Difference between revisions of "Anxiety disorder" - New World Encyclopedia
(→Types) |
|||
| Line 37: | Line 37: | ||
[[Anxiety]] is an [[emotion]] which is characterized by an unpleasant state of inner [[turmoil]] and includes feelings of dread over [[Anticipation|anticipated]] events.<ref>Gerald C. Davison, Kirk R. Blankstein, Gordon L. Flett, and John M. Neale, ''Abnormal Psychology'' (Wiley, 2008, ISBN 978-0470840726).</ref><ref>Maria Miceli and Cristiano Castelfranchi, ''Expectancy and Emotion'' (Oxford University Press, 2015, ISBN 978-0199685868).</ref> It is a feeling of uneasiness and [[worry]], usually generalized and unfocused as an [[overreaction]] to a situation that is only subjectively seen as menacing.<ref> Colin Hemmings and Nick Bouras (eds.), ''Psychiatric and Behavioral Disorders in Intellectual and Developmental Disabilities'' (Cambridge University Press, 2016, ISBN 978-1107645943).</ref> Anxiety is often accompanied by nervous behavior such as pacing back and forth, [[somatic anxiety]], and [[Rumination (psychology)|rumination]],<ref>Martin E. P. Seligman, Elaine F. Walker, and David L. Rosenhan, ''Abnormal psychology'' (W. W. Norton & Company, 2001, ISBN 978-0393944594).</ref> People facing anxiety may withdraw from situations which have provoked anxiety in the past.<ref>Mary Chambers (ed.), ''Psychiatric and Mental Health Nursing: The craft of caring'' (Routledge, 2017, ISBN 1482221950).</ref> | [[Anxiety]] is an [[emotion]] which is characterized by an unpleasant state of inner [[turmoil]] and includes feelings of dread over [[Anticipation|anticipated]] events.<ref>Gerald C. Davison, Kirk R. Blankstein, Gordon L. Flett, and John M. Neale, ''Abnormal Psychology'' (Wiley, 2008, ISBN 978-0470840726).</ref><ref>Maria Miceli and Cristiano Castelfranchi, ''Expectancy and Emotion'' (Oxford University Press, 2015, ISBN 978-0199685868).</ref> It is a feeling of uneasiness and [[worry]], usually generalized and unfocused as an [[overreaction]] to a situation that is only subjectively seen as menacing.<ref> Colin Hemmings and Nick Bouras (eds.), ''Psychiatric and Behavioral Disorders in Intellectual and Developmental Disabilities'' (Cambridge University Press, 2016, ISBN 978-1107645943).</ref> Anxiety is often accompanied by nervous behavior such as pacing back and forth, [[somatic anxiety]], and [[Rumination (psychology)|rumination]],<ref>Martin E. P. Seligman, Elaine F. Walker, and David L. Rosenhan, ''Abnormal psychology'' (W. W. Norton & Company, 2001, ISBN 978-0393944594).</ref> People facing anxiety may withdraw from situations which have provoked anxiety in the past.<ref>Mary Chambers (ed.), ''Psychiatric and Mental Health Nursing: The craft of caring'' (Routledge, 2017, ISBN 1482221950).</ref> | ||
| − | Experiencing occasional anxiety is a normal part of life | + | Experiencing occasional anxiety is a normal part of life: "Anxiety is an adaptive response that promotes harm avoidance, but at the same time excessive anxiety constitutes the most common psychiatric complaint."<ref>Oliver J. Robinson, Alexandra C. Pike, Brian Cornwell, and Christian Grillon, [https://pubmed.ncbi.nlm.nih.gov/31256001/ The translational neural circuitry of anxiety] ''Journal of Neurology, Neurosurgery, and Psychiatry'' 90(12) (2019): 1353-1360. Retrieved November 17, 2022.</ref> However, people with anxiety disorders frequently have intense, excessive, and persistent worry and fear about everyday situations. Anxiety disorders often involve repeated episodes of sudden feelings of intense anxiety and fear or terror that reach a peak within minutes (panic attacks).<ref>[https://www.mayoclinic.org/diseases-conditions/anxiety/symptoms-causes/syc-20350961 Anxiety disorders] ''Mayo Clinic'' Retrieved November 16, 2022.</ref> |
==Types== | ==Types== | ||
Revision as of 17:02, 17 November 2022
| Anxiety disorder | |
| |
| The Scream (Norwegian: Skrik) a painting by Norwegian artist Edvard Munch | |
| Symptoms | Worrying, fast heart rate, shakiness[1] |
|---|---|
| Complications | Depression, insomnia, substance misuse, suicide[2] |
| Usual onset | 15–35 years old[3] |
| Duration | > 6 months[1][3] |
| Causes | Genetic, environmental, and psychological factors[4] |
| Risk factors | Child abuse, family history, poverty[3] |
| Diagnostic method | Psychological assessment |
| Differential diagnosis | Hyperthyroidism; heart disease; caffeine, alcohol, cannabis use; withdrawal from certain drugs[3] |
| Treatment | Lifestyle changes, counselling, medications[3] |
| Medication | Antidepressants, anxiolytics, beta blockers, Pregabalin[4] |
Anxiety disorders are a cluster of mental disorders characterized by significant and uncontrollable feelings of anxiety such that a person's social, occupational, and personal function are significantly impaired. Anxiety may cause physical and cognitive symptoms, such as restlessness, irritability, difficulty concentrating, increased heart rate, abdominal pain, and a variety of other symptoms that vary based on the individual.
