|
|
| (37 intermediate revisions by the same user not shown) |
| Line 1: |
Line 1: |
| − | | + | {{Images OK}}{{Submitted}}{{Approved}}{{Copyedited}} |
| | {{Infobox medical condition (new) | | {{Infobox medical condition (new) |
| | | name = Attention Deficit Hyperactivity Disorder | | | name = Attention Deficit Hyperactivity Disorder |
| Line 22: |
Line 22: |
| | }} | | }} |
| | | | |
| − | '''Attention deficit hyperactivity disorder''' ('''ADHD''') is a [[neurodevelopmental disorder]] characterized by [[executive dysfunction]] occasioning symptoms of [[inattention]], hyperactivity, [[impulsivity]] and [[emotional dysregulation]] that are excessive and pervasive, impairing in multiple contexts, and otherwise [[Developmental psychology|age-inappropriate]]. Although people with ADHD struggle to sustain attention on tasks that entail delayed rewards or consequences, they are often able to maintain an unusually prolonged and intense level of attention for tasks they do find interesting or rewarding; this is known as [[hyperfocus]]. | + | '''Attention deficit hyperactivity disorder''' ('''ADHD''') is a [[neurodevelopmental disorder]] characterized by [[executive dysfunction]] occasioning symptoms of [[inattention]], hyperactivity, [[impulsivity]] and [[emotional dysregulation]] that are excessive and pervasive, impairing in multiple contexts, and otherwise age-inappropriate. Although people with ADHD struggle to sustain attention on tasks that entail delayed rewards or consequences, they are often able to maintain an unusually prolonged and intense level of attention for tasks they do find interesting or rewarding; this is known as [[hyperfocus]]. |
| − | | + | {{toc}} |
| − | ADHD, its diagnosis, and its treatment have been considered controversial since the 1970s. ADHD was officially known as '''attention deficit disorder''' ('''ADD''') from 1980 to 1987; prior to the 1980s, it was known as '''hyperkinetic reaction of childhood'''. ADHD is now a well-validated clinical diagnosis in children and adults, and the debate in the scientific community mainly centers on how it is diagnosed and treated. ADHD management recommendations vary and usually involve some combination of medications, [[psychotherapy|counseling]], and lifestyle changes. | + | ADHD, its diagnosis, and its treatment have been considered controversial since the 1970s, with issues including over-diagnosis, use of stimulants as treatment for children, as well as disagreements on the nature of the disorder. ADHD is now a well-validated clinical diagnosis in children and adults, and the debate in the scientific community mainly centers on how it is diagnosed and treated. ADHD management recommendations usually involve some combination of medications, [[psychotherapy|counseling]], and lifestyle changes. For the majority of individuals, such treatment enables them to live productive and fulfilling lives. |
| | | | |
| | ==History== | | ==History== |
| Line 57: |
Line 57: |
| | ADHD is diagnosed by an assessment of a person's behavioral and mental development, including ruling out the effects of drugs, medications, and other medical or psychiatric problems as explanations for the symptoms. ADHD diagnosis often takes into account feedback from parents and teachers.<ref name="Lake2011"> Mina K. Dulcan, Rachel R. Ballard, Poonam Jha, and Julie M. Sadhu, ''Concise Guide to Child and Adolescent Psychiatry'' (American Psychiatric Publishing, 2017, ISBN 978-1615370788).</ref> | | ADHD is diagnosed by an assessment of a person's behavioral and mental development, including ruling out the effects of drugs, medications, and other medical or psychiatric problems as explanations for the symptoms. ADHD diagnosis often takes into account feedback from parents and teachers.<ref name="Lake2011"> Mina K. Dulcan, Rachel R. Ballard, Poonam Jha, and Julie M. Sadhu, ''Concise Guide to Child and Adolescent Psychiatry'' (American Psychiatric Publishing, 2017, ISBN 978-1615370788).</ref> |
| | | | |
| − | In North America and Australia, DSM-5 criteria are used for diagnosis, while European countries usually use the ICD-11. ADHD is alternately classified as [[neurodevelopmental disorder]]<ref> Caroline S. Clauss-Ehlers, ''Encyclopedia of Cross-Cultural School Psychology'' (Springer, 2010, ISBN 978-0387717982).</ref> or a [[disruptive behavior disorder]] along with [[Oppositional defiant disorder]] (ODD), [[Conduct disorder]] (CD), and [[antisocial personality disorder]].<ref> Jerry M. Wiener and Mina K. Dulcan (eds.), ''Textbook Of Child and Adolescent Psychiatry'' (American Psychiatric Publishing, 2003, ISBN 978-1585620579).</ref> | + | In North America and Australia, the [[American Psychiatric Association]]'s ''Diagnostic and Statistical Manual of Mental Disorders'' (currently DSM-5) criteria are used for diagnosis, while European countries usually use the [[World Health Organization]]'s ''International Classification of Diseases'' (currently ICD-11). ADHD is alternately classified as [[neurodevelopmental disorder]]<ref> Caroline S. Clauss-Ehlers, ''Encyclopedia of Cross-Cultural School Psychology'' (Springer, 2010, ISBN 978-0387717982).</ref> or a [[disruptive behavior disorder]] along with [[Oppositional defiant disorder]] (ODD), [[Conduct disorder]] (CD), and [[antisocial personality disorder]].<ref> Jerry M. Wiener and Mina K. Dulcan (eds.), ''Textbook Of Child and Adolescent Psychiatry'' (American Psychiatric Publishing, 2003, ISBN 978-1585620579).</ref> |
| | | | |
| | Self-rating scales, such as the [[ADHD rating scale]] and the [[Vanderbilt ADHD diagnostic rating scale]], are used in the screening and evaluation of ADHD.<ref> Eric A. Youngstrom, Mitchell J. Prinstein, Eric J. Mash, and Russell A. Barkley (eds.), ''Assessment of Disorders in Childhood and Adolescence'' (The Guilford Press, 2020, ISBN 978-1462543632).</ref> | | Self-rating scales, such as the [[ADHD rating scale]] and the [[Vanderbilt ADHD diagnostic rating scale]], are used in the screening and evaluation of ADHD.<ref> Eric A. Youngstrom, Mitchell J. Prinstein, Eric J. Mash, and Russell A. Barkley (eds.), ''Assessment of Disorders in Childhood and Adolescence'' (The Guilford Press, 2020, ISBN 978-1462543632).</ref> |
| Line 116: |
Line 116: |
| | |} | | |} |
| | | | |
| − | ====Diagnostic and Statistical Manual==== | + | ====DSM-5==== |
| | As with many other psychiatric disorders, a formal diagnosis should be made by a qualified professional based on a set number of criteria. In the United States, these criteria are defined by the [[American Psychiatric Association]] in the [[Diagnostic and Statistical Manual of Mental Disorders|DSM]]. Based on the DSM-5 criteria published in 2013 and the DSM-5-TR criteria published in 2022, there are three presentations of ADHD: | | As with many other psychiatric disorders, a formal diagnosis should be made by a qualified professional based on a set number of criteria. In the United States, these criteria are defined by the [[American Psychiatric Association]] in the [[Diagnostic and Statistical Manual of Mental Disorders|DSM]]. Based on the DSM-5 criteria published in 2013 and the DSM-5-TR criteria published in 2022, there are three presentations of ADHD: |
| | | | |
| Line 127: |
Line 127: |
| | The DSM-5 and the DSM-5-TR also provide two diagnoses for individuals who have symptoms of ADHD but do not entirely meet the requirements. ''Other Specified ADHD'' allows the clinician to describe why the individual does not meet the criteria, whereas ''Unspecified ADHD'' is used where the clinician chooses not to describe the reason. | | The DSM-5 and the DSM-5-TR also provide two diagnoses for individuals who have symptoms of ADHD but do not entirely meet the requirements. ''Other Specified ADHD'' allows the clinician to describe why the individual does not meet the criteria, whereas ''Unspecified ADHD'' is used where the clinician chooses not to describe the reason. |
| | | | |
| − | ====International Classification of Diseases==== | + | ====ICD-11==== |
| | In the eleventh revision of the [[World Health Organization]]'s ICD-11, the disorder is classified as Attention deficit hyperactivity disorder (code 6A05). The defined subtypes are similar to those of the DSM-5: ''predominantly inattentive presentation'' (6A05.0); ''predominantly hyperactive-impulsive presentation''(6A05.1); ''combined presentation'' (6A05.2). The ICD-11 also includes the two residual categories for individuals who do not entirely match any of the defined subtypes: ''other specified presentation'' (6A05.Y) where the clinician includes detail on the individual's presentation; and ''presentation unspecified'' (6A05.Z) where the clinician does not provide detail.<ref name="ICD-11"/> | | In the eleventh revision of the [[World Health Organization]]'s ICD-11, the disorder is classified as Attention deficit hyperactivity disorder (code 6A05). The defined subtypes are similar to those of the DSM-5: ''predominantly inattentive presentation'' (6A05.0); ''predominantly hyperactive-impulsive presentation''(6A05.1); ''combined presentation'' (6A05.2). The ICD-11 also includes the two residual categories for individuals who do not entirely match any of the defined subtypes: ''other specified presentation'' (6A05.Y) where the clinician includes detail on the individual's presentation; and ''presentation unspecified'' (6A05.Z) where the clinician does not provide detail.<ref name="ICD-11"/> |
