Bubonic plague
Bubonic plague, which is commonly referred to as plague, is a deadly infectious disease, which is caused by the bacterium Yersinia pestis. This bacterium, transmitted through the bite of a flea, has caused the death of millions of people.
The epidemiological use of the term "plague" is currently applied to bacterial infections that cause buboes, although historically the medical use of the term plague has been applied to pandemic infections generally. A bubo is a swelling of the lymph nodes. A pandemic is an epidemic (an outbreak of an infectious disease) that spreads across a large region, such as a continent, or even worldwide).
The plague is one of the most feared of all diseases. It is easily transmittable and has a high mortality. But today it can be cured through antibiotics, thanks in large measure to a few doctors and scientists who courageously risked their lives in experiments whose results have allowed countless other lives to be saved. On the other hand, while the creativity and courage of doctors and scientists have been essential to resolving the cause, transmission route, and cure of this dreaded disease, similar human capacities have likewise been applied in developing the use of this disease as a biological weapon. Such use of the plague traces at least to medieval Europe, when infected remains of animals and humans were used to contaminate enemy water supplies and plague victims were tossed into cities under siege. More recently, during the twentieth century, modern nations developed various means of weaponizing plague. During World War II, the Imperial Japanese Army not only developed weaponized plague, but deliberately infected Chinese civilians and prisoners of war to study the disease. (See Plague as a biological weapon.)
Infection/transportation
Plague is primarily a disease of rodents. Infection of human beings most often occurs when a person is bitten by an infected flea that has fed on an infected rodent. The bacteria multiply inside the flea, sticking together to form a plug that blocks its stomach and causes it to begin to starve. The flea then voraciously bites a host and continues to feed, even though it is unable to satisfy its hunger. During the feeding process, blood cannot flow into the blocked stomach, and consequently the flea vomits blood tainted with the bacteria back into the bite wound. The Bubonic plague bacterium then infects a new host, and the flea eventually dies from starvation. Any serious outbreak of plague is usually started as a result of other disease outbreaks in rodents, or some other crash in the rodent population. During these outbreaks, infected fleas that have lost their normal hosts seek other sources of blood.
In 1894, two bacteriologists, Alexandre Yersin and Shibasaburo Kitasato, independently isolated the bacterium in Hong Kong responsible for the Third Pandemic. Though both investigators reported their findings, a series of confusing and contradictory statements by Kitasato eventually led to the acceptance of Yersin as the primary discoverer of the organism. Yersin named it Pasteurella pestis in honor of the Pasteur Institute, where he worked. But in 1967, the genus was changed to Yersinia pestis, in honor of Yersin .
Yersin also reported that rats were affected by plague bacteria not only during epidemics, but that they were also often affected preceding epidemics in humans. Villagers in China and India noticed that when large numbers of rats were found dead, plague outbreaks in people soon followed.
In 1898, the French scientist Paul-Louis Simond, who had also come to China to battle the Third Pandemic, discovered the rat-flea vector relationship that drives the disease. He had noted that persons who became ill did not have to be in close contact with each other to acquire the disease. In Yunnan, China, inhabitants would flee from their homes as soon as they saw dead rats, and on the island of Formosa (Taiwan), residents considered handling dead rats a risk for developing plague. These observations led him to suspect that the flea might be an intermediary factor in the transmission of plague, since people acquired plague only if they were in contact with recently dead rats, but not affected if they touched rats that had been dead for more than 24 hours. In a now classic experiment, Simond demonstrated how a healthy rat died of plague after infected fleas had jumped to it from a plague-killed rat.
Clinical features
There are three forms of plague : (1) bubonic, (2) septicemic, and (3) pneumonic. Bubonic plague becomes evident three to eight days after the infection. Initial symptoms are chills, fever, diarrhea, headaches, and the swelling of the infected lymph nodes as the bacteria replicate there. If untreated, the rate of mortality for bubonic plague is 50-90 percent (Hoffman 1980).