There are several types of anxiety disorders, the major ones being generalized anxiety disorder, social anxiety disorder, Obsessive-compulsive disorder, panic disorder, and Post-Traumatic Stress Disorder. Also included within the anxiety disorders are specific phobias, fear of a particular situation or object. It is possible for an individual to have more than one anxiety disorder during their life or at the same time.
Anxiety disorders are common mental disorders. However, they are treatable and most people are able to lead normal productive lives.
Definitions

Anxiety disorders are a cluster of mental disorders characterized by significant and uncontrollable feelings of anxiety and fear such that a person's social, occupational, and personal function are significantly impaired. The anxiety may cause physical and cognitive symptoms, such as restlessness, irritability, easy fatiguability, difficulty concentrating, increased heart rate, chest pain, abdominal pain, and a variety of other symptoms that may vary based on the individual.[1]
In casual discourse, the words anxiety and fear are often used interchangeably. In clinical usage, they have distinct meanings: anxiety is defined as an unpleasant emotional state for which the cause is either not readily identified or perceived to be uncontrollable or unavoidable, whereas fear is an emotional and physiological response to a recognized external threat.[5]
Anxiety is linked to fear and manifests as a future-oriented mood state that consists of a complex cognitive, affective, physiological, and behavioral response system associated with preparation for the anticipated events or circumstances perceived as threatening.[6]
Anxiety is an emotion which is characterized by an unpleasant state of inner turmoil and includes feelings of dread over anticipated events.[7][8] It is a feeling of uneasiness and worry, usually generalized and unfocused as an overreaction to a situation that is only subjectively seen as menacing.[9] Anxiety is often accompanied by nervous behavior such as pacing back and forth, somatic anxiety, and rumination,[10] People facing anxiety may withdraw from situations which have provoked anxiety in the past.[11]
Experiencing occasional anxiety is a normal part of life: "Anxiety is an adaptive response that promotes harm avoidance, but at the same time excessive anxiety constitutes the most common psychiatric complaint."[12] However, people with anxiety disorders frequently have intense, excessive, and persistent worry and fear about everyday situations. Anxiety disorders often involve repeated episodes of sudden feelings of intense anxiety and fear or terror that reach a peak within minutes (panic attacks).[13]
Types
There are multiple forms of anxiety disorder (such as generalized anxiety disorder and obsessive compulsive disorder) with specific clinical definitions.[14] Part of the definition of an anxiety disorder, which distinguishes it from everyday anxiety, is that it is persistent, typically lasting 6 months or more, although the criterion for duration is intended as a general guide with allowance for some degree of flexibility and is sometimes of shorter duration in children.[15]
There are several types of anxiety disorders, the main ones being generalized anxiety disorder, social anxiety disorder, Obsessive-compulsive disorder, panic disorder, and Post-Traumatic Stress Disorder. The individual disorder can be diagnosed using the specific and unique symptoms, triggering events, and timing.[1] If a person is diagnosed with an anxiety disorder, a medical professional must have evaluated the person to ensure the anxiety cannot be attributed to another medical illness or mental disorder.[1] It is possible for an individual to have more than one anxiety disorder during their life or at the same time[1] and anxiety disorders are marked by a typical persistent course.[16]
In addition to these disorders which manifest as severe chronic anxiety, there are also phobias, which manifest as strong, persistent, and irrational fear or anxiety related to certain situations, objects, activities, or persons.
Generalized anxiety disorder
Generalized anxiety disorder (GAD) is a common disorder, characterized by long-lasting anxiety which is not focused on any one object or situation. Those with generalized anxiety disorder experience non-specific persistent fear and worry, and become overly concerned with everyday matters. Generalized anxiety disorder is "characterized by chronic excessive worry accompanied by three or more of the following symptoms: restlessness, fatigue, concentration problems, irritability, muscle tension, and sleep disturbance".[17] Generalized anxiety disorder is the most common anxiety disorder to affect older adults.[18] Anxiety can be a symptom of a medical or substance use disorder problem, and medical professionals must be aware of this. A diagnosis of GAD is made when a person has been excessively worried about an everyday problem for six months or more.[19] These stresses can include family life, work, social life, or their own health. A person may find that they have problems making daily decisions and remembering commitments as a result of lack of concentration and/or preoccupation with worry.[20] A symptom can be a strained appearance, with increased sweating from the hands, feet, and axillae,[21] and they may be tearful, which can suggest depression.[22] Before a diagnosis of anxiety disorder is made, physicians must rule out drug-induced anxiety and other medical causes.[23]
In children, GAD may be associated with headaches, restlessness, abdominal pain, and heart palpitations.[24] Typically it begins around 8 to 9 years of age.[24]
Panic disorder
With panic disorder, a person has brief attacks of intense terror and apprehension, often marked by trembling, shaking, confusion, dizziness, nausea, and/or difficulty breathing. These panic attacks, defined by the APA as fear or discomfort that abruptly arises and peaks in less than ten minutes, can last for several hours.[25] Attacks can be triggered by stress, irrational thoughts, general fear or fear of the unknown, or even exercise. However, sometimes the trigger is unclear and the attacks can arise without warning. To help prevent an attack, one can avoid the trigger. This can mean avoiding places, people, types of behaviors, or certain situations that have been known to cause a panic attack. This being said, not all attacks can be prevented.