| | | | |
| Line 146: |
Line 146: |
| | ADHD is often comorbid with disruptive, impulse control, and conduct disorders. [[Oppositional defiant disorder]] (ODD), characterized by angry or irritable mood, argumentative or defiant behavior and vindictiveness which are age-inappropriate, occurs in about 25 percent of children with an inattentive presentation and 50 percent of those with a combined presentation. [[Conduct disorder]] (CD), characterized by aggression, destruction of property, deceitfulness, theft and violations of rules, occurs in about 25 percent of adolescents with ADHD.<ref name=DSM5TR/> | | ADHD is often comorbid with disruptive, impulse control, and conduct disorders. [[Oppositional defiant disorder]] (ODD), characterized by angry or irritable mood, argumentative or defiant behavior and vindictiveness which are age-inappropriate, occurs in about 25 percent of children with an inattentive presentation and 50 percent of those with a combined presentation. [[Conduct disorder]] (CD), characterized by aggression, destruction of property, deceitfulness, theft and violations of rules, occurs in about 25 percent of adolescents with ADHD.<ref name=DSM5TR/> |
| | | | |
| − | [[Anxiety disorder]]s have been found to occur more commonly in the ADHD population, as have [[mood disorder]]s (especially [[bipolar disorder]] and [[major depressive disorder]]). Boys diagnosed with the combined ADHD subtype are more likely to have a mood disorder.<ref name="Wilens_2010">{{cite journal |vauthors=Wilens TE, Spencer TJ |title=Understanding attention-deficit/hyperactivity disorder from childhood to adulthood |journal=Postgraduate Medicine |volume=122 |issue=5 |pages=97–109 |date=September 2010 |pmid=20861593 |pmc=3724232 |doi=10.3810/pgm.2010.09.2206 }}</ref> Adults and children with ADHD sometimes also have bipolar disorder, which requires careful assessment to accurately diagnose and treat both conditions.<ref name="pmid21717696">{{cite journal |vauthors=Baud P, Perroud N, Aubry JM |title=[Bipolar disorder and attention deficit/hyperactivity disorder in adults: differential diagnosis or comorbidity] |language=fr |journal=Revue Médicale Suisse |volume=7 |issue=297 |pages=1219–1222 |date=June 2011 |pmid=21717696 }}</ref><ref name="Wilens_2011">{{cite journal |vauthors=Wilens TE, Morrison NR |title=The intersection of attention-deficit/hyperactivity disorder and substance abuse |journal=Current Opinion in Psychiatry |volume=24 |issue=4 |pages=280–285 |date=July 2011 |pmid=21483267 |pmc=3435098 |doi=10.1097/YCO.0b013e328345c956 }}</ref> | + | [[Anxiety disorder]]s have been found to occur more commonly in the ADHD population, as have [[mood disorder]]s (especially [[bipolar disorder]] and [[major depressive disorder]]). |
| | | | |
| − | [[Sleep disorders]] and ADHD commonly co-exist. They can also occur as a side effect of medications used to treat ADHD. In children with ADHD, [[insomnia]] is the most common sleep disorder with behavioural therapy being the preferred treatment.<ref name="pmid21600348">{{cite journal |vauthors=Corkum P, Davidson F, Macpherson M |title=A framework for the assessment and treatment of sleep problems in children with attention-deficit/hyperactivity disorder |journal=Pediatric Clinics of North America |volume=58 |issue=3 |pages=667–683 |date=June 2011 |pmid=21600348 |doi=10.1016/j.pcl.2011.03.004 }}</ref><ref name="pmid20451036">{{cite journal |vauthors=Tsai MH, Huang YS |title=Attention-deficit/hyperactivity disorder and sleep disorders in children |journal=The Medical Clinics of North America |volume=94 |issue=3 |pages=615–632 |date=May 2010 |pmid=20451036 |doi=10.1016/j.mcna.2010.03.008 }}</ref> Problems with sleep initiation are common among individuals with ADHD but often they will be deep sleepers and have significant difficulty getting up in the morning.<ref name="Brown_2008" /> [[Melatonin]] is sometimes used in children who have sleep onset insomnia.<ref name="pmid20028959">{{cite journal |vauthors=Bendz LM, Scates AC |title=Melatonin treatment for insomnia in pediatric patients with attention-deficit/hyperactivity disorder |journal=The Annals of Pharmacotherapy |volume=44 |issue=1 |pages=185–191 |date=January 2010 |pmid=20028959 |doi=10.1345/aph.1M365 |s2cid=207263711 }}</ref> Specifically, the sleep disorder [[restless legs syndrome]] has been found to be more common in those with ADHD and is often due to [[iron deficiency anemia]].<ref name="pmid21365608">{{cite journal |vauthors=Merino-Andreu M |title=[Attention deficit hyperactivity disorder and restless legs syndrome in children] |language=es |journal=Revista de Neurología |volume=52 |issue=Suppl 1 |pages=S85–S95 |date=March 2011 |pmid=21365608 |trans-title=Attention deficit hyperactivity disorder and restless legs syndrome in children |doi=10.33588/rn.52S01.2011037}}</ref><ref name="pmid20620105">{{cite journal |vauthors=Picchietti MA, Picchietti DL |title=Advances in pediatric restless legs syndrome: Iron, genetics, diagnosis and treatment |journal=Sleep Medicine |volume=11 |issue=7 |pages=643–651 |date=August 2010 |pmid=20620105 |doi=10.1016/j.sleep.2009.11.014 }}</ref> However, restless legs can simply be a part of ADHD and requires careful assessment to differentiate between the two disorders.<ref name="pmid18656214">{{cite journal |vauthors=Karroum E, Konofal E, Arnulf I |title=[Restless-legs syndrome] |language=fr |journal=Revue Neurologique |volume=164 |issue=8–9 |pages=701–721 |year=2008 |pmid=18656214 |doi=10.1016/j.neurol.2008.06.006 }}</ref> [[Delayed sleep phase disorder]] is also a common comorbidity of those with ADHD.<ref>{{cite journal |vauthors=Wajszilber D, Santiseban JA, Gruber R |title=Sleep disorders in patients with ADHD: impact and management challenges |journal=Nature and Science of Sleep |volume=10 |pages=453–480 |date=December 2018 |pmid=30588139 |pmc=6299464 |doi=10.2147/NSS.S163074 |doi-access=free }}</ref> | + | [[Sleep disorders]] and ADHD commonly co-exist. However, they can also occur as a side effect of medications used to treat ADHD. |
| | | | |
| − | There are other psychiatric conditions which are often co-morbid with ADHD, such as [[substance use disorder]]s.<ref>{{cite journal | vauthors = Long Y, Pan N, Ji S, Qin K, Chen Y, Zhang X, He M, Suo X, Yu Y, Wang S, Gong Q | display-authors = 6 | title = Distinct brain structural abnormalities in attention-deficit/hyperactivity disorder and substance use disorders: A comparative meta-analysis | journal = Translational Psychiatry | volume = 12 | issue = 1 | pages = 368 | date = September 2022 | pmid = 36068207 | pmc = 9448791 | doi = 10.1038/s41398-022-02130-6 }}</ref> Individuals with ADHD are at increased risk of [[substance abuse]].{{rp|9|quote=Comorbid substance use disorder (SUD) deserves special attention due to the high rates of ADHD within SUD populations. A bidirectional link between ADHD and SUD is reported with ADHD symptoms over represented in SUD populations and SUD in ADHD populations.}} This is most commonly seen with [[alcoholic beverage|alcohol]] or [[cannabis (drug)|cannabis]].<ref name="Kooij_2010" />{{rp|9|quote=Alcohol and cannabis are the most frequently abused substances in these populations followed by lower rates of cocaine and amphetamine abuse.}} The reason for this may be an altered reward pathway in the brains of ADHD individuals, self-treatment and increased psychosocial risk factors.{{rp|9|quote=The causes for such comorbidity are likely to be complex including altered reward processing in ADHD, increased exposure to psychosocial risk factors and self treatment. }} This makes the evaluation and treatment of ADHD more difficult, with serious substance misuse problems usually treated first due to their greater risks.