) rigid contact lens can provide good level of vision in people who have astigmatism or distorted corneal shapes as with keratoconus.
While rigid lenses have been around for about 120 years, soft lenses are a much more recent development. The principal breakthrough in soft lenses made by Otto Wichterle led to the launch of the first soft (hydrogel) lenses in some countries in the 1960s and the approval of the 'Soflens' material (polymacon) by the United States FDA in 1971. Soft lenses are immediately comfortable, while rigid lenses require a period of adaptation before full comfort is achieved. The polymers from which soft lenses are manufactured improved over the next 25 years, primarily in terms of increasing the oxygen permeability by varying the ingredients making up the polymers.
A small number of hybrid rigid/soft lenses exist. An alternative technique is piggybacking of contact lenses, a smaller, rigid lens being mounted atop a larger, soft lens. This is done for a variety of clinical situations where a single lens will not provide the optical power, fitting characteristics, or comfort required.
In 1999, 'silicone hydrogels' became available. Silicone hydrogels have both the extremely high oxygen permeability of silicone and the comfort and clinical performance of the conventional hydrogels. These lenses were initially advocated primarily for extended (overnight) wear, although more recently daily (no overnight) wear silicone hydrogels have been launched.
While it provides the oxygen permeability, the silicone also makes the lens surface highly hydrophobic and less "wettable." This frequently results in discomfort and dryness during lens wear. In order to compensate for the hydrophobicity, hydrogels are added (hence the name "silicone hydrogels") to make the lenses more hydrophilic. However the lens surface may still remain hydrophobic. Hence some of the lenses undergo surface modification processes which cover the hydrophobic sites of silicone. Some other lens types incorporate internal rewetting agents to make the lens surface hydrophilic.
By wear time
A daily wear contact lens is designed to be removed prior to sleeping. An extended wear (EW) contact lens is designed for continuous overnight wear, typically for 6 or more consecutive nights. Newer materials, such as silicone hydrogels, allow for even longer wear periods of up to 30 consecutive nights; these longer-wear lenses are often referred to as continuous wear (CW). Generally, extended wear lenses are discarded after the specified length of time. These are increasing in popularity, due to their obvious convenience. Extended- and continuous-wear contact lenses can be worn for such long periods of time because of their high oxygen permeability (typically 5-6 times greater than conventional soft lenses), which allows the eye to remain remarkably healthy.
Extended lens wearers may have an increased risk for corneal infections and corneal ulcers, primarily due to poor care and cleaning of the lenses, tear film instability, and bacterial stagnation. Corneal neovascularization has historically also been a common complication of extended lens wear, though this does not appear to be a problem with silicone hydrogel extended wear. The most common complication of extended lens use is conjunctivitis, usually allergic or giant papillary conjunctivitis (GPC), sometimes associated with a poorly fitting contact lens.
By frequency of replacement
The various soft contact lenses available are often categorized by their replacement schedule. The shortest replacement schedule is single use (daily disposable) lenses, which are disposed of each night.[13] These may be best for patients with ocular allergies or other conditions, because it limits deposits of antigens and protein. Single use lenses are also useful for people who use contacts infrequently, or for purposes where losing a lens is likely (for instance, swimming) or not easily replaced (such as when on vacation). More commonly, contact lenses are prescribed to be disposed of on a two-week or monthly basis. Quarterly or annual lenses, which used to be very common, have lost favor because a more frequent disposal schedule allows for thinner lenses and limits deposits. Rigid gas permeable lenses are very durable and may last for several years without the need for replacement.
By design
A spherical contact lens is one in which both the inner and outer optical surfaces are portions of a sphere. A toric lens is one in which either or both of the optical surfaces have the effect of a cylindrical lens, usually in combination with the effect of a spherical lens. Myopic (nearsighted) and hypermetropic (farsighted) people who also have astigmatism and who have been told they are not suitable for regular contact lenses may be able to use toric lenses. If one eye has astigmatism and the other does not, the patient may be told to use a spherical lens in one eye and a toric lens in the other. Toric lenses are made from the same materials as regular contact lenses but have a few extra characteristics:
- They correct for both spherical and cylindrical aberration.