In addition to recurrent unexpected panic attacks, a diagnosis of panic disorder requires that said attacks have chronic consequences: either worry over the attacks' potential implications, persistent fear of future attacks, or significant changes in behavior related to the attacks. As such, those with panic disorder experience symptoms even outside specific panic episodes. Often, normal changes in heartbeat are noticed, leading them to think something is wrong with their heart or they are about to have another panic attack. In some cases, a heightened awareness (hypervigilance) of body functioning occurs during panic attacks, wherein any perceived physiological change is interpreted as a possible life-threatening illness (i.e., extreme hypochondriasis).
Post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) was once an anxiety disorder (now moved to trauma- and stressor-related disorders in DSM-V) that results from a traumatic experience. PTSD affects approximately 3.5% of U.S. adults every year, and an estimated one in eleven people will be diagnosed with PTSD in their lifetime.[26] Post-traumatic stress can result from an extreme situation, such as combat, natural disaster, rape, hostage situations, child abuse, bullying, or even a serious accident. It can also result from long-term (chronic) exposure to a severe stressor—[27] for example, soldiers who endure individual battles but cannot cope with continuous combat. Common symptoms include hypervigilance, flashbacks, avoidant behaviors, anxiety, anger and depression.[28] In addition, individuals may experience sleep disturbances.[29] People who have PTSD often try to detach themselves from their friends and family, and have difficulty maintaining these close relationships. There are a number of treatments that form the basis of the care plan for those with PTSD. Such treatments include cognitive behavioral therapy (CBT), prolonged exposure therapy, stress inoculation therapy, medication, and psychotherapy and support from family and friends.[19]
Post-traumatic stress disorder (PTSD) research began with Vietnam veterans, as well as natural and non-natural disaster victims. Studies have found the degree of exposure to a disaster has been found to be the best predictor of PTSD.[30]
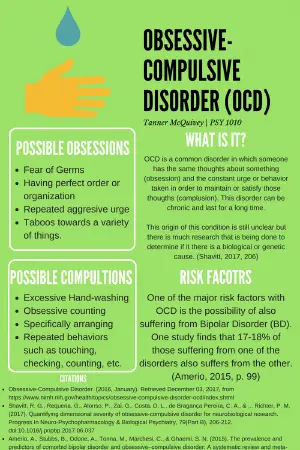
Obsessive–compulsive disorder
Obsessive–compulsive disorder (OCD) is not classified as an anxiety disorder by the DSM-5, but is by the ICD-10. It was previously classified as an anxiety disorder in the DSM-IV. It is a condition where the person has obsessions (distressing, persistent, and intrusive thoughts or images) and compulsions (urges to repeatedly perform specific acts or rituals), that are not caused by drugs or physical disorder, and which cause distress or social dysfunction.[31][32] The compulsive rituals are personal rules followed to relieve the feeling of discomfort.[32] OCD affects roughly 1–2% of adults (somewhat more women than men), and under 3% of children and adolescents.[31][32]
A person with OCD knows that the symptoms are unreasonable and struggles against both the thoughts and the behavior.[31][33] Their symptoms could be related to external events they fear (such as their home burning down because they forget to turn off the stove) or worry that they will behave inappropriately.[33]
It is not certain why some people have OCD, but behavioral, cognitive, genetic, and neurobiological factors may be involved.[32] Risk factors include family history, being single (although that may result from the disorder), and higher socioeconomic class or not being in paid employment.[32] Of those with OCD about 20% of people will overcome it, and symptoms will at least reduce over time for most people (a further 50%).[31]
Social anxiety disorder
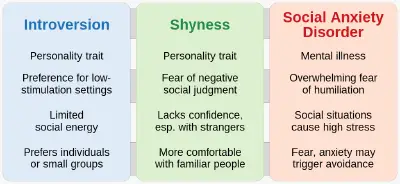
Social anxiety disorder (SAD; also known as social phobia) describes an intense fear and avoidance of negative public scrutiny, public embarrassment, humiliation, or social interaction. This fear can be specific to particular social situations (such as public speaking) or, more typically, is experienced in most (or all) social interactions. Roughly 7% of American adults have social anxiety disorder, and more than 75% of people experience their first symptoms in their childhood or early teenage years.[34] Social anxiety often manifests specific physical symptoms, including blushing, sweating, rapid heart rate, and difficulty speaking.[35] As with all phobic disorders, those with social anxiety often will attempt to avoid the source of their anxiety; in the case of social anxiety this is particularly problematic, and in severe cases can lead to complete social isolation.