<ref name="NICE2009-part2">{{cite book |author=National Collaborating Centre for Mental Health |title=Attention Deficit Hyperactivity Disorder: Diagnosis and Management of ADHD in Children, Young People and Adults |date=2009 |url=https://www.ncbi.nlm.nih.gov/books/NBK53652/ |publisher=British Psychological Society |isbn=978-1-85433-471-8 |series=NICE Clinical Guidelines |volume=72 |location=Leicester |pages=[https://www.ncbi.nlm.nih.gov/books/NBK53663/#ch2.s8 18–26], [https://www.ncbi.nlm.nih.gov/books/NBK53663/#ch2.s41 38] |chapter=Attention Deficit Hyperactivity Disorder |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK53663/ |url-status=live |archive-date=13 January 2016 |archive-url=https://web.archive.org/web/20160113133612/http://www.ncbi.nlm.nih.gov/books/NBK53652/ |via=NCBI Bookshelf}}</ref> Other psychiatric conditions include [[reactive attachment disorder]],<ref>{{cite journal | vauthors = Storebø OJ, Rasmussen PD, Simonsen E | title = Association Between Insecure Attachment and ADHD: Environmental Mediating Factors | journal = Journal of Attention Disorders | volume = 20 | issue = 2 | pages = 187–196 | date = February 2016 | pmid = 24062279 | doi = 10.1177/1087054713501079 | url = https://findresearcher.sdu.dk:8443/ws/files/134088245/Association_Between_Insecure_Attachment_and_ADHD.pdf | access-date = 22 November 2021 | url-status = live | s2cid = 23564305 | archive-url = https://web.archive.org/web/20211209135025/https://findresearcher.sdu.dk:8443/ws/files/134088245/Association_Between_Insecure_Attachment_and_ADHD.pdf | archive-date = 9 December 2021 }}</ref> characterised by a severe inability to appropriately relate socially, and [[sluggish cognitive tempo]], a cluster of symptoms that potentially comprises another attention disorder and may occur in 30–50% of ADHD cases, regardless of the subtype.<ref>{{cite journal | vauthors = Barkley RA | title = Sluggish cognitive tempo (concentration deficit disorder?): current status, future directions, and a plea to change the name | journal = Journal of Abnormal Child Psychology | volume = 42 | issue = 1 | pages = 117–125 | date = January 2014 | pmid = 24234590 | doi = 10.1007/s10802-013-9824-y | url = https://psychology.uiowa.edu/sites/psychology.uiowa.edu/files/groups/nikolas/files/Barkley,%202014.pdf | url-status = live | s2cid = 8287560 | author-link = Russell Barkley | archive-url = https://web.archive.org/web/20170809102631/https://psychology.uiowa.edu/sites/psychology.uiowa.edu/files/groups/nikolas/files/Barkley,%202014.pdf | archive-date = 9 August 2017 }}</ref> Individuals with ADHD are three times more likely to develop and be diagnosed with an [[eating disorder]] compared to those without ADHD; conversely, individuals with eating disorders are two times more likely to have ADHD than those without eating disorders.<ref name="Nazar_2016">{{cite journal | vauthors = Nazar BP, Bernardes C, Peachey G, Sergeant J, Mattos P, Treasure J | title = The risk of eating disorders comorbid with attention-deficit/hyperactivity disorder: A systematic review and meta-analysis | journal = The International Journal of Eating Disorders | volume = 49 | issue = 12 | pages = 1045–1057 | date = December 2016 | pmid = 27859581 | doi = 10.1002/eat.22643 | s2cid = 38002526 | url = https://kclpure.kcl.ac.uk/portal/en/publications/the-risk-of-eating-disorders-comorbid-with-attentiondeficithyperactivity-disorder(9a8e868e-de6e-4e19-9561-f8a576836848).html | access-date = 26 October 2022 | archive-date = 8 December 2022 | archive-url = https://web.archive.org/web/20221208035350/https://kclpure.kcl.ac.uk/portal/en/publications/the-risk-of-eating-disorders-comorbid-with-attentiondeficithyperactivity-disorder(9a8e868e-de6e-4e19-9561-f8a576836848).html | url-status = live }}</ref> | + | There are other psychiatric conditions which are often co-morbid with ADHD, such as [[substance use disorder]]s, commonly seen with [[alcoholic beverage|alcohol]] or [[cannabis (drug)|cannabis]].<ref name="Kooij_2010" /> Other psychiatric conditions include [[reactive attachment disorder]] and [[eating disorder]]s. |
| | | | |
| | ===Trauma=== | | ===Trauma=== |
| − | ADHD, [[Psychological trauma|trauma]], and [[Adverse childhood experiences|Adverse Childhood Experiences]] are also comorbid,<ref>{{cite journal | vauthors = Schneider M, VanOrmer J, Zlomke K | title = Adverse Childhood Experiences and Family Resilience Among Children with Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder | journal = Journal of Developmental and Behavioral Pediatrics | volume = 40 | issue = 8 | pages = 573–580 | date = 2019 | pmid = 31335581 | doi = 10.1097/DBP.0000000000000703 | s2cid = 198193637 }}</ref><ref>{{cite journal | vauthors = Moon DS, Bong SJ, Kim BN, Kang NR | title = Association between Maternal Adverse Childhood Experiences and Attention-Deficit/Hyperactivity Disorder in the Offspring: The Mediating Role of Antepartum Health Risks | journal = Soa—Ch'ongsonyon Chongsin Uihak = Journal of Child & Adolescent Psychiatry | volume = 32 | issue = 1 | pages = 28–34 | date = January 2021 | pmid = 33424239 | pmc = 7788667 | doi = 10.5765/jkacap.200041 }}</ref> which could in part be potentially explained by the similarity in presentation between different diagnoses. The symptoms of ADHD and [[Post-traumatic stress disorder|PTSD]] can have significant behavioural overlap—in particular, motor restlessness, difficulty concentrating, distractibility, irritability/anger, emotional constriction or dysregulation, poor impulse control, and forgetfulness are common in both.<ref name="Ford_2009">{{Cite journal |vauthors=Ford JD, Connor DF |date=1 June 2009 |title=ADHD and post-traumatic stress disorder |journal=Current Attention Disorders Reports |language=en |volume=1 |issue=2 |pages=60–66 |doi=10.1007/s12618-009-0009-0 |issn=1943-457X |s2cid=145508751}}</ref><ref>{{cite journal | vauthors = Harrington KM, Miller MW, Wolf EJ, Reardon AF, Ryabchenko KA, Ofrat S | title = Attention-deficit/hyperactivity disorder comorbidity in a sample of veterans with posttraumatic stress disorder | journal = Comprehensive Psychiatry | volume = 53 | issue = 6 | pages = 679–690 | date = August 2012 | pmid = 22305866 | pmc = 6519447 | doi = 10.1016/j.comppsych.2011.12.001 }}</ref> This could result in trauma-related disorders or ADHD being mis-identified as the other.<ref name="Szymanski_2011">{{Cite journal |vauthors=Szymanski K, Sapanski L, Conway F |date=1 January 2011 |title=Trauma and ADHD – Association or Diagnostic Confusion? A Clinical Perspective |journal=Journal of Infant, Child, and Adolescent Psychotherapy |location=Philadelphia PA |publisher=Taylor & Francis Group |volume=10 |issue=1 |pages=51–59 |doi=10.1080/15289168.2011.575704 |issn=1528-9168 |eissn=1940-9214 |s2cid=144348893}}</ref> Additionally, traumatic events in childhood are a risk factor for ADHD<ref>{{cite journal | vauthors = Zhang N, Gao M, Yu J, Zhang Q, Wang W, Zhou C, Liu L, Sun T, Liao X, Wang J | display-authors = 6 | title = Understanding the association between adverse childhood experiences and subsequent attention deficit hyperactivity disorder: A systematic review and meta-analysis of observational studies | journal = Brain and Behavior | volume = 12 | issue = 10 | pages = e32748 | date = October 2022 | pmid = 36068993 | pmc = 9575611 | doi = 10.1002/brb3.2748 }}</ref><ref>{{cite journal | vauthors = Nguyen MN, Watanabe-Galloway S, Hill JL, Siahpush M, Tibbits MK, Wichman C | title = Ecological model of school engagement and attention-deficit/hyperactivity disorder in school-aged children | journal = European Child & Adolescent Psychiatry | volume = 28 | issue = 6 | pages = 795–805 | date = June 2019 | pmid = 30390147 | doi = 10.1007/s00787-018-1248-3 | s2cid = 53263217 }}</ref> - it can lead to structural brain changes and the development of ADHD behaviours.<ref name="Szymanski_2011"/> Finally, the behavioural consequences of ADHD symptoms cause a higher chance of the individual experiencing trauma (and therefore ADHD leads to a concrete diagnosis of a trauma-related disorder).<ref>{{Cite journal | vauthors = Miodus S, Allwood MA, Amoh N |date=5 January 2021 |title=Childhood ADHD Symptoms in Relation to Trauma Exposure and PTSD Symptoms Among College Students: Attending to and Accommodating Trauma |journal=Journal of Emotional and Behavioral Disorders |language=en |volume=29 |issue=3 |pages=187–196 |doi=10.1177/1063426620982624 |s2cid=234159064 |issn=1063-4266 }}</ref>{{Primary source inline|date=January 2023}} | + | ADHD, [[Psychological trauma|trauma]], and [[Adverse childhood experiences|Adverse Childhood Experiences]] are also comorbid, which could in part be potentially explained by the similarity in presentation between different diagnoses. The symptoms of ADHD and [[Post-traumatic stress disorder|PTSD]] can have significant behavioral overlap—in particular, motor restlessness, difficulty concentrating, distractibility, irritability/anger, emotional constriction or dysregulation, poor impulse control, and forgetfulness are common in both. |
| | | | |
| | ===Non-psychiatric=== | | ===Non-psychiatric=== |