- They may have a specific 'top' and 'bottom', as they are not symmetrical around their centre and must not be rotated. Lenses must be designed to maintain their orientation regardless of eye movement. Often lenses are thicker at the bottom and this thicker zone is pushed down by the upper eyelid during blinking to allow the lens to rotate into the correct position (with this thicker zone at the 6 o'clock position on the eye). Toric lenses are usually marked with tiny striations to assist their fitting.
- They are usually more expensive to produce than non-toric lenses; as such, they are usually meant for extended wear and previous to 2000 when Vistakon introduced the first disposable Toric lenses, Toric lenses were not available in disposable forms.
Like eyeglasses, contact lenses can have one (single vision) or more (multifocal) focal points.
For correction of presbyopia or accommodative insufficiency multifocal contact lenses are almost always used; however, single vision lenses may also be used in a process known as monovision[14]: single vision lenses are used to correct one eye's far vision and the other eye's near vision. Alternatively, a person may wear single vision contact lenses to improve distance vision and reading glasses to improve near vision.
Multifocal contact lenses are more complex to manufacture and require more skill to fit. All soft bifocal contact lenses are considered "simultaneous vision" because both far and near vision are corrected simultaneously, regardless of the position of the eye. Commonly these are designed with distance correction in the center of the lens and near correction in the periphery, or viceversa. Rigid gas permeable contact lenses most commonly have a small lens on the bottom for the near correction: when the eyes are lowered to read, this lens comes into the optical path.
Implantation
Intraocular contact lenses, also known as an implantable contact lenses, are special small corrective lenses surgically implanted in the eye's posterior chamber behind the iris and in front of the lens to correct higher amounts of myopia and hyperopia.
Manufacture of contact lenses
Most contact lenses are mass produced.
- Spin-cast lenses: A spin cast lens is a soft contact lens manufactured by whirling liquid plastic in a revolving mold at high speed.[15]
- Lathe cut: A lathe cut contact lens is cut and ground on a lathe.[15]
Contact lens prescriptions
The prescription of contact lenses is usually restricted to appropriately qualified eye care practitioners. In countries such as the United States (where all contact lenses are deemed to be medical devices by the Food and Drug Administration), the United Kingdom and Australia, optometrists are usually responsible. In France and eastern European countries, ophthalmologists play the major role. In other parts of the world, opticians usually prescribe contact lenses. Prescriptions for contact lenses and glasses may be similar, but are not interchangeable.
The practitioner or contact lens fitter typically determines an individual's suitability for contact lenses during an eye examination. Corneal health is verified; ocular allergies or dry eyes may affect a person's ability to successfully wear contact lenses. Especially above the age of 35 years dry eyes often makes wearing contact lenses too risky, especially soft lenses.
The parameters specified in a contact lenses prescription may include:
- Material (such as Oxygen Permeability/Transmissibility (Dk/L, Dk/t), water content, modulus)
- Base curve radius (BC, BCR)
- Diameter (D, OAD)
- Power in dioptres - Spherical, Cylindrical and/or reading addition)
- Cylinder axis
- Center thickness (CT)
- Brand
Many people already wearing contact lenses order them over the Internet at their own risk. It is also possible to convert the power of a prescription for eyeglasses to the power of contact lenses, using the following formula:
- ,
where
- is the distance of the glasses to the eye and
- is the focal length of the contact lens or the glasses,
- is the lens power in diopters.
The Fairness to Contact Lens Consumers Act, which became law in February, 2004, was intended to ensure the availability of contact lens prescriptions to patients.[16] Under the law, consumers have a right to obtain a copy of their contact lens prescription, allowing them to fill that prescription at the business of their choice.