Children are also affected by social anxiety disorder, although their associated symptoms are different than that of teenagers and adults. They may experience difficulty processing or retrieving information, sleep deprivation, disruptive behaviors in class, and irregular class participation.[36]
Specific phobias
The specific phobias are a category of anxiety disorders which includes all cases in which fear and anxiety are triggered by a specific stimulus or situation. Between 5% and 12% of the population worldwide have specific phobias.[19] According to the National Institute of Mental Health, a phobia is an intense fear of or aversion to specific objects or situations.[37] Individuals with a phobia typically anticipate terrifying consequences from encountering the object of their fear, which can be anything from an animal to a location to a bodily fluid to a particular situation. Common phobias are flying, blood, water, highway driving, and tunnels. When people are exposed to their phobia, they may experience trembling, shortness of breath, or rapid heartbeat.[38] Thus meaning that people with specific phobias often go out of their way to avoid encountering their phobia. People understand that their fear is not proportional to the actual potential danger but still are overwhelmed by it.[39]
Diagnosis
The diagnosis of anxiety disorders is made by symptoms, triggers, and a person's personal and family histories. There are no objective biomarkers or laboratory tests that can diagnose anxiety.[40] It is important for a medical professional to evaluate a person for other medical and mental causes for prolonged anxiety because treatments will vary considerably.[1]
Numerous questionnaires have been developed for clinical use and can be used for an objective scoring system. Symptoms may be vary between each subtype of generalized anxiety disorder. Generally, symptoms must be present for at least six months, occur more days than not, and significantly impair a person's ability to function in daily life. Symptoms may include: feeling nervous, anxious, or on edge; worrying excessively; difficulty concentrating; restlessness; irritability.[1][3]
Questionnaires developed for clinical use include the State-Trait Anxiety Inventory (STAI), the Generalized Anxiety Disorder 7 (GAD-7), the Beck Anxiety Inventory (BAI), the Zung Self-Rating Anxiety Scale, and the Taylor Manifest Anxiety Scale.[40] Other questionnaires combine anxiety and depression measurement, such as the Hamilton Anxiety Rating Scale, the Hospital Anxiety and Depression Scale (HADS), the Patient Health Questionnaire (PHQ), and the Patient-Reported Outcomes Measurement Information System (PROMIS).[40] Examples of specific anxiety questionnaires include the Liebowitz Social Anxiety Scale (LSAS), the Social Interaction Anxiety Scale (SIAS), the Social Phobia Inventory (SPIN), the Social Phobia Scale (SPS), and the Social Anxiety Questionnaire (SAQ-A30).[41]
Differential diagnosis
Anxiety disorders differ from developmentally normal fear or anxiety by being excessive or persisting beyond developmentally appropriate periods. They differ from transient fear or anxiety, often stress-induced, by being persistent (e.g., typically lasting 6 months or more), although the criterion for duration is intended as a general guide with allowance for some degree of flexibility and is sometimes of shorter duration in children.[1]
The diagnosis of an anxiety disorder requires first ruling out an underlying medical cause.[42][5] Diseases that may present similar to an anxiety disorder, including certain endocrine diseases (hypo- and hyperthyroidism, hyperprolactinemia),[3][42][43] metabolic disorders (diabetes),[42][44] deficiency states (low levels of vitamin D, B2, B12, folic acid),[42] gastrointestinal diseases (celiac disease, non-celiac gluten sensitivity, inflammatory bowel disease),[45][46][47] heart diseases,[3][42] blood diseases (anemia),[42] and brain degenerative diseases (Parkinson's disease, dementia, multiple sclerosis, Huntington's disease).[42][48][49][50]
Several drugs can also cause or worsen anxiety, whether in intoxication, withdrawal, or from chronic use. These include alcohol, tobacco, cannabis, sedatives (including prescription benzodiazepines), opioids (including prescription painkillers and illicit drugs like heroin), stimulants (such as caffeine, cocaine and amphetamines), hallucinogens, and inhalants.[3][1]
Prevention
Focus is increasing on prevention of anxiety disorders.[51] There is tentative evidence to support the use of cognitive behavioral therapy[51] and mindfulness therapy.[52][53] A 2013 review found no effective measures to prevent GAD in adults.[54] A 2017 review found that psychological and educational interventions had a small benefit for the prevention of anxiety.[55][56] Research indicates that predictors of the emergence of anxiety disorders partly differ from the factors that predict their persistence.[16]
Treatment
Treatment options include lifestyle changes, therapy, and medications. There is no clear evidence as to whether therapy or medication is most effective; the specific medication decision can be made by a doctor and patient with consideration to the patient's specific circumstances and symptoms.[57] If while on treatment with a chosen medication, the person's anxiety does not improve, another medication may be offered.[57] Specific treatments will vary by subtype of anxiety disorder, a person's other medical conditions, and medications.
Lifestyle and diet
Lifestyle changes include exercise, for which there is moderate evidence for some improvement, regularizing sleep patterns, reducing caffeine intake, and stopping smoking.[57] Stopping smoking has benefits in anxiety as large as or larger than those of medications.[58] Omega-3 polyunsaturated fatty acids, such as fish oil, may reduce anxiety, particularly in those with more significant symptoms.[59]
Psychotherapy
Cognitive behavioral therapy (CBT) is effective for anxiety disorders and is a first-line treatment.[57][60][61][62][63]Template:Excessive citations inline CBT appears to be equally effective when carried out via the internet compared to sessions completed face to face.[63][64]
Mindfulness-based programs also appear to be effective for managing anxiety disorders.[65][66] It is unclear if meditation has an effect on anxiety and transcendental meditation appears to be no different than other types of meditation.[67]
A 2015 Cochrane review of Morita therapy for anxiety disorder in adults found not enough evidence to draw a conclusion.[68]
Adventure-based counseling can be an effective way to anxiety. Using rock-climbing as an example, climbing can often bring on fear or frustration, and tackling these negative feelings in a nurturing environment can help people develop coping mechanisms necessary to deal with these negative feelings.[69]
Medications
First-line choices for medications include SSRIs or SNRIs to treat generalized anxiety disorder.[57][70] There is no good evidence supporting which specific medication in the SSRI or SNRI class is best for treating anxiety, so cost often drives drug choice.[57][70] If they are effective, it is recommended that they are continued for at least a year.[71] Stopping these medications results in a greater risk of relapse.[72]