| − | Some non-psychiatric conditions are also comorbidities of ADHD. This includes [[epilepsy]],<ref name="NHS2018">{{cite web |title=ADHD Symptoms |url=https://www.nhs.uk/conditions/attention-deficit-hyperactivity-disorder-adhd/symptoms/#related-conditions-in-children-and-teenagers |website=nhs.uk |access-date=15 May 2018 |date=20 October 2017 |archive-date=1 February 2021 |archive-url=https://web.archive.org/web/20210201015023/https://www.nhs.uk/conditions/attention-deficit-hyperactivity-disorder-adhd/symptoms/#related-conditions-in-children-and-teenagers |url-status=live }}</ref> a neurological condition characterised by recurrent seizures.<ref>{{cite journal | vauthors = Williams AE, Giust JM, Kronenberger WG, Dunn DW | title = Epilepsy and attention-deficit hyperactivity disorder: links, risks, and challenges | journal = Neuropsychiatric Disease and Treatment | volume = 12 | pages = 287–296 | date = 2016 | pmid = 26929624 | pmc = 4755462 | doi = 10.2147/NDT.S81549 | doi-access = free }}</ref><ref>{{cite journal | vauthors = Silva RR, Munoz DM, Alpert M | title = Carbamazepine use in children and adolescents with features of attention-deficit hyperactivity disorder: a meta-analysis | journal = Journal of the American Academy of Child and Adolescent Psychiatry | volume = 35 | issue = 3 | pages = 352–358 | date = March 1996 | pmid = 8714324 | doi = 10.1097/00004583-199603000-00017 | doi-access = free }}</ref> There are well established associations between ADHD and obesity, [[asthma]] and sleep disorders,<ref name="pmid27664125">{{cite journal |vauthors=Instanes JT, Klungsøyr K, Halmøy A, Fasmer OB, Haavik J |date=February 2018 |title=Adult ADHD and Comorbid Somatic Disease: A Systematic Literature Review |journal=Journal of Attention Disorders |type=Systematic Review |volume=22 |issue=3 |pages=203–228 |doi=10.1177/1087054716669589 |pmc=5987989 |pmid=27664125}}</ref> and an association with celiac disease.<ref>{{cite journal | vauthors = Gaur S | title = The Association between ADHD and Celiac Disease in Children | journal = Children | volume = 9 | issue = 6 | page = 781 | date = May 2022 | pmid = 35740718 | pmc = 9221618 | doi = 10.3390/children9060781 | publisher = MDPI | doi-access = free }}</ref> Children with ADHD have a higher risk for [[migraine]] headaches,<ref>{{cite journal | vauthors = Hsu TW, Chen MH, Chu CS, Tsai SJ, Bai YM, Su TP, Chen TJ, Liang CS | display-authors = 6 | title = Attention deficit hyperactivity disorder and risk of migraine: A nationwide longitudinal study | journal = Headache | volume = 62 | issue = 5 | pages = 634–641 | date = May 2022 | pmid = 35524451 | doi = 10.1111/head.14306 | s2cid = 248553863 }}</ref> but have no increased risk of tension-type headaches. In addition, children with ADHD may also experience headaches as a result of medication.<ref name="Salem_2017">{{cite journal |vauthors=Salem H, Vivas D, Cao F, Kazimi IF, Teixeira AL, Zeni CP |date=March 2018 |title=ADHD is associated with migraine: a systematic review and meta-analysis |journal=European Child & Adolescent Psychiatry |publisher=Springer Science and Business Media LLC |volume=27 |issue=3 |pages=267–277 |doi=10.1007/s00787-017-1045-4 |pmid=28905127 |s2cid=3949012}}</ref><ref name="Pan_2021">{{cite journal |display-authors=6 |vauthors=Pan PY, Jonsson U, Şahpazoğlu Çakmak SS, Häge A, Hohmann S, Nobel Norrman H, Buitelaar JK, Banaschewski T, Cortese S, Coghill D, Bölte S |date=January 2022 |title=Headache in ADHD as comorbidity and a side effect of medications: a systematic review and meta-analysis |journal=Psychological Medicine |publisher=Cambridge University Press |volume=52 |issue=1 |pages=14–25 |doi=10.1017/s0033291721004141 |pmc=8711104 |pmid=34635194 |doi-access=free}}</ref> | + | Some non-psychiatric conditions are also comorbidities of ADHD. This includes [[epilepsy]], a neurological condition characterized by recurrent seizures. There are well established associations between ADHD and obesity, [[asthma]] and sleep disorders. Children with ADHD have a higher risk for [[migraine]] headaches, but have no increased risk of tension-type headaches. In addition, children with ADHD may also experience headaches as a result of medication. |
| − | | |
| − | A 2021 review reported that several neurometabolic disorders caused by [[inborn errors of metabolism]] converge on common neurochemical mechanisms that interfere with biological mechanisms also considered central in ADHD pathophysiology and treatment. This highlights the importance of close collaboration between health services to avoid clinical overshadowing.<ref>{{cite journal |vauthors=Cannon Homaei S, Barone H, Kleppe R, Betari N, Reif A, Haavik J |title=ADHD symptoms in neurometabolic diseases: Underlying mechanisms and clinical implications |journal=Neuroscience and Biobehavioral Reviews |date=November 2021 |volume=132 |pages=838–856 |pmid=34774900 |doi=10.1016/j.neubiorev.2021.11.012 |issn=0149-7634 |s2cid=243983688 |doi-access=free }}</ref>
| |
| | | | |
| | ===Suicide risk=== | | ===Suicide risk=== |
| − | Systematic reviews conducted in 2017 and 2020 found strong evidence that ADHD is associated with increased [[suicide]] risk across all age groups, as well as growing evidence that an ADHD diagnosis in childhood or adolescence represents a significant future suicidal risk factor.<ref>{{cite journal |vauthors=Balazs J, Kereszteny A |title=Attention-deficit/hyperactivity disorder and suicide: A systematic review |journal=World Journal of Psychiatry |volume=7 |issue=1 |pages=44–59 |date=March 2017 |pmid=28401048 |pmc=5371172 |doi=10.5498/wjp.v7.i1.44 |doi-access=free }}</ref><ref name="Garas_2020">{{cite journal |vauthors=Garas P, Balazs J |title=Long-Term Suicide Risk of Children and Adolescents With Attention Deficit and Hyperactivity Disorder-A Systematic Review |journal=Frontiers in Psychiatry |volume=11 |page=557909 |date=21 December 2020 |pmid=33408650 |pmc=7779592 |doi=10.3389/fpsyt.2020.557909 |doi-access=free |id=557909 }}</ref> Potential causes include ADHD's association with functional impairment, negative social, educational and occupational outcomes, and financial distress.<ref name="Septier_2019">{{cite journal |vauthors=Septier M, Stordeur C, Zhang J, Delorme R, Cortese S |title=Association between suicidal spectrum behaviors and Attention-Deficit/Hyperactivity Disorder: A systematic review and meta-analysis |journal=Neuroscience and Biobehavioral Reviews |volume=103 |pages=109–118 |date=August 2019 |pmid=31129238 |doi=10.1016/j.neubiorev.2019.05.022 |s2cid=162184004 |url=https://eprints.soton.ac.uk/431399/1/Septier_et_al_ADHD_SUICIDE_R2_CLEANED.docx |access-date=7 December 2021 |archive-date=4 November 2021 |archive-url=https://web.archive.org/web/20211104140233/https://eprints.soton.ac.uk/431399/1/Septier_et_al_ADHD_SUICIDE_R2_CLEANED.docx |url-status=live }}</ref><ref>{{cite journal |vauthors=Beauchaine TP, Ben-David I, Bos M |title=ADHD, financial distress, and suicide in adulthood: A population study |journal=Science Advances |volume=6 |issue=40 |pages=eaba1551 |date=September 2020 |pmid=32998893 |pmc=7527218 |doi=10.1126/sciadv.aba1551 |id=eaba1551 |bibcode=2020SciA....6.1551B }}</ref> A 2019 meta-analysis indicated a significant association between ADHD and suicidal spectrum behaviours (suicidal attempts, ideations, plans, and completed suicides); across the studies examined, the prevalence of suicide attempts in individuals with ADHD was 18.9%, compared to 9.3% in individuals without ADHD, and the findings were substantially replicated among studies which adjusted for other variables. However, the relationship between ADHD and suicidal spectrum behaviours remains unclear due to mixed findings across individual studies and the complicating impact of comorbid psychiatric disorders.<ref name="Septier_2019" /> There is no clear data on whether there is a direct relationship between ADHD and suicidality, or whether ADHD increases suicide risk through comorbidities.<ref name="Garas_2020" /> | + | Systematic reviews conducted in 2017 and 2020 found strong evidence that ADHD is associated with increased [[suicide]] risk across all age groups, as well as growing evidence that an ADHD diagnosis in childhood or adolescence represents a significant future suicidal risk factor. However, the relationship between ADHD and suicidal spectrum behaviors remains unclear. There is no clear data on whether there is a direct relationship between ADHD and suicidality, or whether ADHD increases suicide risk through comorbidities.<ref>P. Garas and J. Balazs, Long-Term Suicide Risk of Children and Adolescents With Attention Deficit and Hyperactivity Disorder-A Systematic Review, ''Frontiers in Psychiatry'' 11 (December 21, 2020):557909.</ref> |
| | | | |
| | ==Causes== | | ==Causes== |