Complications
Complications due to contact lens wear affect roughly 6 percent of contact lens wearers each year.[17] Excessive wear of contact lenses, particularly overnight wear, is associated with most of the safety concerns.[18] Problems associated with contact lens wear may affect the eyelid, the conjunctiva, the various layers of the cornea, and even the tear film that covers the outer surface of the eye.[17]
Eyelid:
- Ptosis
Conjunctiva:
- Contact dermatitis
- Giant papillary conjunctivitis
- Superior limbic keratoconjunctivitis
Cornea:
- Corneal abrasion
- Corneal erosion
- Corneal ulcer
- Hypoxia
- Stroma
- Infection and keratitis
- Contact lens acute red eye (CLARE)
- Keratoconus
- Endothelium
Usage
Before touching the contact lens or one's eyes, it is important to thoroughly wash and rinse hands with a soap that does not contain moisturizers or allergens such as fragrances. The technique for removing or inserting a contact lens varies slightly depending upon whether the lens is soft or rigid.
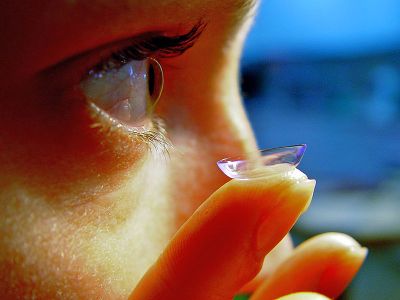
Insertion
Contact lenses are typically inserted into the eye by placing them on the index finger with the concave side upward and raising them to touch the cornea. The other hand may be employed to keep the eye open. Problems may arise particularly with disposable soft lenses; if the surface tension between the lens and the finger is too great the lens may turn itself inside out; alternatively it may fold itself in half. When the lens first contacts the eye, a brief period of irritation may ensue as the eye acclimates to the lens and also (if a multi-use lens is not correctly cleansed) as dirt on the lens irritates the eye. Irrigation may help during this period, which generally should not exceed one minute.
Removal
A soft lens may be removed by holding the eyelids open and grasping the lens with opposing digits. This method can cause irritation, could risk damage to the eye and may in many cases be difficult, in part due to the blink reflex. If the lens is pushed off the cornea it will buckle up (due to the difference in curvature), making it easier to grasp.
Rigid contact lenses may be removed by pulling with one finger on the outer or lateral canthus, then blinking to cause the lens to lose adhesion. The other hand is typically cupped underneath the eye to catch the lens. There also exist small tools specifically for removing lenses, which resemble small plungers made of flexible plastic; the concave end is raised to the eye and touched to the lens, forming a seal stronger than that of the lens with the cornea and allowing the lens to be removed from the eye.
Care (cleaning and disinfection)
While daily disposable lenses require no cleaning, other types require regular cleaning and disinfecting in order to retain clear vision and prevent discomfort and infections by various microorganisms including bacteria, fungi, and Acanthamoeba, that form a biofilm on the lens surface. There are a number of products that can be used to perform these tasks:
- Multipurpose solution - The most popular cleaning solution for contact lenses. Used for rinsing, disinfecting, cleaning and storing the lenses. Using this product eliminates the need for protein removal enzyme tablets in most cases. Multipurpose solutions are not effective at disinfecting Acanthamoeba from the lens.[19] In May 2007, one brand of multipurpose solution was recalled due to a cluster of Acanthamoeba infections.[20]
- Saline solution - Used for rinsing the lens after cleaning and preparing it for insertion. Saline solutions do not disinfect the lenses.
- Daily cleaner - Used to clean lenses on a daily basis. A few drops of cleaner are applied to the lens while it rests in the palm of the hand, then the lens is rubbed for about 20 seconds with a fingertip (check the cleaner's directions) on each side. Long fingernails can damage the lens, so care should be taken.