Buspirone and pregabalin are second-line treatments for people who do not respond to SSRIs or SNRIs; there is also evidence that benzodiazepines, including diazepam and clonazepam, are effective.[57] Pregabalin and gabapentin are effective in treating some anxiety disorders but there is concern regarding their off-label use due to the lack of strong scientific evidence for their efficacy in multiple conditions and their proven side effects.[73][74]
Medications need to be used with care among older adults, who are more likely to have side effects because of coexisting physical disorders. Adherence problems are more likely among older people, who may have difficulty understanding, seeing, or remembering instructions.[18]
In general, medications are not seen as helpful in specific phobia, but a benzodiazepine is sometimes used to help resolve acute episodes. In 2007, data were sparse for efficacy of any drug.[75]
Children
Both therapy and a number of medications have been found to be useful for treating childhood anxiety disorders.[76] Therapy is generally preferred to medication.[77]
Cognitive behavioral therapy (CBT) is a good first therapy approach.[77] Studies have gathered substantial evidence for treatments that are not CBT-based as being effective forms of treatment, expanding treatment options for those who do not respond to CBT.[77] Although studies have demonstrated the effectiveness of CBT for anxiety disorders in children and adolescents, evidence that it is more effective than treatment as usual, medication, or wait list controls is inconclusive.[78] Like adults, children may undergo psychotherapy, cognitive-behavioral therapy, or counseling. Family therapy is a form of treatment in which the child meets with a therapist together with the primary guardians and siblings.[79] Each family member may attend individual therapy, but family therapy is typically a form of group therapy. Art and play therapy are also used. Art therapy is most commonly used when the child will not or cannot verbally communicate, due to trauma or a disability in which they are nonverbal. Participating in art activities allows the child to express what they otherwise may not be able to communicate to others.[80] In play therapy, the child is allowed to play however they please as a therapist observes them. The therapist may intercede from time to time with a question, comment, or suggestion. This is often most effective when the family of the child plays a role in the treatment.[79][81]
If a medication option is warranted, antidepressants such as SSRIs and SNRIs can be effective.[76] Minor side effects with medications, however, are common.[76]
Epidemiology
Globally, as of 2010, approximately 273 million (4.5% of the population) had an anxiety disorder.[82] It is more common in females (5.2%) than males (2.8%).[82]
In Europe, Africa and Asia, lifetime rates of anxiety disorders are between 9 and 16%, and yearly rates are between 4 and 7%.[83] In the United States, the lifetime prevalence of anxiety disorders is about 29%[84] and between 11 and 18% of adults have the condition in a given year.[83] This difference is affected by the range of ways in which different cultures interpret anxiety symptoms and what they consider to be normative behavior.[85][86] In general, anxiety disorders represent the most prevalent psychiatric condition in the United States, outside of substance use disorder.[87]
Like adults, children can experience anxiety disorders; between 10 and 20 percent of all children will develop a full-fledged anxiety disorder prior to the age of 18,[88] making anxiety the most common mental health issue in young people. Anxiety disorders in children are often more challenging to identify than their adult counterparts, owing to the difficulty many parents face in discerning them from normal childhood fears. Likewise, anxiety in children is sometimes misdiagnosed as attention deficit hyperactivity disorder or, due to the tendency of children to interpret their emotions physically (as stomachaches, headaches, etc.), anxiety disorders may initially be confused with physical ailments.[89]
Anxiety in children has a variety of causes; sometimes anxiety is rooted in biology, and may be a product of another existing condition, such as autism spectrum disorder.[90] Gifted children are also often more prone to excessive anxiety than non-gifted children.[91] Other cases of anxiety arise from the child having experienced a traumatic event of some kind, and in some cases, the cause of the child's anxiety cannot be pinpointed.[92]
Anxiety in children tends to manifest along age-appropriate themes, such as fear of going to school (not related to bullying) or not performing well enough at school, fear of social rejection, fear of something happening to loved ones, etc. What separates disordered anxiety from normal childhood anxiety is the duration and intensity of the fears involved.[89]
Stigma
People with an anxiety disorder may be challenged by prejudices and stereotypes that the world believes, most likely as a result of misconception around anxiety and anxiety disorders.[93] Misconceptions found in a data analysis from the National Survey of Mental Health Literacy and Stigma include (1) many people believe anxiety is not a real medical illness; and (2) many people believe that people with anxiety could turn it off if they wanted to.[94] For people experiencing the physical and mental symptoms of an anxiety disorder, stigma and negative social perception can make an individual less likely to seek treatment.[94]
There are two prevalent types of stigmas that surround anxiety disorders: Public and Self-Stigma. Public stigma in this context is the reaction that the general population has to people with an anxiety disorder. Self-Stigma is described as the prejudice which people with mental illness turn against themselves.[93]
There is no explicit evidence that announces the exact cause of stigma towards anxiety, however there are three highlighted perspectives. The macro, intermediate, and micro levels. The macro level marks society as whole with the influence from mass media. The intermediate level includes health care professionals and their perspective. The micro level details the individuals contributions to the process through self-stigmatization.[95]
Stigma can be described in three conceptual ways: cognitive, emotional, and behavioural. This allows for differentiation between stereotypes, prejudice, and discrimination.[95]
Notes
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5 (American Psychiatric Publishing, 2013, ISBN 978-0890425558).
- ↑ Anxiety disorders – Symptoms and causes: Complications Mayo Clinic. Retrieved November 17, 2022.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Michelle G. Craske and Murray B. Stein, Anxiety Lancet 388(10063) (2016): 3048–3059. Retrieved November 17, 2022.
- ↑ 4.0 4.1 Anxiety Disorders National Institute of Mental Health. Retrieved November 17, 2022.