| − | The precise causes of ADHD are unknown in the majority of cases.<ref name=nimh/><ref>{{cite journal | vauthors = Franke B, Michelini G, Asherson P, Banaschewski T, Bilbow A, Buitelaar JK, Cormand B, Faraone SV, Ginsberg Y, Haavik J, Kuntsi J, Larsson H, Lesch KP, Ramos-Quiroga JA, Réthelyi JM, Ribases M, Reif A | display-authors = 6 | title = Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan | journal = European Neuropsychopharmacology | volume = 28 | issue = 10 | pages = 1059–1088 | date = October 2018 | pmid = 30195575 | pmc = 6379245 | doi = 10.1016/j.euroneuro.2018.08.001 }}</ref> For most people with ADHD, many genetic and environmental risk factors accumulate to cause the disorder. The environmental risks for ADHD most often exert their influence in the early prenatal period. In some cases a single event might cause ADHD such as traumatic brain injury, exposure to biohazards during pregnancy, a major genetic mutation or extreme nutritional deprivation early in life. Later in life, there is no biologically distinct adult onset ADHD except for when ADHD occurs after traumatic brain injury.<ref>{{Cite journal |last1=Faraone |first1=Stephen V. |last2=Banaschewski |first2=Tobias |last3=Coghill |first3=David |last4=Zheng |first4=Yi |last5=Biederman |first5=Joseph |last6=Bellgrove |first6=Mark A. |last7=Newcorn |first7=Jeffrey H. |last8=Gignac |first8=Martin |last9=Al Saud |first9=Nouf M. |last10=Manor |first10=Iris |last11=Rohde |first11=Luis Augusto |last12=Yang |first12=Li |last13=Cortese |first13=Samuele |last14=Almagor |first14=Doron |last15=Stein |first15=Mark A. |date=2021-09-01 |title=The World Federation of ADHD International Consensus Statement: 208 Evidence-based conclusions about the disorder |journal=Neuroscience & Biobehavioral Reviews |volume=128 |pages=789–818 |doi=10.1016/j.neubiorev.2021.01.022 |pmid=33549739 |pmc=8328933 |issn=0149-7634}}</ref> | + | The precise causes of ADHD are unknown in the majority of cases. For most people with ADHD, many genetic and environmental risk factors accumulate to cause the disorder. The environmental risks for ADHD most often exert their influence in the early prenatal period. |
| | | | |
| | === Genetics === | | === Genetics === |
| − | A [[Family study|family]], twin, and [[Adoption study|adoption studies]] literature review published in ''[[Molecular Psychiatry]]'' in April 2019 by psychologists [[Stephen Faraone]] and Henrik Larsson that found an average heritability estimate of 0.74 for ADHD.<ref>{{cite journal|last1=Faraone|first1=Stephen V.|author-link1=Stephen Faraone |last2=Larsson |first2=Henrik |year=2019 |title=Genetics of attention deficit hyperactivity disorder|journal=[[Molecular Psychiatry]] |publisher=[[Nature Research]] |volume=24 |issue=4 |pages=562–575 |doi=10.1038/s41380-018-0070-0 |pmid=29892054 |pmc=6477889}}</ref> Additionally, [[Evolutionary psychiatry|evolutionary psychiatrist]] [[Randolph M. Nesse]] has argued that the 5:1 [[Sex differences in psychology|male-to-female sex ratio]] in the [[Mental disorders and gender|epidemiology of ADHD]] suggests that ADHD may be the [[Variability hypothesis|end of a continuum where males are overrepresented at the tails]], citing clinical psychologist [[Simon Baron-Cohen]]'s [[Empathising–systemising theory|suggestion]] for the [[Sex differences in autism|sex ratio in the epidemiology of autism]] as an analogue.<ref name="Baron-Cohen 2002">{{cite journal |last=Baron-Cohen|first=Simon|author-link=Simon Baron-Cohen|title=The extreme male brain theory of autism |year=2002|journal=[[Trends in Cognitive Sciences]]|publisher=[[Elsevier]]|volume=6|issue=6|pages=248–254|doi=10.1016/S1364-6613(02)01904-6 |pmid=12039606 |s2cid=8098723 |url=https://www.cell.com/trends/cognitive-sciences/fulltext/S1364-6613(02)01904-6|access-date=9 July 2020 |archive-date=3 July 2013 |archive-url=https://web.archive.org/web/20130703172532/http://www.cell.com/trends/cognitive-sciences/fulltext/S1364-6613(02)01904-6|url-status=live}}</ref><ref name="Nesse 2005 p. 918">{{cite book|last1=Nesse|first1=Randolph M. |author-link1=Randolph M. Nesse |editor-last=Buss |editor-first=David M.|editor-link=David Buss|title=The Handbook of Evolutionary Psychology |chapter=32. Evolutionary Psychology and Mental Health |page=918 |year=2005 |edition=1st |place=[[Hoboken, New Jersey|Hoboken, NJ]] |publisher=[[Wiley (publisher)|Wiley]] |isbn=978-0471264033}}</ref><ref name="Nesse 2016 p. 1019">{{cite book |last1=Nesse |first1=Randolph M. |author-link1=Randolph M. Nesse |editor-last1=Buss |editor-first1=David M. |editor-link1=David Buss |year=2016 |orig-date=2005 |title=The Handbook of Evolutionary Psychology, Volume 2: Integrations |edition=2nd |chapter=43. Evolutionary Psychology and Mental Health |page=1019 |place=[[Hoboken, New Jersey|Hoboken, NJ]] |publisher=[[Wiley (publisher)|Wiley]] |isbn=978-1118755808}}</ref>
| + | Family, twin, and adoption studies show that ADHD runs in families, with an average heritability of 74 percent.<ref name=Faraone>Stephen V. Faraone and Henrik Larsson, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6477889/ Genetics of attention deficit hyperactivity disorder] ''Molecular Psychiatry'' 24(4) (2019):562–575. Retrieved January 22, 2024.</ref> The siblings of children with ADHD are three to four times more likely to develop the disorder than siblings of children without the disorder.<ref>Susan Nolen-Hoeksema, ''Abnormal Psychology'' (McGraw Hill, 2022, ISBN 978-1265237769).</ref> |
| | | | |
| − | There are multiple gene variants which each slightly increase the likelihood of a person having ADHD; it is [[polygenic disease|polygenic]] and arises through the combination of many gene variants which each have a small effect.<ref name="Faraone_2018">{{cite journal |vauthors=Faraone SV, Larsson H |date=April 2019 |title=Genetics of attention deficit hyperactivity disorder |journal=Molecular Psychiatry |publisher=Springer Science and Business Media LLC |volume=24 |issue=4 |pages=562–575 |doi=10.1038/s41380-018-0070-0 |pmc=6477889 |pmid=29892054}}</ref><ref name="Faraone_2021">{{cite journal |vauthors=Faraone SV, Banaschewski T, Coghill D, Zheng Y, Biederman J, Bellgrove MA, Newcorn JH, Gignac M, Al Saud NM, Manor I, Rohde LA, Yang L, Cortese S, Almagor D, Stein MA, Albatti TH, Aljoudi HF, Alqahtani MM, Asherson P, Atwoli L, Bölte S, Buitelaar JK, Crunelle CL, Daley D, Dalsgaard S, Döpfner M, Espinet S, Fitzgerald M, Franke B, Gerlach M, Haavik J, Hartman CA, Hartung CM, Hinshaw SP, Hoekstra PJ, Hollis C, Kollins SH, Sandra Kooij JJ, Kuntsi J, Larsson H, Li T, Liu J, Merzon E, Mattingly G, Mattos P, McCarthy S, Mikami AY, Molina BS, Nigg JT, Purper-Ouakil D, Omigbodun OO, Polanczyk GV, Pollak Y, Poulton AS, Rajkumar RP, Reding A, Reif A, Rubia K, Rucklidge J, Romanos M, Ramos-Quiroga JA, Schellekens A, Scheres A, Schoeman R, Schweitzer JB, Shah H, Solanto MV, Sonuga-Barke E, Soutullo C, Steinhausen HC, Swanson JM, Thapar A, Tripp G, van de Glind G, van den Brink W, Van der Oord S, Venter A, Vitiello B, Walitza S, Wang Y |display-authors=6 |title=The World Federation of ADHD International Consensus Statement: 208 Evidence-based conclusions about the disorder |journal=Neuroscience and Biobehavioral Reviews |volume=128 |pages=789–818 |date=September 2021 |pmid=33549739 |pmc=8328933 |doi=10.1016/j.neubiorev.2021.01.022 |publisher=Elsevier BV |doi-access=free}}</ref> The siblings of children with ADHD are three to four times more likely to develop the disorder than siblings of children without the disorder.<ref>{{cite book |vauthors=Nolen-Hoeksema S |title=Abnormal Psychology |year=2013 |isbn=978-0-07-803538-8 |page=267 |publisher=McGraw-Hill Education |edition=6th}}</ref> | + | There are multiple gene variants which each slightly increase the likelihood of a person having ADHD; it is [[polygenic disease|polygenic]] and arises through the combination of many gene variants which each have a small effect.<ref name=Faraone/> |
| | | | |
| | For [[genetic variation]] to be used as a tool for diagnosis, more validating studies need to be performed. | | For [[genetic variation]] to be used as a tool for diagnosis, more validating studies need to be performed. |
| | | | |
| | === Environment === | | === Environment === |
| − | {{See also|Digital media use and mental health#ADHD}}
| + | In addition to genetics, environmental factors might play a role in ADHD development.causing ADHD.<ref>[https://www.cdc.gov/ncbddd/adhd/research.html Research on ADHD] ''Centers for Disease Control and Prevention''. Retrieved January 22, 2024.</ref> |
| − | | |
| − | In addition to genetics, some environmental factors might play a role in causing ADHD.<ref name="Sonu_2013" /><ref name="cdc2016">{{cite web |author=CDC |title=Attention-Deficit / Hyperactivity Disorder (ADHD) |publisher=Centers for Disease Control and Prevention |url=https://www.cdc.gov/ncbddd/adhd/research.html |date=16 March 2016 |access-date=17 April 2016 |url-status=live |archive-date=14 April 2016 |archive-url=https://web.archive.org/web/20160414160548/http://www.cdc.gov/ncbddd/adhd/research.html}}</ref> Alcohol intake during pregnancy can cause [[fetal alcohol spectrum disorder]]s which can include ADHD or symptoms like it.<ref name="Burger_2011">{{cite journal |vauthors=Burger PH, Goecke TW, Fasching PA, Moll G, Heinrich H, Beckmann MW, Kornhuber J |title=Einfluss des mütterlichen Alkoholkonsums während der Schwangerschaft auf die Entwicklung von ADHS beim Kind |trans-title=How does maternal alcohol consumption during pregnancy affect the development of attention deficit/hyperactivity syndrome in the child |language=de |journal=Fortschritte der Neurologie-Psychiatrie |volume=79 |issue=9 |pages=500–506 |date=September 2011 |pmid=21739408 |doi=10.1055/s-0031-1273360 |s2cid=140766296 |type=Review }}</ref> Children exposed to certain toxic substances, such as [[lead]] or [[polychlorinated biphenyls]], may develop problems which resemble ADHD.