In septicemic plague, there is bleeding into the skin and other organs, which creates black patches on the skin. There are bite-like bumps on the skin, commonly red and sometimes white in the center. Untreated septicemic plague is universally fatal, but early treatment with antibiotics reduces the mortality rate to between 4 and 15 percent (Wagle 1948; Meyer 1950; Datt Gupta 1948). People who die from this form of plague often die on the same day symptoms first appear.
The pneumonic plague infects the lungs, and with that infection comes the possibility of person-to-person transmission through respiratory droplets. The incubation period for pneumonic plague is usually between two and four days, but can be as little as a few hours. The initial symptoms, of headache, weakness, and coughing with hemoptysis, are indistinguishable from other respiratory illnesses. Without diagnosis and treatment, the infection can be fatal in one to six days; mortality in untreated cases may be as high as 95 percent.
Plague Bacteria
| Yersinia pestis | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
 | ||||||||||||
| Scientific classification | ||||||||||||
| ||||||||||||
| Yersinia pestis (Lehmann & Neumann, 1896) van Loghem 1944 |
There are 11 known species of Yersinia, but only three are considered pathogenic to human beings : (1) Y. pestis, the cause of plague, (2) Y. pseudotuberculosis, and (3) Y. enterocolitica, which is the most likely of these three to infect people.
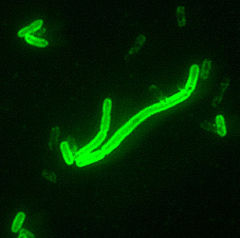
Yersinia pestis is a small gram-negative or bipolar-staining bacterium. They may appear as straight rods or coccobacilli. The bacteria have no flagella and are nonmotile. They contain two membranes.
Diagnosis
Organisms are best isolated from an infected bubo. Blood smears are usually negative for Y. pestis unless the patient is septicemic. However a series of blood samples taken 10-30 min apart has a greater chance of catching organisms released from lymph nodes into the blood. Sputum samples usually have too many other types of organisms to be useful (CDC 2007).
The plague bacilli are covered by a unique glycoprotein called the F1 antigen. This specific anitgen can be detected by a fluorescent antibody (FA) test. Plague bacilli can be broken open (lysed) by a specific bacteriophage at either 25 or 37 degrees Celsius.
The diagnosis of plague is confirmed if one of the following is observed:
- An isolated culture is lysed by a specific bacteriophage;
- Two samples of serum show a four fold anti-F1 antigen titer difference by aggultination testing;
- One sample of serum has a titer greater than 1:128 by agglutination;
and the patient has no previous history of plague antigen (CDC 2007).
Treatment
An Indian doctor, Vladimir Havkin, was the first to invent and test a plague antibiotic.
The traditional treatments are:
- Streptomycin 30 mg/kg intramuscular twice daily for 7 days
- Chloramphenicol 25â30 mg/kg single dose, followed by 12.5â15 mg/kg four times daily
- Tetracycline 2 g single dose, followed by 500 mg four times daily for 7â10 days (not suitable for children)
More recently,
- Gentamicin 2.5 mg/kg intravenous or intramuscular twice daily for 7 days
- Doxycycline 100 mg (adults) or 2.2 mg/kg (children) orally twice daily have also been shown to be effective (Mwengee 2006).
History
The earliest (though unvalidated) account describing a possible plague epidemic is found in I Samuel 5:6 of the Hebrew Bible (Torah). In this account, the Philistines of Ashdod were stricken with a plague for the crime of stealing the Ark of the Covenant from the Children of Israel. These events have been dated to approximately the second half of the eleventh century B.C.E. The word "tumors" is used in most English translations to describe the sores that came upon the Philistines. The Hebrew, however, can be interpreted as "swelling in the secret parts." The account indicates that the Philistine city and its political territory were stricken with a "ravaging of mice" and a plague, bringing death to a large segment of the population.