- ↑ 5.0 5.1 World Health Organization, Pharmacological Treatment of Mental Disorders in Primary Health Care (World Health Organization, 2010, ISBN 978-9241547697).
- ↑ Suma P. Chand and Raman Marwaha,Anxiety StatPearls Publishing, 2022. Retrieved November 17, 2022.
- ↑ Gerald C. Davison, Kirk R. Blankstein, Gordon L. Flett, and John M. Neale, Abnormal Psychology (Wiley, 2008, ISBN 978-0470840726).
- ↑ Maria Miceli and Cristiano Castelfranchi, Expectancy and Emotion (Oxford University Press, 2015, ISBN 978-0199685868).
- ↑ Colin Hemmings and Nick Bouras (eds.), Psychiatric and Behavioral Disorders in Intellectual and Developmental Disabilities (Cambridge University Press, 2016, ISBN 978-1107645943).
- ↑ Martin E. P. Seligman, Elaine F. Walker, and David L. Rosenhan, Abnormal psychology (W. W. Norton & Company, 2001, ISBN 978-0393944594).
- ↑ Mary Chambers (ed.), Psychiatric and Mental Health Nursing: The craft of caring (Routledge, 2017, ISBN 1482221950).
- ↑ Oliver J. Robinson, Alexandra C. Pike, Brian Cornwell, and Christian Grillon, The translational neural circuitry of anxiety Journal of Neurology, Neurosurgery, and Psychiatry 90(12) (2019): 1353-1360. Retrieved November 17, 2022.
- ↑ Anxiety disorders Mayo Clinic Retrieved November 16, 2022.
- ↑ (2005) Treating and preventing adolescent mental health disorders: what we know and what we don't know. A research agenda for improving the mental health of our youth. Oxford University Press. DOI:10.1093/9780195173642.001.0001. ISBN 978-0-19-517364-2. OCLC 56324679.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedDSM-5 - ↑ 16.0 16.1 Hovenkamp-Hermelink (2021). Predictors of persistence of anxiety disorders across the lifespan: a systematic review. The Lancet Psychiatry 8 (5): 428–443.
- ↑ Schacter, D. L., Gilbert, D. T., & Wegner, D.M. (2011). Psychology: Second Edition. New York, NY: Worth.
- ↑ 18.0 18.1 (2008). Anxiety Disorders in Later Life: Differentiated Diagnosis and Treatment Strategies. Psychiatric Times 26 (8).
- ↑ 19.0 19.1 19.2 Phil Barker (7 October 2003). Psychiatric and mental health nursing: the craft of caring. London: Arnold. ISBN 978-0-340-81026-2.
- ↑ Psychology, Michael Passer, Ronald Smith, Nigel Holt, Andy Bremner, Ed Sutherland, Michael Vliek (2009) McGrath Hill Education, UK: McGrath Hill Companies Inc. p 790
- ↑ All About Anxiety Disorders: From Causes to Treatment and Prevention.
- ↑ Psychiatry, Michael Gelder, Richard Mayou, John Geddes 3rd ed. Oxford; New York: Oxford University Press, c 2005 p. 75
- ↑ Varcarolis. E (2010). Manual of Psychiatric Nursing Care Planning: Assessment Guides, Diagnoses and Psychopharmacology. 4th ed. New York: Saunders Elsevier. p 109.
- ↑ 24.0 24.1 Keeton, CP (2009). Pediatric generalized anxiety disorder: epidemiology, diagnosis, and management.. Paediatric Drugs 11 (3): 171–83.
- ↑ Panic Disorder.
- ↑ What Is PTSD?.
- ↑ (2006) Post-Traumatic Stress Disorder and the Family. Veterans Affairs Canada. ISBN 978-0-662-42627-1.
- ↑ Psychological Disorders {{#invoke:webarchive|webarchive}}, Psychologie Anglophone
- ↑ (2017). Post-Traumatic Stress Disorder. New England Journal of Medicine 376 (25): 2459–2469.
- ↑ Fullerton, Carol (1997). Posttraumatic Stress Disorder. Washington, D.C.: American Psychiatric Press Inc., 8–9. ISBN 978-0-88048-751-1.
- ↑ 31.0 31.1 31.2 31.3 (2006) Obsessive-Compulsive Disorder: Core Interventions in the Treatment of Obsessive-Compulsive Disorder and Body Dysmorphic Disorder. ISBN 9781854334305.
- ↑ 32.0 32.1 32.2 32.3 32.4 (18 January 2012) Obsessive compulsive disorder.. BMJ Clinical Evidence 2012.
- ↑ 33.0 33.1 Obsessive-compulsive disorder: overview. Institute for Quality and Efficiency in Health Care (IQWiG).
- ↑ Social Anxiety Disorder (in en).
- ↑ NIMH » Social Anxiety Disorder: More Than Just Shyness.
- ↑ Managing Anxiety in the Classroom (in en).
- ↑ NIMH » Anxiety Disorders.
- ↑ U.S. Department of Health & Human Services (2017). Phobias (in en-us).
- ↑ Psychology. Michael Passer, Ronald Smith, Nigel Holt, Andy Bremner, Ed Sutherland, Michael Vliek. (2009) McGrath Hill Higher Education; UK: McGrath Hill companies Inc.