<ref name="nimh" /><ref name="Eubig_2010">{{cite journal |vauthors=Eubig PA, Aguiar A, Schantz SL |title=Lead and PCBs as risk factors for attention deficit/hyperactivity disorder |journal=Environmental Health Perspectives |volume=118 |issue=12 |pages=1654–1667 |date=December 2010 |pmid=20829149 |pmc=3002184 |doi=10.1289/ehp.0901852 |type=Review. Research Support, N.I.H., Extramural. Research Support, U.S. Gov't, Non-P.H.S. }}</ref> Exposure to the [[organophosphate]] insecticides [[chlorpyrifos]] and [[Alkyl phosphate|dialkyl phosphate]] is associated with an increased risk; however, the evidence is not conclusive.<ref name="de_Cock_2012">{{cite journal |vauthors=de Cock M, Maas YG, van de Bor M |title=Does perinatal exposure to endocrine disruptors induce autism spectrum and attention deficit hyperactivity disorders? Review |journal=Acta Paediatrica |volume=101 |issue=8 |pages=811–818 |date=August 2012 |pmid=22458970 |doi=10.1111/j.1651-2227.2012.02693.x |type=Review. Research Support, Non-U.S. Gov't |s2cid=41748237 }}</ref> Exposure to tobacco smoke during pregnancy can cause problems with central nervous system development and can increase the risk of ADHD.<ref name="nimh">{{cite web |title=Attention Deficit Hyperactivity Disorder (Easy-to-Read) |url=http://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder-easy-to-read/index.shtml |publisher=National Institute of Mental Health |year=2013 |access-date=17 April 2016 |url-status=live |archive-date=14 April 2016 |archive-url=https://web.archive.org/web/20160414031036/http://www.nimh.nih.gov/health/publications/attention-deficit-hyperactivity-disorder-easy-to-read/index.shtml}}</ref><ref name="Abbott_2012">{{cite journal |vauthors=Abbott LC, Winzer-Serhan UH |title=Smoking during pregnancy: lessons learned from epidemiological studies and experimental studies using animal models |journal=Critical Reviews in Toxicology |volume=42 |issue=4 |pages=279–303 |date=April 2012 |pmid=22394313 |doi=10.3109/10408444.2012.658506 |type=Review |s2cid=38886526 }}</ref> [[Nicotine]] exposure during pregnancy may be an environmental risk.<ref>{{cite journal |vauthors=Tiesler CM, Heinrich J |title=Prenatal nicotine exposure and child behavioural problems |journal=European Child & Adolescent Psychiatry |volume=23 |issue=10 |pages=913–929 |date=October 2014 |pmid=25241028 |pmc=4186967 |doi=10.1007/s00787-014-0615-y }}</ref> | |
| − | | |
| − | Extreme [[premature birth]], very [[low birth weight]], and extreme neglect, abuse, or social deprivation also increase the risk<ref>{{cite journal | vauthors = Botting N, Powls A, Cooke RW, Marlow N | title = Attention deficit hyperactivity disorders and other psychiatric outcomes in very low birthweight children at 12 years | journal = Journal of Child Psychology and Psychiatry, and Allied Disciplines | volume = 38 | issue = 8 | pages = 931–941 | date = November 1997 | pmid = 9413793 | doi = 10.1111/j.1469-7610.1997.tb01612.x | url = https://onlinelibrary.wiley.com/doi/10.1111/j.1469-7610.1997.tb01612.x | access-date = 22 March 2022 | url-status = live | archive-url = https://web.archive.org/web/20220517212252/https://onlinelibrary.wiley.com/doi/10.1111/j.1469-7610.1997.tb01612.x | archive-date = 17 May 2022 }}</ref><ref name="nimh" /><ref name="Thapar-2012">{{cite journal | vauthors = Thapar A, Cooper M, Jefferies R, Stergiakouli E | title = What causes attention deficit hyperactivity disorder? | journal = Archives of Disease in Childhood | volume = 97 | issue = 3 | pages = 260–265 | date = March 2012 | pmid = 21903599 | pmc = 3927422 | doi = 10.1136/archdischild-2011-300482 | type = Review. Research Support, Non-U.S. Gov't }}</ref> as do certain infections during pregnancy, at birth, and in early childhood. These infections include, among others, various viruses ([[measles]], [[Varicella zoster virus|varicella zoster]] [[encephalitis]], [[rubella]], [[enterovirus 71]]).<ref name="Millichap_2008">{{cite journal | vauthors = Millichap JG | title = Etiologic classification of attention-deficit/hyperactivity disorder | journal = Pediatrics | volume = 121 | issue = 2 | pages = e358–e365 | date = February 2008 | pmid = 18245408 | doi = 10.1542/peds.2007-1332 | type = Review | s2cid = 24339363 }}</ref> At least 30% of children with a [[traumatic brain injury]] later develop ADHD<ref name="Eme-2012">{{cite journal | vauthors = Eme R | title = ADHD: an integration with pediatric traumatic brain injury | journal = Expert Review of Neurotherapeutics | volume = 12 | issue = 4 | pages = 475–483 | date = April 2012 | pmid = 22449218 | doi = 10.1586/ern.12.15 | type = Review | s2cid = 35718630 }}</ref> and about 5% of cases are due to brain damage.<ref name="Erk_2009" />
| |
| − | | |
| − | Studies have shown a small but [[Statistical significance|significant relationship]] between media use and ADHD-related behaviors.<ref>{{cite journal|last1=Nikkelen|first1=Sanne W.C. |last2=Valkenburg|first2=Patti M.|last3=Huizinga|first3=Mariette|last4=Bushman|first4=Brad J.|year=2014|title=Media use and ADHD-related behaviors in children and adolescents: A meta-analysis|journal=[[Developmental Psychology (journal)|Developmental Psychology]] |volume=50 |issue=9|pages=2228–41|publisher=[[American Psychological Association]] |pmid=24999762 |doi=10.1037/a0037318 |s2cid=15418721 |url=https://research.vu.nl/en/publications/71197262-f534-411c-ae83-7b994100ff74 |access-date=13 June 2021 |archive-date=20 October 2021 |archive-url=https://web.archive.org/web/20211020044404/https://research.vu.nl/en/publications/media-use-and-adhd-related-behaviors-in-children-and-adolescents- |url-status=live}}</ref> In October 2018, ''[[Proceedings of the National Academy of Sciences of the United States of America|PNAS USA]]'' published a [[systematic review]] of four decades of research on the relationship between children and adolescents' screen media use and ADHD-related behaviors and concluded that a statistically small relationship between children's media use and ADHD-related behaviors exists.<ref>{{cite journal|last1=Beyens|first1=Ine|last2=Valkenburg|first2=Patti M. |last3=Piotrowski|first3=Jessica Taylor |title=Screen media use and ADHD-related behaviors: Four decades of research|date=2 October 2018 |journal=[[Proceedings of the National Academy of Sciences of the United States of America|PNAS USA]]|publisher=[[National Academy of Sciences]]|volume=115|issue=40|pages=9875–9881 |doi=10.1073/pnas.1611611114|pmid=30275318|pmc=6176582|bibcode=2018PNAS..115.9875B |doi-access=free}}</ref> In July 2018, the ''[[JAMA|Journal of the American Medical Association]]'' published a two-month [[Longitudinal study|longitudinal]] [[Cohort study|cohort survey]] of 3,051 U.S. teenagers ages 15 and 16 (recruited at 10 different [[Los Angeles County, California]] [[Secondary education in the United States|secondary schools]] by [[convenience sampling]]) [[Self-report inventory|self-reporting]] engagement in 14 different modern digital media activities at high-frequency. 2,587 subjects had no significant symptoms of ADHD at baseline with a [[Standard deviation|mean number]] of 3.62 modern digital media activities used at high-frequency and each additional activity used frequently at baseline positively correlating with a significantly higher probability of ADHD symptoms at follow-ups. 495 subjects who reported no high-frequency digital media activities at baseline had a 4.6% mean rate of having ADHD symptoms at follow-ups, as compared with 114 subjects who reported 7 high-frequency activities who had a 9.5% mean rate at follow-ups and 51 subjects with 14 high-frequency activities who had a 10.5% mean rate at follow-ups (indicating a statistically significant but modest association between higher frequency of digital media use and subsequent symptoms of ADHD).<ref>{{cite journal |last1=Ra |first1=Chaelin K. |last2=Cho |first2=Junhan |last3=Stone |first3=Matthew D. |last4=De La Cerda |first4=Julianne |last5=Goldenson |first5=Nicholas I.|last6=Moroney|first6=Elizabeth|last7=Tung|first7=Irene|last8=Lee|first8=Steve S. |last9=Leventhal |first9=Adam M. |title=Association of Digital Media Use With Subsequent Symptoms of Attention-Deficit/Hyperactivity Disorder Among Adolescents |date=17 July 2018 |journal=[[JAMA (journal)|JAMA]] |publisher=[[American Medical Association]] |volume=320 |issue=3 |pages=255–263 |doi=10.1001/jama.2018.8931 |pmid=30027248 |pmc=6553065 |url=https://jamanetwork.com/journals/jama/fullarticle/2687861|access-date=8 July 2020 |archive-date=10 June 2021 |archive-url=https://web.archive.org/web/20210610025116/https://jamanetwork.com/journals/jama/fullarticle/2687861 |url-status=live}}</ref><ref>{{cite news |last=Chatterjee|first=Rhitu|title=More Screen Time For Teens Linked To ADHD Symptoms|date=17 July 2018|work=[[Morning Edition]] |publisher=[[NPR]]|url=https://www.npr.org/sections/health-shots/2018/07/17/629517464/more-screen-time-for-teens-may-fuel-adhd-symptoms |access-date=8 July 2020|archive-date=10 June 2021|archive-url=https://web.archive.org/web/20210610025056/https://www.npr.org/sections/health-shots/2018/07/17/629517464/more-screen-time-for-teens-may-fuel-adhd-symptoms|url-status=live}}</ref><ref>{{cite news |last=Clopton|first=Jennifer|title=ADHD Rising in the U.S., but Why?|date=20 November 2018|website=[[WebMD]]|publisher=[[Internet Brands]] |url=https://www.webmd.com/add-adhd/news/20181126/adhd-rising-in-the-us-but-why |access-date=8 July 2020|archive-date=10 June 2021 |archive-url=https://web.archive.org/web/20210610025058/https://www.webmd.com/add-adhd/news/20181126/adhd-rising-in-the-us-but-why|url-status=live}}</ref>