In the second year of the Peloponnesian War (430 B.C.E.), Thucydides described an epidemic disease that was said to have begun in Ethiopia, pass through Egypt and Libya, then come to the Greek world. In the Plague of Athens, the city lost possibly one third of its population, including Pericles. Modern historians disagree on whether the plague was a critical factor in the loss of the war. This epidemic has long been considered an outbreak of plague; however, because of Thucydides' description, modern scholars dispute that it was indeed plague. Many modern scholars feel that typhus, smallpox, or measles may better fit the descriptions. A recent study of the DNA found in the dental pulp of plague victims suggests that typhoid was actually responsible. Other scientists dispute these findings, citing serious methodologic flaws in the DNA study.
In the first century C.E., Rufus of Ephesus, a Greek anatomist, refers to an outbreak of plague in Libya, Egypt, and Syria. He records that Alexandrian doctors named Dioscorides and Posidonius described symptoms including acute fever, pain, agitation, and delirium. Buboesâlarge, hard, and non-suppuratingâdeveloped behind the knees, around the elbows, and "in the usual places." The death toll of those infected was very high. Rufus also wrote that similar buboes were reported by a Dionysius Curtus, who may have practiced medicine in Alexandria in the third century B.C.E. If this is correct, the eastern Mediterranean world may have been familiar with bubonic plague at that early date (Simpson 1905; Patrick 1967)
Plague of Justinian
The Plague of Justinian in 541â542 C.E.is the first known pandemic on record and marks the first firmly recorded pattern of bubonic plague. This outbreak is thought to have originated in Ethiopia or Egypt. The huge city of Constantinople imported massive amounts of grain, mostly from Egypt, to feed its citizens. The grain ships may have been the source of contagion for the city, with massive public granaries nurturing the rat and flea population. At its peak, the plague was killing 10,000 people in Constantinople every day and ultimately destroyed perhaps 40 percent of the city's inhabitants. It went on to destroy up to a quarter of the human population of the eastern Mediterranean.
In 588 C.E., a second major wave of plague spread through the Mediterranean into what is now France. A maximum of 25 million dead is considered a reasonable estimate. An outbreak of it in the 560s C.E. was described in 790 C.E. as causing "swellings in the glandsâŚin the manner of a nut or date" in the groin "and in other rather delicate places followed by an unbearable fever." While the swellings in this description have been identified by some as buboes, there is some contention as to whether the pandemic should be attributed to the bubonic plague organism, Yersinia pestis.
Black Death
During the mid-fourteenth century, from about 1347 to 1350, the Black Death, a massive and deadly pandemic, swept through Eurasia, killing approximately one third of the population (according to some estimates) and changing the course of Asian and European history. It is estimated that anywhere from a quarter to two-thirds of Europe's population became victims to the plague, making the Black Death the largest death toll from any known non-viral epidemic. While accurate statistical data do not exist, it is estimated that 1/4 of England's population (4.2 million) died. A higher percentage of individuals is likely to have died in Italy. On the other hand, northeastern Germany, Bohemia, Poland, and Hungary are believed to have suffered less, with no estimates for Russia or the Balkans.
In many European cities and countries, the presence of Jews was blamed for the arrival of the plague, and they were killed in pogroms or expelled.
The Black Death continued to strike parts of Europe throughout the fourteenth, fifteenth, and sixteenth centuries with intensity and fatality decreasing with time, strongly suggesting rising resistance.
Some have argued that changes in hygiene habits and strong efforts within the public health and sanitation sectors had a significant impact on the rate of infection. Also, medical practices of the time were based largely on spiritual and astrological factors, but towards the end of the plague, doctors took a more scientific approach to helping patients.
Was the Black Death viral?
In the early twentieth century, following the identification by Yersin and Kitasato of the plague bacterium that caused the late nineteenth and early twentieth century Asian bubonic plague (the Third Pandemic), most scientists and historians came to believe that the Black Death was an incidence of this plague, with a strong presence of the more contagious pneumonic and septicemic varieties increasing the pace of infection, spreading the disease deep into inland areas of the continents. It was claimed that the disease was spread mainly by black rats in Asia and that therefore there must have been black rats in northwest Europe at the time of the Black Death to spread it, although black rats are currently rare, except near the Mediterranean. This led to the development of a theory that brown rats had invaded Europe, largely wiping out black rats, bringing the plagues to an end, although there is no evidence for this theory in historical records. The view that the Black Death was caused by Yersinia pestis has been incorporated into medical textbooks throughout the twentieth century and has become part of popular culture, as illustrated by recent books (Kelly 2005).
