Bursitis
| Bursitis Classification and external resources | |
| Bursitis of the Elbow | |
| ICD-10 | M71.9 |
| ICD-9 | 727.3 |
| DiseasesDB | 31623 |
| MedlinePlus | 000419 |
| eMedicine | emerg/74  |
| MeSH | D002062 |
Bursitis is the inflammation of one or more bursae, the fluid-filled sacs that rest adjacent to tendons, bones, and other tissues and create a smooth gliding surface and cushion. For example, bursae are located adjacent to tendons in elbow, shoulder, ankle, knee, heel, and hip. When bursitis takes hold, perhaps due to overuse, injury, or infection, the movement that relies on the inflamed bursa becomes rough and painful.
Bursitis is usually a temporary condition that causes pain and may restrain motion, and in chronic can lead to muscle deterioration; it generally does not cause deformity. It is common among people who are repeatedly using a limb or using it with excessive pressure, such as in baseball, tennis, running, shoveling snow, house painting, and so forth. The appearance of bursitis reflects on how harmoniously the human body normally works, allowing the muscles, tendons, and bones to interact seamlessly because of these small sacs.
Bursitis may be associated with other diseases, such as arthritis, thyroid disease, and diabetes (NYPH 2007).
Overview
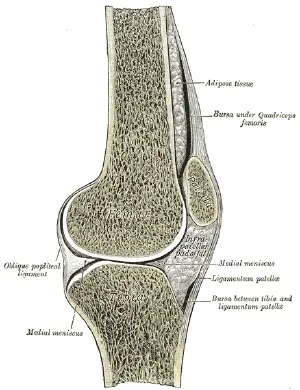
A bursa (plural bursae or bursas) is a small, closed, fluid-filled sac that is composed of white fibrous tissue. Bursae rest at the points where internal functionaries, like muscles and tendons, slide across bone. Bursae are found around almost every major joint of the body, providing a cushion between bones and tendons and/or muscles around the joint, and acting as a smooth and almost frictionless gliding surface as they move back and forth across each other. With hundreds of them throughout the body, bursae provide this surface for all motion, making movement normally painless.
Bursitis is the inflammation of one or more of these bursae which are lined with a synovial membrane that secretes a lubricating synovial fluid (Vigorita 2015). Inflammation is a localized protective response of a body's living tissue to injury, infection, irritation, or allergy. Inflammation is characterized by the following quintet: Redness (rubor), heat (calor), swelling (tumor), pain (dolor), and dysfunction of the organs involved (functio laesa).
When bursitis occurs, the individual can experience pain, localized tenderness, and limited motion, as well as swelling and redness if the inflamed bursa is close to the surface (NYPH 2007). Movement of tendons and muscles over the inflamed bursa causes it to become more inflamed, perpetuating the problem. In chronic bursitis, there may be repeated attacks of pain, tenderness, and swelling, possibly leading to deterioration of the muscles (NYPH 2007).
The major bursae are located near the large joints, such as shoulders, hips, elbows, and knees (NYPH 2007). These tend to be the most common areas affected with bursitis.
Causes
Trauma, auto-immune disorders, infection, and iatrogenic (medicine-related) factors can all cause bursitis (Vigorita 2015).
Bursitis is commonly caused by repetition of movement or excessive pressure. Elbows and knees are the most commonly affected because they are rested upon more than many parts of the body with bursae and they also get the most repetitive use. Individuals that are overusing a limb or using it incorrectly, or that are in poor physical condition and with bad postures are at risk of developing bursitis (NYPH 2007). When there is compression of the bursa on a regular basis, such as a person who sleeps on the side and places significant pressure on the hip or shoulder for a long time, the person may become at risk of bursitis when continuing movement of this compressed area (BS 2005).
The other main cause of bursitis is traumatic injury, which can cause swelling of the bursae. The swelling itself causes irritation because the sac will no longer fit in the small area between the bone and the functionary. When the bone begins to increase pressure on the bursa, bursitis ensues.
Infection can be a probable cause as well (NYPH 2007). Inflammation of bursae can also be caused by other inflammatory conditions, such as rheumatoid arthritis, scleroderma, systemic lupus erythematosus, and gout. Immune deficiencies, including HIV and diabetes, can also cause bursitis (Vigorita 2015). Scoliosis can also be a cause of bursitis of the shoulders, although this is rare.
Types
Among the more common types of bursitis are the following.
- Kneecap bursitis. This bursitis is medically known as prepatellar bursitis and also called housemaid's knee. One of several types of bursa in the knee is known as the prepatellar bursa, and is located in front of the kneecap adjacent to the attachment of the patellar tendon (AAOS 2025). This may result from kneeling on a hard or raised surface for long periods, such as maids cleaning floors on their knees, or skilled laborers such as carpet layers or plumbers who are on their knees often (NYPH 2007). It is also common among wrestlers, from their knees rubbing on the mats, or among volleyball players who are diving onto the floor for the ball (AAOS 2025).