| |
| | | | |
| − | In April 2019, ''[[PLOS One]]'' published the results of a longitudinal birth cohort study of [[screen time]] use reported by parents of 2,322 children in Canada at ages 3 and 5 and found that compared to children with less than 30 minutes per day of screen time, children with more than 2 hours of screen time per day had a 7.7-fold increased risk of meeting criteria for ADHD.<ref>{{cite journal |last1=Tamana |first1=Sukhpreet K. |last2=Ezeugwu |first2=Victor |last3=Chikuma |first3=Joyce |last4=Lefebvre |first4=Diana L. |last5=Azad |first5=Meghan B. |last6=Moraes |first6=Theo J. |last7=Subbarao |first7=Padmaja |last8=Becker |first8=Allan B. |last9=Turvey |first9=Stuart E. |last10=Sears |first10=Malcolm R. |last11=Dick |first11=Bruce D. |last12=Carson |first12=Valerie |last13=Rasmussen |first13=Carmen |last14=Pei |first14=Jacqueline |last15=Mandhane |first15=Piush J. |title=Screen-time is associated with inattention problems in preschoolers: Results from the CHILD birth cohort study |date=17 April 2019|journal=[[PLOS One]] |publisher=[[PLOS]] |volume=14 |issue=4 |page=e0213995 |pmid=30995220 |doi=10.1371/journal.pone.0213995 |pmc=6469768 |bibcode=2019PLoSO..1413995T |doi-access=free}}</ref> In January 2020, the ''Italian Journal of Pediatrics'' published a [[cross-sectional study]] of 1,897 children from ages 3 through 6 attending 42 [[kindergarten]]s in [[Wuxi]], China that also found that children exposed to more than 1 hour of screen-time per day were at increased risk for the development of ADHD and noted its similarity to a finding relating screen time and the development of [[Autism spectrum|autism spectrum disorder]] (ASD).<ref>{{cite journal |last1=Xie |first1=Guodong |last2=Deng |first2=Qianye |last3=Cao |first3=Jing |last4=Chang |first4=Qing |title=Digital screen time and its effect on preschoolers' behavior in China: results from a cross-sectional study |year=2020 |journal=Italian Journal of Pediatrics |publisher=[[Springer Nature]] |volume=46 |issue=9 |page=9 |doi=10.1186/s13052-020-0776-x |pmid=31973770 |pmc=6979375 |doi-access=free}}</ref> In November 2020, ''[[Infant Behavior and Development]]'' published a study of 120 3-year-old children with or without [[Family history (medicine)|family histories]] of ASD or ADHD (20 with ASD, 14 with ADHD, and 86 for comparison) examining the relationship between screen time, behavioral outcomes, and [[Spoken language|expressive]]/[[Language processing in the brain|receptive]] [[language development]] that found that higher screen time was associated with lower expressive/receptive language scores across comparison groups and that screen time was associated with [[Phenotype#Difficulties in definition|behavioral phenotype]], [[Behavioral epigenetics|not family history]] of ASD or ADHD.<ref name="Hill et. al 2020">{{cite journal |last1=Hill |first1=Monique Moore |last2=Gangi |first2=Devon |last3=Miller |first3=Meghan |last4=Rafi |first4=Sabrina Mohamed |last5=Ozonoff |first5=Sally |year=2020 |title=Screen time in 36-month-olds at increased likelihood for ASD and ADHD |journal=[[Infant Behavior and Development]] |publisher=[[Elsevier]] |volume=61 |issue= |page=101484 |doi=10.1016/j.infbeh.2020.101484 |pmid=32871326 |pmc=7736468}}</ref>
| + | Environmental risk factors that have been identified as risk factors for ADHD include:<ref>[https://www.adhdcentre.co.uk/exploring-the-links-between-adhd-and-environmental-factors/ Exploring the Links Between ADHD and Environmental Factors] ''The ADHD Centre'' (July 13, 2023). Retrieved January 22, 2024.</ref> |
| | + | *Maternal smoking, [[alcohol]] consumption, and drug use during pregnancy |
| | + | *Premature birth, or a low birth weight |
| | + | *Environmental toxins, including exposure to lead and [[pesticide]]s, and air pollution |
| | + | *Some illnesses, such as bacterial diseases (such as [[encephalitis]]) |
| | | | |
| − | In 2015, ''[[Preventive Medicine (journal)|Preventive Medicine Reports]]'' published a [[General linear model|multivariate linear]] and [[logistic regression]] study of 7,024 subjects aged 6–17 in the [[Maternal and Child Health Bureau]]'s 2007 National Survey of Children's Health examining the association between [[bedroom]] [[television]]s and screen time in children and adolescents diagnosed with ADHD that found that 59 percent of subjects had a bedroom television, subjects with bedroom televisions averaged 159.1 minutes of screen time per weekday versus 115.2 minutes per weekday for those without, and after adjusting for child and family characteristics, a bedroom television was associated with 25.1 minutes more of screen time per weekday and a 32.1 percent higher probability of average weekday screen time exceeding 2 hours.<ref>{{cite journal |last1=Lo |first1=Charmaine B. |last2=Waring |first2=Molly E. |last3=Pagoto |first3=Sherry L. |author-link3=Sherry Pagoto |last4=Lemon |first4=Stephenie C. |year=2015 |title=A television in the bedroom is associated with higher weekday screen time among youth with attention deficit hyperactivity disorder (ADD/ADHD) |journal=[[Preventive Medicine (journal)|Preventive Medicine Reports]] |publisher=[[Elsevier]] |volume=2 |pages=1–3 |issn=2211-3355 |doi=10.1016/j.pmedr.2014.11.001 |pmid=25599016 |pmc=4292909 }}</ref> In July 2021, ''[[Sleep Medicine Reviews|Sleep Medicine]]'' published a correlational study of 374 [[France|French]] children with a mean age of 10.8±2.8 years where parents completed the Sleep Disturbance Scale for Children (SDSC), the [[ADHD rating scale|ADHD Rating Scale]], and a questionnaire about the subjects screen time habits during the [[morning]], [[afternoon]], and [[evening]] that found that subjects with bedroom televisions had greater sleep disturbance and ADHD symptoms, that evening screen time was associated with higher SDSC and ADHD scores, and that [[structural equation modeling]] demonstrated that evening screen time was directly associated with greater sleep disturbance which in turn was directly associated with greater ADHD symptoms.<ref>{{cite journal |last1=Cavalli |first1=Eddy |last2=Anders |first2=Royce |last3=Chaussoy |first3=Louise |last4=Herbillon |first4=Vania |last5=Franco |first5=Patricia |last6=Putois |first6=Benjamin |year=2021 |title=Screen exposure exacerbates ADHD symptoms indirectly through increased sleep disturbance |journal=Sleep Medicine |publisher=Elsevier |volume=83 |pages=241–247 |doi=10.1016/j.sleep.2021.03.010 |pmid=34049043 |s2cid=233655160}}</ref>
| + | Studies have shown a relationship between media use and ADHD-related behaviors.<ref>S.W.C. Nikkelen, P.M. Valkenburg, Mariëtte Huizinga, and B.J. Bushman, [https://research.vu.nl/en/publications/media-use-and-adhd-related-behaviors-in-children-and-adolescents- Media use and ADHD-related behaviors in children and adolescents: A meta-analysis] ''Developmental Psychology'' 50(9) (2014):2228–2241. Retrieved January 22, 2024.</ref> In October 2018, ''[[Proceedings of the National Academy of Sciences of the United States of America|PNAS USA]]'' published a [[systematic review]] of four decades of research on the relationship between children and adolescents' screen media use and ADHD-related behaviors and concluded that a statistically small relationship between children's media use and ADHD-related behaviors exists.<ref>Ine Beyens, Patti M, Valkenburg, and Jessica Taylor Piotrowski, [https://pubmed.ncbi.nlm.nih.gov/30275318/ Screen media use and ADHD-related behaviors: Four decades of research]''Proceedings of the National Academy of Sciences of the United States of America'' (PNAS USA) 115(40) (October 2, 2018):9875–9881. Retrieved January 22, 2024.</ref> |
| | | | |
| | == Pathophysiology == | | == Pathophysiology == |
| | === Brain structure === | | === Brain structure === |
| − | Once neuroimaging studies were possible, studies conducted in the 1990s provided support for the pre-existing theory that neurological differences - particularly in the [[frontal lobe]]s - were involved in ADHD. | + | Once neuroimaging studies became possible, studies conducted in the 1990s provided support for the pre-existing theory that neurological differences - particularly in the [[frontal lobe]]s - were involved in ADHD. |
| − | | |