Many modern researchers have argued that the disease was more likely to have been viral (that is, not bubonic plague), pointing to the absence of rats from some parts of Europe that were badly affected and to the conviction of people at the time that the disease was spread by direct human contact. According to the accounts of the time, the black death was extremely virulent, unlike the nineteenth and early twentieth century bubonic plague. The bubonic plague theory has been comprehensively rebutted by Samuel K. Cohn (2003A). He points to five major weaknesses in this theory (Cohn 2003B):
- Very different transmission speedsâthe Black Death was reported to have spread 385km in 91 days in 664, compared to 12-15 km a year for the modern bubonic plague, with the assistance of trains and cars;
- Difficulties with the attempt to explain the rapid spread of the Black Death by arguing that it was spread by the rare pneumonic form of the diseaseâin fact this form killed less than 0.3 percent of the infected population in its worst outbreak (Manchuria in 1911);
- Different seasonalityâthe modern plague can only be sustained at temperatures between 50 and 78 degrees F and requires high humidity, while the Black Death occurred even in Norway in the middle of the winter and in the Mediterranean in the middle of hot dry summers;
- Very different death ratesâin several places (including Florence in 1348) over 75 percent of the population appears to have died; in contrast, the highest mortality for the modern Bubonic Plague was 3 percent in Bombay (now known as Mumbai) in 1903
- The cycles and trends of infection were very different between the diseasesâhumans did not develop resistance to the modern disease, but resistance to the Black Death rose sharply, so that eventually it became mainly a childhood disease.
Cohn also points out that while the identification of the disease as having buboes relies on accounts of Boccaccio and others, they described buboes, abscesses, rashes, and carbuncles occurring all over the body, mostly concentrated around the neck or behind the ears. In contrast, the modern disease rarely has more than one bubo, most commonly in the groin, and is not characterized by abscesses, rashes, and carbuncles.
Third Pandemic
The Third Pandemic began in China in 1855, spreading plague to all inhabited continents and ultimately killing more than 12 million people in India and China alone. Casualty patterns indicate that waves of this pandemic may have come from two different sources. The first was primarily bubonic and was carried around the world through ocean-going trade, transporting infected persons, rats, and cargoes harboring fleas. The second, more virulent strain was primarily pneumonic in character, with a strong person-to-person contagion. This strain was largely confined to Manchuria and Mongolia. Researchers during the "Third Pandemic" identified plague vectors and the plague bacterium, leading, in time, to modern treatment methods.
The last significant European outbreak of plague occurred in Russia in 1877â1889 C.E. in rural areas near the Ural Mountains and the Caspian Sea. Efforts in hygiene and patient isolation reduced the spread of the disease, with approximately 420 deaths in the region. Significantly, the region of Vetlianka is near a population of the bobak marmot, a small rodent, which may be a very dangerous plague reservoir.
The bubonic plague continued to circulate through different ports globally for the next 50 years. However, it was primarily found in Southeast Asia. An epidemic in Hong Kong in 1894 had particularly high death rates, greater than 75 percent. As late as 1897, medical authorities in the European powers organized a conference in Venice, seeking ways to keep the plague out of Europe. The disease reached the Republic of Hawaii in December of 1899, and in an unprecedented catastrophe, the Board of Health of Hawaii burned down all of Honoluluâs Chinatown on January 20, 1900. Plague finally reached the United States later that year, in San Francisco.
Although the outbreak that began in China in 1855 is conventionally known as the Third Pandemicâthe First being the Plague of Justinian and the second being the Black Deathâit is unclear whether there have been fewer, or more, than three major outbreaks of bubonic plague. Most modern outbreaks of bubonic plague among humans have been preceded by a striking, high mortality among rats, yet this phenomenon is absent from descriptions of some earlier plagues, especially the Black Death. The buboes, or swellings of lymph nodes in the groin, that are especially characteristic of plague, are also a feature of other diseases such as syphilis and gonorrhea.