- Hydrogen peroxide solution - Used for disinfecting the lenses, and available as 'two-step' or 'one-step' systems. If using a 'two-step' product, one must ensure that the lens taken out of the hydrogen peroxide is neutralized before it is worn, or else wear will be extremely painful. Saline must not be used to rinse away the peroxide. Some peroxide solutions, such as CIBA Vision's Clear Care, come with a special storage case that contains a catalyzing disk. If soaked in the solution with the disk for at least six hours, the hydrogen peroxide decomposes and the remaining solution is a saline that will not harm the eye. People with extremely sensitive, irritable eyes often use these types of cleaning solutions. Peroxide solutions are the only commonly used disinfectant effective against Acanthamoeba, although the two-step solutions are more effective than the one-step, which neutralize too quickly to kill the amoeba's cysts.[21]
- Enzymatic cleaner - Used for cleaning protein deposits off lenses, usually weekly, if the daily cleaner is not sufficient. Typically, this cleaner is in tablet form. Protein deposits make use of contact lenses uncomfortable, and may lead to various eye problems.
Some products must only be used with certain types of contact lenses: it is important to check the product label to make sure that it can be used for a given type of lens. It is also important to follow the product's directions carefully to reduce risk of eye infection or eye irritation.
It is important to ensure that the product does not become contaminated with microorganisms: the tips of the containers for these solutions should never touch any surface, and the container should be kept closed when not in use. To counteract minor contamination of the product and kill microorganisms on the contact lens, some products may contain preservatives such as thimerosal, benzalkonium chloride, benzyl alcohol, and other compounds. In 1989, thimerosal was responsible for about ten percent of problems related to contact lenses[22]: because of this, many products no longer contain thimerosal. Preservative-free products usually have shorter shelf life. For example, non-aerosol preservative-free saline solutions can typically be used for only two weeks once opened. The introduction of silicone-hydrogel soft contact lens materials in 1999 made selection of the proper disinfecting solution more important. One study has noted several incompatibilities between these new lens materials and some solutions resulting in corneal staining.[23]
Notes
- ↑ The History of Contact Lenses Piedmont Eye Center, October 26, 2016. Retrieved July 16, 2022.
- ↑ Robert B. Mandell, Contact Lens Practice (Springfield, IL: Charles C. Thomas, 1988, ISBN 0398055092).
- ↑ O. Wichterle, D. Lim, Hydrophilic gels for biological use Nature 185(1960):117-118. Retrieved July 16, 2022.
- ↑ J. Barr, "2004 Annual Report". Contact Lens Spectrum (January 2005). Retrieved July 11, 2022.
- ↑ Rosalia Moreddu, D. Vigolo, and A. Yetisen, Contact Lens Technology: From Fundamentals to Applications Advanced Healthcare Materials 8 (2019). Retrieved July 11, 2022.
- ↑ NP Hartenbaum and CM Stack, Color vision deficiency and the X-Chrom lens Occup Health Saf. 66(9) (Sep 1997):36-40, 42. Retrieved July 16, 2022.
- ↑ I M Siegel, The X-Chrom lens. On seeing red Surv Ophthalmol. 25(5) (Mar-Apr 1981):312-324. Retrieved July 16, 2022.
- ↑ HA Swarbrick, P. Nguyen, T. Nguyen, P. Pham, The ChromaGen contact lens system: color vision test results and subjective responses Ophthalmic Physiol Opt. 21(3) (May 2001):182-196. Retrieved July 16, 2022.
- ↑ DA Harris and SJ MacRow-Hill, Application of ChromaGen haploscopic lenses to patients with dyslexia: a double masked placebo controlled trial Journal of the American Optometric Association 70(10) (Oct 1999):629-40. Retrieved July 16, 2022.
- ↑ 'Colored' and Decorative Contact Lenses: A Prescription Is A Must U.S. Food and Drug Administration, July 31, 2019. Retrieved July 16, 2022.
- ↑ Costume, Theatrical, Special Effects Contacts FX Contact Lenses. Retrieved July 16, 2022.
- ↑ Maria Fontanazza, Contact Lenses Employed for Drug Delivery R&D DIGEST, January 2005. Retrieved July 16, 2022.