- ↑ 40.0 40.1 40.2 (2014). Assessment of patient-reported symptoms of anxiety. Dialogues Clin Neurosci 16 (2): 197–211 (Table 1).Template:Open access
- ↑ (2014). Assessment of patient-reported symptoms of anxiety. Dialogues Clin Neurosci 16 (2): 197–211 (Table 2).Template:Open access
- ↑ 42.0 42.1 42.2 42.3 42.4 42.5 42.6 (2013). Psychiatric emergencies (part III): psychiatric symptoms resulting from organic diseases. European Review for Medical and Pharmacological Sciences 17 (s1): 86–99. Template:Open access
- ↑ Samuels MH (2008). Cognitive function in untreated hypothyroidism and hyperthyroidism. Current Opinion in Endocrinology, Diabetes and Obesity 15 (5): 429–33.
- ↑ (2002). Prevalence of anxiety in adults with diabetes: a systematic review. Journal of Psychosomatic Research 53 (6): 1053–60.
- ↑ (April 2015) Psychological morbidity of celiac disease: A review of the literature. United European Gastroenterology Journal 3 (2): 136–45.
- ↑ (May 2015) Systematic review: noncoeliac gluten sensitivity. Alimentary Pharmacology & Therapeutics 41 (9): 807–20.
- ↑ (2016). Depression and anxiety in patients with Inflammatory Bowel Disease: A systematic review. Journal of Psychosomatic Research 87: 70–80.
- ↑ (2016). The prevalence of neuropsychiatric symptoms in Alzheimer's disease: Systematic review and meta-analysis. Journal of Affective Disorders 190: 264–71.
- ↑ (2016). Depression, anxiety, and apathy in Parkinson's disease: insights from neuroimaging studies. European Journal of Neurology 23 (6): 1001–19.
- ↑ (2015). The incidence and prevalence of psychiatric disorders in multiple sclerosis: a systematic review. Multiple Sclerosis Journal 21 (3): 305–17.
- ↑ 51.0 51.1 Bienvenu, OJ (December 2007). Prevention of anxiety disorders. International Review of Psychiatry 19 (6): 647–54.
- ↑ (Aug 2013) Mindfulness-based therapy: a comprehensive meta-analysis. Clinical Psychology Review 33 (6): 763–71.
- ↑ (Jul 2014) Mindfulness-based stress reduction as a stress management intervention for healthy individuals: a systematic review. J Evid Based Complementary Altern Med 19 (4): 271–86.
- ↑ (3 December 2013)In the clinic. Generalized anxiety disorder.. Annals of Internal Medicine 159 (11): ITC6–1, ITC6–2, ITC6–3, ITC6–4, ITC6–5, ITC6–6, ITC6–7, ITC6–8, ITC6–9, ITC6–10, ITC6–11; quiz ITC6–12.
- ↑ (1 October 2017) Effectiveness of Psychological and/or Educational Interventions in the Prevention of Anxiety: A Systematic Review, Meta-analysis, and Meta-regression.. JAMA Psychiatry 74 (10): 1021–1029.
- ↑ (2019) "8 - Targeting anxiety sensitivity as a prevention strategy", The Clinician's Guide to Anxiety Sensitivity Treatment and Assessment. Academic Press, 145–178. ISBN 978-0-12-813495-5.
- ↑ 57.0 57.1 57.2 57.3 57.4 57.5 57.6 (19 November 2015) Clinical Practice: Generalized Anxiety Disorder.. The New England Journal of Medicine 373 (21): 2059–68.
- ↑ Taylor, G. (13 February 2014). Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ 348 (feb13 1): g1151.
- ↑ (2018). Association of Use of Omega-3 Polyunsaturated Fatty Acids With Changes in Severity of Anxiety Symptoms. JAMA Network Open 1 (5): e182327.
- ↑ Cuijpers, P (Mar 2014). Psychological treatment of generalized anxiety disorder: A meta-analysis.. Clinical Psychology Review 34 (2): 130–140.
- ↑ Otte, C (2011). Cognitive behavioral therapy in anxiety disorders: current state of the evidence.. Dialogues in Clinical Neuroscience 13 (4): 413–21.
- ↑ (13 April 2016)Psychological therapies for panic disorder with or without agoraphobia in adults: a network meta-analysis.. The Cochrane Database of Systematic Reviews 2016 (4): CD011004.
- ↑ 63.0 63.1 (12 March 2016) Therapist-supported Internet cognitive behavioural therapy for anxiety disorders in adults.. The Cochrane Database of Systematic Reviews 2016 (3): CD011565.
- ↑ (2013-09-09) Media-delivered Cognitive Behavioural Therapy and Behavioural Therapy (Self-Help) for Anxiety Disorders in Adults. The Cochrane Database of Systematic Reviews (9): CD005330.
- ↑ (Nov 2013) Mindfulness and acceptance-based behavioral therapies for anxiety disorders. Curr Psychiatry Rep 15 (11): 410.
- ↑ Lang AJ (May 2013). What mindfulness brings to psychotherapy for anxiety and depression. Depress Anxiety 30 (5): 409–12.
- ↑ (25 January 2006) Meditation therapy for anxiety disorders.. The Cochrane Database of Systematic Reviews (1): CD004998.
- ↑ (19 February 2015) Morita therapy for anxiety disorders in adults. Cochrane Database of Systematic Reviews (2): CD008619.
- ↑ (2022-02-17)Wall Climbing Therapy for Adults Diagnosed with Complex PTSD Due Childhood Sexual Assault. Journal of Loss and Trauma 27 (2): 191–193.
- ↑ 70.0 70.1 (2014-04-08)Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: A revision of the 2005 guidelines from the British Association for Psychopharmacology. Journal of Psychopharmacology 28 (5): 403–439.