Plague as a biological weapon
Plague has a long history as a biological weapon. Historical accounts from medieval Europe detail the use of infected animal carcasses of cattle, horses, and human beings, by Mongols, Turks, and other groups, to contaminate enemy water supplies. Plague victims were also reported to have been tossed by catapult into cities under siege.
During World War II, the Imperial Japanese Army developed weaponized plague, based on the breeding and release of large numbers of fleas. During the Japanese occupation of Manchuria, Unit 731 deliberately infected Chinese civilians and prisoners of war with plague bacteria. These subjects, called "logs," were then studied by dissection, or vivisection while still conscious. Kirby (2005), who notes that "plague fleas have a rich military heritage as vectors of disease," records an effort by Japan to use a weapon of plague fleas against the United States in the Pacific theater in 1944, which apparently was foiled by the sinking of a submarine. Fortunately, after considering to use such weapons of devastating destructiveness against the continental United States, the Chief of Staff of the Imperial Japanese Army canceled the mission in March of 1945, considering it to be ethically unacceptable (Kirby 2005). Germany and the USSR investigated means of using fleas to transmit bubonic plague beginning in the 1930s, and the United States after the Korean War (Kirby 2005).
After World War II, both the United States and the Soviet Union developed diverse means of weaponizing pneumonic plague. Experiments included various delivery methods, vacuum drying, sizing the bacteria, developing strains resistant to antibiotics, combining the bacteria with other diseases (such as diphtheria), and genetic engineering. Scientists who worked in USSR bio-weapons programs have stated that the Soviet effort was formidable and that large stocks of weaponized plague bacteria were produced. Information on many of the Soviet projects is largely unavailable. Aerosolized pneumonic plague remains the most significant threat.
Contemporary cases
Two species of non-plague Yersinia, Yersinia pseudotuberculosis and Yersinia enterocolitica, still exist in fruit and vegetables from the Caucasus Mountains east across southern and central Russia, to Kazakhstan, Mongolia, and parts of China; in Southwest and Southeast Asia, Southern Africa and East Africa (including the island of Madagascar); in North America, from the Pacific ocean eastward to the western Great Plains, and from British Columbia south to Mexico; and in South America in two areas: The Andes mountains and Brazil.
There is no plague-infected animal population in Europe or Australia. Worldwide there are about 1,000 to 2,000 cases of human infection by plague each year.
The last plague epidemic involving rats in the United States occurred in Los Angeles in 1924-25. In the 1980s there were about 18 cases of plague per year with most of the victims being less than 20 years old.
- It was reported in September 2005 (ABC NEWS) that three mice infected with Yersinia pestis apparently disappeared from a laboratory belonging to the Public Health Research Institute,
- On 19 April, 2006, CNN News and others reported a case of plague in Los Angeles, California, the first reported case in that city since 1984.
- In May 2005, KSL Newsradio reported a case of plague found in dead field mice and chipmunks at Natural Bridges about 40 miles west of Blanding in San Juan County, Utah.
- In June 2006, the Arizona Central reported an article from the Associated Press of a case of plague found in a cat.
- In the U.S., about half of all food cases of plague since 1970 have occurred in New Mexico. There were 6 plague deaths in the state in 2006, the first fatalities in 12 years.
- The British Broadcast Corporation (BBC) reported that one hundred deaths resulting from pneumonic plague were reported in Ituri district of the eastern Democratic Republic of the Congo in June 2006. Control of the plague was proving difficult due to the Ituri conflict.
ReferencesISBN links support NWE through referral fees
- ABC News. 2005. Plague-infected mice missing From N.J. lab. ABC News September 15, 2005. Retrieved May 8, 2007.
- Arizona Central. 2006. Cat tests positive for bubonic plague. Arizona Central June 28, 2006. Retrieved May 8, 2007.
- BBC News. 2006. DR Congo 'Plague' leaves 100 dead. BBC News June 14, 2006. Retrieved December 15, 2006.