- ↑ Liz Segre, Daily disposable contact lenses: pros and cons All About Vision. Retrieved July 16, 2022.
- ↑ KA Lebow and JB Goldberg, Characteristic of binocular vision found for presbyopic patients wearing single vision contact lenses Am Optom Assoc. 46(11) (Nov 1975) :1116-1123. Retrieved July 16, 2022.
- ↑ 15.0 15.1 B. Cassin and S. Solomon, Dictionary of Eye Terminology (Gainesville, FL: Triad Publishing Company, 1990, ISBN 0937404330).
- ↑ The Contact Lens Rule: A Guide for Prescribers and Sellers Federal Trade Commission, June 2020. Retrieved July 16, 2022.
- ↑ 17.0 17.1 John Stamler, The complications of contact lens wear Current Opinion in Ophthalmology 9(4) (August 1998): 66-71. Retrieved July 16, 2022.
- ↑ Dixie Farley, "Keeping an Eye on Contact Lenses: Safety, Options Shape Contact Lens Decisions." U.S. Food and Drug Administration: FDA Consumer. (March-April 1998), revised August 1998. Retrieved July 11, 2022.
- ↑ K. Hiti, J. Walochnik, E M Haller-Schober, C Faschinger, and H. Aspöck, Viability of Acanthamoeba after exposure to a multipurpose disinfecting contact lens solution and two hydrogen peroxide systems British Journal of Ophthalmology 86(2) (Feb 2002):144-146. Retrieved Juy 16, 2022.
- ↑ Acanthamoeba Keratitis --- Multiple States, 2005—2007 Center for Disease Control, May 26, 2007. Retrieved July 16, 2022.
- ↑ Reanne Hughes and Simon Kilvington, Comparison of Hydrogen Peroxide Contact Lens Disinfection Systems and Solutions against Acanthamoeba polyphaga Antimicrobial Agents and Chemotherapy 45(7) (July 2001): 50-57. Retrieved July 16, 2022.
- ↑ N. Wilson-Holt and JK Dart, Thiomersal keratoconjunctivitis, frequency, clinical spectrum and diagnosis Eye 3(Pt 5) (1989):581-587. Retrieved July 16, 2022.
- ↑ G. Andrasko and K. Ryen, A Series of Evaluations of MPS and Silicone Hydrogel Lens Combinations Review of Cornea & Contact Lenses (March 2007). Retrieved July 16, 2022.
ReferencesISBN links support NWE through referral fees
- Bennett, Edward S., and Barry A. Weissman. Clinical Contact Lens Practice. Philadelphia, PA: Lippincott Williams & Wilkins, 2004. ISBN 0781737052
- Cassin, B. and S. Solomon. Dictionary of Eye Terminology. Gainesville, FL: Triad Publishing Company, 1990. ISBN 0937404330
- Efron, Nathan. Contact Lens Practice. St. Louis, MO: Elsevier Health Sciences, 2002. ISBN 075064690X
- Gasson, Andrew, and Judith A. Morris. The Contact Lens Manual—A Practical Guide to Fitting. Boston, MA: Butterworth-Heinemann, 2003. ISBN 0750655488
- Heitz, R.F., and J. M. Enoch. Leonardo da Vinci: An assessment on his discourses on image formation in the eye. Advances in Diagnostic Visual Optics (1987): 19—26.
- Hom, Milton M., and Adrian S. Bruce. Manual of Contact Lens Prescribing and Fitting with CD-ROM, 3rd ed. Boston, MA: Butterworth-Heinemann, 2006. ISBN 0750675179
- Mandell, Robert B. Contact Lens Practice. Springfield, IL: Charles C. Thomas, 1988. ISBN 0398055092
External links
All links retrieved January 7, 2024.
- Consumer Guide to Contact Lenses (Articles).
- Contact Lens Facts And Statistics in 2022 Want Lens
- Contact Lenses Pasadena Eye Associates
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.