- Knee bursitis. Known medically as pes anserine bursitis, or also commonly as goosefoot bursitis, this affects the pes anserine bursa located on the inner side of the knee below the knee joint, between the shin bone and the three tendons of the hamstring muscles that attach to the shin bone (tibia) (NYPH 2007). This might result from lack of stretching before exercise, out-turning of the knee or lower leg, being overweight, or arthritis, and is also common among swimmers who do the breaststroke (NYPH 2007).
- Elbow bursitis. Known medically as olecranon bursitis and also nicknamed student's elbow, this affects the olecranon bursa located between the skin and bones of the elbow (NYPH 2007). This results from repeated pressure on the point of the elbow, such as leaning on a hard surface, as on a table or desk for a long time.
- Anterior Achilles tendon bursitis. Also called Albert's disease, this is characterized by inflammation of the bursa located in front of the attachment of the tendon to the heel, caused by extra strain on the Achilles tendon, such as injury or shoes with rigid back support (NYPH 2007).
- Posterior Achilles tendon bursitis. Otherwise known as Haglund's deformity, this involves inflammation of bursa located between the skin of the heel and the Achilles tendon, which attaches the calf muscles to the heel (NYPH 2007). This commonly results from a type of walking, such as among young women, whereby the soft heel tissue is pushed to the hard, back support of a shoe.
- Hip bursitis. Known medically as trochanteric bursitis, this involves inflammation of the trochanteric bursa, which is located on the outer, upper area of the thigh, over the greater trochanger (which is a bump on the outerside of the upper part of the femur. It may be a result of injury, overuse, arthritis, spinal abnormalities, or surgery, and may occur with running, walking, or bicycling. This type of bursitis is also more common among women, middle-aged people, and older people (NYPH 2007).
- Shoulder bursitis. This results from inflammation of the shoulder bursa, such as with sports with overhead movements (swimming, tennis, baseball, throwing) or activities such as painting and carpentry (AAOS 2025).
- Buttocks bursitis. This involves an inflamed bursa over the bone in one's buttocks, perhaps from sitting on a hard surface for a long period, such as from bicycling (Mayo 2007).
Symptoms and diagnosis
The symptoms of bursitis can be as varied as the causes and types of bursitis. It can range from an achy pain and stiffness in the local area of the joint to a burning sensation in the area surrounding the whole joint with the inflamed bursa. The pain usually escalates during and after activity, with the bursa and the surrounding joint area becoming stiffer the following day.
Apart from pain, one finds localized tenderness and limited motion to be common among people who have bursitis. Swelling and redness may occur if the inflamed bursa is close to the surface (Vigorita 2015). Repeated attacks of pain, swelling, and tenderness, possibly leading to the deterioration of muscles and a limited range-of-motion, is a case of chronic bursitis.
Firstly, an analysis of complete medical history and physical examination is mandatory. As the symptoms of bursitis resemble other medical conditions or problems, an accurate diagnosis is important. So other intensive diagnostic procedures are also employed. A sample of fluid from the bursa is obtained to rule out infections and to find the cause of the bursitis. Other tests that may be run are x-rays, computed tomography scan (CT or CAT scan), magnetic resonance imaging (MRI), anthrogram to provide evidence of a tear, opening, or blockage, and aspiration to rule out infection or gout as causes (NYPH 2007).
Treatment and prevention
Treatment depends on whether or not infection is involved, and the causes and symptoms. It is important to differentiate between infected and non-infected bursitis. People may have surrounding cellulitis and systemic symptoms include a fever. The bursa should be aspirated to rule out an infectious process (Vigorita 2015).
A common treatment is rest for the affected area, reducing swelling by ice, use of NSAIDs (nonsteroidal, anti-inflammatory drugs) to reduce inflammation and relieve pain, using a compression wrap to support and protect the bursa, elevating the affected area, and using topical pain relievers (NYPH 2007; Mayo 2007). Cortisone injections may be used, as well as physical therapy. In the case of infection, antibiotics may be used, and in worst case scenarios, surgical drainage and removal of the infected bursa (bursectomy) (NYPH 2007).
Prevention can be aided by regular stretching exercises, which can loosen the muscles and lengthen tendon connections around the bursa; relaxation techniques can also help reduce pressure on the bursa. Protective equipment, such as knee pads, can reduce injury and pressure on the joint area. Immediate treatment can reduce the risk of the bursitis becoming more severe.
ReferencesISBN links support NWE through referral fees
- Bursitis.org (BS). 2005. Bursitis. Retrieved April 8, 2025.
- Mayo Clinic. 2007. Bursitis. Retrieved April 8, 2025.
- New York-Presbyterian Hospital (NYPH). 2007. Bursitis. Retrieved April 8, 2025
- American Academy of Orthopaedic Surgeons (AAOS). 2025. Bursitis. Retrieved April 8, 2025.
- Vigorita, Vincent J. 2015. Orthopaedic Pathology Third Edition. Lippincott Williams & Wilkins. ISBN 978-1451192025
External links
All links retrieved April 8, 2025.
- Bursitis Cleveland Clinic
- Bursitis: Symptoms, Causes, and Treatment WebMD
- Bursitis Johns Hopkins Medicine
- Bursitis National Health Service UK (NHS)
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.