- Centers for Disease Control (CDC). 2005. Plague. Centers for Disease Control. Retrieved April 14, 2007.
- Cohn, S. K. 2003A. The Black Death Transformed: Disease and Culture in Early Renaissance Europe. A Hodder Arnold. ISBN 0340706465
- Cohn, S. K. 2003B. Black Death. In Encyclopedia of Population 1:98-101.101. Macmillan Publishers. ISBN 0028656776
- Datt Gupta, A. K. 1948. A short note on plague cases treated at Campbell Hospital. Ind Med Gaz 83: 150â151.
- Hoffman, S. L. 1980. Plague in the United States: The "Black Death" is still alive. Annals of Emergency Medicine 9: 319â22.
- Kelly, J. 2005. The Great Mortality: An Intimate History of the Black Death, the Most Devastating Plague of All Time. New York: HarperCollins Publishers Inc. ISBN 0060006927
- Kirby, R. 2005. Using the flea as weapon. Army Chemical Review July-December (2005): 30-35.
- KSL News ,Campground Closes Because of Plague. 2006.http://www.ksl.com/?nid=148&sid=265470
- Meyer,K.F. 1950. Modern therapy of plague. J Am Med Assoc 144: 982â985.
- Mwengee, W. et al. 2006. Treatment of plague with genamicin or doxycycline in a randomized clinical trial in Tanzania. Clin. Infect. Dis. 42(5): 614â21.
- New Mexico Department of Health, Albuquerque Environmental Health Department. 2006. Department of Health confirms sixth human plague case. Fifth case from Torrance County dies. New Mexico Department of Health July 25, 2006. Retrieved May 8, 2007.
- Patrick, A. 1967. Disease in antiquity: Ancient Greece and Rome. In D. Brothwell and A. t. Sandison, eds., Diseases in Antiquity. Springfield, Illinois.
- Simpson, W. J. 1905.A Treatise on Plague. Cambridge, England: Cambridge University Press.
- Wagle, P. M. 1948. Recent advances in the treatment of bubonic plague. Indian J Med Sci 2: 489â94.
Bibliography
- Biraben, J.-N. 1975. Les Hommes et la Peste The Hague.
- Buckler, J., B. D. Hill, and J. P. McKay. 1995. A History of Western Society, 5th Edition. New York: Houghton Mifflin Co. ISBN 0395708419
- Cantor, N. F. 2001. In the Wake of the Plague: The Black death and the World It Made New York: Harper. ISBN 0684857359
- de Carvalho, R. W., N. M. Serra-Freire, P. M. Linardi, A. B. de Almeida, and J. N. da Costa. 2001. Small rodents fleas from the bubonic plague focus located in the Serra dos ĂrgĂŁos Mountain Range, State of Rio de Janeiro, Brazil. MemĂłrias do Instituto Oswaldo Cruz 96(5): 603â609. Retrieved March 2, 2005.
- Gregg, C. T. 1978. Plague!: The Shocking Story of a Dread Disease in America Today. New York, NY: Scribner. ISBN 0684153726
- McNeill, W. H. 1976. Plagues and People. New York: Anchor Books. ISBN 0385121229
- Mohr, J. C. 2005. Plague and Fire: Battling Black Death and the 1900 Burning of Honolulu's Chinatown. New York, NY: Oxford University Press. ISBN 0195162315
- Orent, W. 2004. Plague: The Mysterious Past and Terrifying Future of the World's Most Dangerous Disease. New York: Free Press. ISBN 0743236858
- Platt, C. 1996. King Death: The Black Death and its Aftermath in Late-Medieval England Toronto University Press. ISBN 0802009301
- Spielvogel, J. J. 1999. Western Civilization: A Brief History Vol. 1: to 1715. Belmont, Calif.: West/Wadsworth, Ch. 3, p. 56, paragraph 2. ISBN 0534560628
External links
All links retrieved November 22, 2023.
- World Health Organization
- Plague Centers for Disease Control and Prevention
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.