- ↑ (13 September 2017) Risk of relapse after antidepressant discontinuation in anxiety disorders, obsessive-compulsive disorder, and post-traumatic stress disorder: systematic review and meta-analysis of relapse prevention trials. BMJ 358: j3927.
- ↑ (13 September 2017) Risk of relapse after antidepressant discontinuation in anxiety disorders, obsessive-compulsive disorder, and post-traumatic stress disorder: systematic review and meta-analysis of relapse prevention trials.. BMJ (Clinical Research Ed.) 358: j3927.
- ↑ (2022-10-17)Review finds little evidence to support gabapentinoid use in bipolar disorder or insomnia. NIHR Evidence.
- ↑ (March 2022) Gabapentin and pregabalin in bipolar disorder, anxiety states, and insomnia: Systematic review, meta-analysis, and rationale. Molecular Psychiatry 27 (3): 1339–1349.
- ↑ (April 2007) Treatment of specific phobia in adults.. Clinical Psychology Review 27 (3): 266–86.
- ↑ 76.0 76.1 76.2 (31 August 2017) Comparative Effectiveness and Safety of Cognitive Behavioral Therapy and Pharmacotherapy for Childhood Anxiety Disorders. JAMA Pediatrics 171 (11): 1049–1056.
- ↑ 77.0 77.1 77.2 (18 June 2015) Evidence Base Update: 50 Years of Research on Treatment for Child and Adolescent Anxiety.. Journal of Clinical Child and Adolescent Psychology 45 (2): 91–113.
- ↑ (2015-02-18) Cognitive behavioural therapy for anxiety disorders in children and adolescents. The Cochrane Database of Systematic Reviews 2020 (2): CD004690.
- ↑ 79.0 79.1 (2015-05-25)Treatment of childhood anxiety disorder in the context of maternal anxiety disorder: a randomised controlled trial and economic analysis. Health Technology Assessment 19 (38): 1–184.
- ↑ (1999). Family assessment and intervention using an interactive are exercise. Australian and New Zealand Journal of Family Therapy 20 (2): 61–69.
- ↑ Bratton, S.C., & Ray, D. (2002). Humanistic play therapy. In D.J. Cain (Ed.), Humanistic psychotherapies: Handbook of research and practice (pp. 369-402). Washington, DC: American Psychological Association.
- ↑ 82.0 82.1 (15 December 2012) Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380 (9859): 2163–96.
- ↑ 83.0 83.1 (2010) Anxiety disorders : theory, research, and clinical perspectives, 1. publ., Cambridge, UK: Cambridge University Press. ISBN 978-0-521-51557-3.
- ↑ (June 2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 62 (6): 593–602.
- ↑ (2014) "6", Social Anxiety: Clinical, Developmental, and Social Perspectives, 3, Elsevier. DOI:10.1016/B978-0-12-394427-6.00006-6. ISBN 978-0-12-394427-6.
- ↑ (December 2010) Cultural Aspects in Social Anxiety and Social Anxiety Disorder. Depress Anxiety 27 (12): 1117–1127.
- ↑ (12 August 2004) Generalized Anxiety Disorder. New England Journal of Medicine 351 (7): 675–682.
- ↑ (2006) Child and Adolescent Psychopathology: Theoretical and Clinical Implications. Hove, East Sussex: Routledge.
- ↑ 89.0 89.1 GENERALIZED ANXIETY. AnxietyBC (2014-11-14).
- ↑ Anxiety and Autism Spectrum Disorders. Indiana Resource Center for Autism.
- ↑ (2012). Perfectionism and Anxiety: A Paradox in Intellectual Giftedness?. PLOS ONE 7 (7): e41043.
- ↑ Anxiety Disorders During Childhood and Adolescence: Origins and Treatment. Annual Review of Clinical Psychology.
- ↑ 93.0 93.1 Corrigan, Patrick W. (February 2016). Lessons learned from unintended consequences about erasing the stigma of mental illness. World Psychiatry 15 (1): 67–73.
- ↑ 94.0 94.1 beyondblue. Stigma relating to anxiety - Beyond Blue (in en).
- ↑ 95.0 95.1 Rossler, Wulf (2016). The stigma of mental disorders. EMBO Reports 17 (9): 1250–1253.
ReferencesISBN links support NWE through referral fees
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. American Psychiatric Publishing, 2013. ISBN 978-0890425558
- Chambers, Mary (ed.). Psychiatric and Mental Health Nursing: The craft of caring. Routledge, 2017. ISBN 1482221950
- Davison, Gerald C., Kirk R. Blankstein, Gordon L. Flett, and John M. Neale. Abnormal Psychology. Wiley, 2008. ISBN 978-0470840726
- Miceli, Maria, and Cristiano Castelfranchi. Expectancy and Emotion. Oxford University Press, 2015. ISBN 978-0199685868
- Seligman, Martin E. P., Elaine F. Walker, and David L. Rosenhan. Abnormal psychology. W. W. Norton & Company, 2001. ISBN 978-0393944594
- World Health Organization. Pharmacological Treatment of Mental Disorders in Primary Health Care. World Health Organization, 2010. ISBN 978-9241547697
External links
All links retrieved
- Anxiety disorders Mayo Clinic
- Anxiety Disorders National Institute of Mental Health
- Anxiety Disorders Cleveland Clinic
- What are Anxiety Disorders? American Psychiatric Association
- What are the five major types of anxiety disorders? U.S. Department of Health & Human Services
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.