| − | In children with ADHD, there is a general reduction of volume in certain brain structures, with a proportionally greater decrease in the volume in the left-sided [[prefrontal cortex]].<ref name="Malenka ADHD neurosci" /><ref name="Krain2006">{{cite journal |vauthors=Krain AL, Castellanos FX |title=Brain development and ADHD |journal=Clinical Psychology Review |volume=26 |issue=4 |pages=433–444 |date=August 2006 |pmid=16480802 |doi=10.1016/j.cpr.2006.01.005 }}</ref> The [[posterior parietal cortex]] also shows thinning in individuals with ADHD compared to controls. Other brain structures in the prefrontal-striatal-cerebellar and prefrontal-striatal-thalamic circuits have also been found to differ between people with and without ADHD.<ref name="Malenka ADHD neurosci" /><ref name="pmid22169776" /><ref name="pmid22983386" />
| |
| | | | |
| − | The subcortical volumes of the [[accumbens]], [[amygdala]], [[Caudate nucleus|caudate]], [[hippocampus]], and [[putamen]] appears smaller in individuals with ADHD compared with controls.<ref>{{cite journal |vauthors=Hoogman M, Bralten J, Hibar DP, Mennes M, Zwiers MP, Schweren LS, van Hulzen KJ, Medland SE, Shumskaya E, Jahanshad N, Zeeuw P, Szekely E, Sudre G, Wolfers T, Onnink AM, Dammers JT, Mostert JC, Vives-Gilabert Y, Kohls G, Oberwelland E, Seitz J, Schulte-Rüther M, Ambrosino S, Doyle AE, Høvik MF, Dramsdahl M, Tamm L, van Erp TG, Dale A, Schork A, Conzelmann A, Zierhut K, Baur R, McCarthy H, Yoncheva YN, Cubillo A, Chantiluke K, Mehta MA, Paloyelis Y, Hohmann S, Baumeister S, Bramati I, Mattos P, Tovar-Moll F, Douglas P, Banaschewski T, Brandeis D, Kuntsi J, Asherson P, Rubia K, Kelly C, Martino AD, Milham MP, Castellanos FX, Frodl T, Zentis M, Lesch KP, Reif A, Pauli P, Jernigan TL, Haavik J, Plessen KJ, Lundervold AJ, Hugdahl K, Seidman LJ, Biederman J, Rommelse N, Heslenfeld DJ, Hartman CA, Hoekstra PJ, Oosterlaan J, Polier GV, Konrad K, Vilarroya O, Ramos-Quiroga JA, Soliva JC, Durston S, Buitelaar JK, Faraone SV, Shaw P, Thompson PM, Franke B |display-authors=6 |title=Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: a cross-sectional mega-analysis |journal=The Lancet. Psychiatry |volume=4 |issue=4 |pages=310–319 |date=April 2017 |pmid=28219628 |pmc=5933934 |doi=10.1016/S2215-0366(17)30049-4 }}</ref> Structural MRI studies have also revealed differences in white matter, with marked differences in inter-hemispheric asymmetry between ADHD and typically developing youths.<ref>{{cite journal |vauthors=Douglas PK, Gutman B, Anderson A, Larios C, Lawrence KE, Narr K, Sengupta B, Coorray G, Douglas DB, Thompson PM, McGough JJ, Bookheimer SY |journal=NeuroImage: Clinical |title=Hemispheric brain asymmetry differences in youths with attention-deficit/hyperactivity disorder |volume=18 |pages=744–752 |date=February 2018 |pmid=29876263 |pmc=5988460 |doi=10.1016/j.nicl.2018.02.020 }}</ref>
| + | In children with ADHD, there is a general reduction of volume in certain brain structures, with a proportionally greater decrease in the volume in the left-sided [[prefrontal cortex]].<ref name="Krain2006">Amy L Krain and F. Xavier Castellanos, [https://pubmed.ncbi.nlm.nih.gov/16480802/ Brain development and ADHD] ''Clinical Psychology Review'' 26(4) (August 2005):433–444. Retrieved January 22, 2024.</ref> Other brain structures in the prefrontal-striatal-cerebellar and prefrontal-striatal-thalamic circuits have also been found to differ between people with and without ADHD, while the subcortical volumes of the [[accumbens]], [[amygdala]], [[Caudate nucleus|caudate]], [[hippocampus]], and [[putamen]] appears smaller in individuals with ADHD compared with controls.<ref>Martine Hoogman et al., [https://pubmed.ncbi.nlm.nih.gov/28219628/ Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: a cross-sectional mega-analysis] ''Lancet Psychiatry'' 4(4) (April 2017):310-319. Retrieved January 22, 2024.</ref> Structural MRI studies have also revealed differences in white matter, with marked differences in inter-hemispheric asymmetry between ADHD and typically developing youths.<ref>P.K. Douglas et al., [https://pubmed.ncbi.nlm.nih.gov/29876263/ Hemispheric brain asymmetry differences in youths with attention-deficit/hyperactivity disorder] ''Neuroimage Clin.'' 18 (February 2018):744–752. Retrieved January 22, 2024. </ref> |
| | | | |
| − | [[Functional magnetic resonance imaging|Function MRI]] (fMRI) studies have revealed a number of differences between ADHD and control brains. Mirroring what is known from structural findings, fMRI studies have showed evidence for a higher connectivity between subcortical and cortical regions, such as between the caudate and prefrontal cortex. The degree of hyperconnectivity between these regions correlated with the severity of inattention or hyperactivity <ref name="Damiani_2021">{{cite journal |display-authors=6 |vauthors=Damiani S, Tarchi L, Scalabrini A, Marini S, Provenzani U, Rocchetti M, Oliva F, Politi P |date=April 2021 |title=Beneath the surface: hyper-connectivity between caudate and salience regions in ADHD fMRI at rest |journal=European Child & Adolescent Psychiatry |volume=30 |issue=4 |pages=619–631 |doi=10.1007/s00787-020-01545-0 |pmid=32385695 |s2cid=218540328 |hdl=2318/1755224|hdl-access=free }}</ref> Hemispheric lateralization processes have also been postulated as being implicated in ADHD, but empiric results showed contrasting evidence on the topic.<ref name="Tarchi_2022">{{cite journal | vauthors = Tarchi L, Damiani S, Fantoni T, Pisano T, Castellini G, Politi P, Ricca V | title = Centrality and interhemispheric coordination are related to different clinical/behavioral factors in attention deficit/hyperactivity disorder: a resting-state fMRI study | journal = Brain Imaging and Behavior | volume = 16 | issue = 6 | pages = 2526–2542 | date = December 2022 | pmid = 35859076 | pmc = 9712307 | doi = 10.1007/s11682-022-00708-8 }}</ref><ref>{{cite journal | vauthors = Mohamed SM, Börger NA, Geuze RH, van der Meere JJ | title = Brain lateralization and self-reported symptoms of ADHD in a population sample of adults: a dimensional approach | journal = Frontiers in Psychology | volume = 6 | pages = 1418 | date = 2015 | pmid = 26441789 | doi = 10.3389/fpsyg.2015.01418 | pmc = 4585266 | doi-access = free }}</ref> | + | [[Functional magnetic resonance imaging|Function MRI]] (fMRI) studies have revealed a number of differences between ADHD and control brains. Mirroring what is known from structural findings, fMRI studies have shown evidence for a higher connectivity between subcortical and cortical regions, such as between the caudate and prefrontal cortex. The degree of hyperconnectivity between these regions correlated with the severity of inattention or hyperactivity <ref>Stefano Damiani et al., [https://pubmed.ncbi.nlm.nih.gov/32385695/ Beneath the surface: hyper-connectivity between caudate and salience regions in ADHD fMRI at rest] ''European Child & Adolescent Psychiatry'' 30(4) (April 2021):619–631. Retrieved January 22, 2024.</ref> |
| | | | |
| − | === Executive function and motivation === | + | === Executive function === |
| − | The symptoms of ADHD arise from a deficiency in certain [[executive function]]s (e.g., [[attentional control]], [[inhibitory control]], and [[working memory]]).<ref name="Malenka ADHD neurosci" /> Executive functions are a set of [[Cognition|cognitive processes]] that are required to successfully select and monitor behaviours that facilitate the attainment of one's chosen goals.<ref name="Malenka pathways" /><ref name="Executive functions" /> The executive function impairments that occur in ADHD individuals result in problems with staying organised, time keeping, excessive [[procrastination]], maintaining concentration, paying attention, ignoring distractions, regulating emotions, and remembering details.<ref name="Brown_2008" /><ref name="Malenka ADHD neurosci" /><ref name="Malenka pathways" /> People with ADHD appear to have unimpaired long-term memory, and deficits in long-term recall appear to be attributed to impairments in working memory.<ref name="pmid24232170">{{cite journal |vauthors=Skodzik T, Holling H, Pedersen A |title=Long-Term Memory Performance in Adult ADHD |journal=Journal of Attention Disorders |volume=21 |issue=4 |pages=267–283 |date=February 2017 |pmid=24232170 |doi=10.1177/1087054713510561 |s2cid=27070077 }}</ref> Due to the rates of brain maturation and the increasing demands for executive control as a person gets older, ADHD impairments may not fully manifest themselves until adolescence or even early adulthood.<ref name="Brown_2008" /> Conversely, brain maturation trajectories, potentially exhibiting diverging longitudinal trends in ADHD, may support a later improvement in executive functions after reaching adulthood.<ref name="Tarchi_2022" /> | + | The symptoms of ADHD arise from a deficiency in certain [[executive function]]s - the [[Cognition|cognitive processes]] that are required to successfully select and monitor behaviors that facilitate the attainment of one's chosen goals. The executive function impairments that occur in ADHD individuals result in problems with staying organized, time keeping, excessive [[procrastination]], maintaining concentration, paying attention, ignoring distractions, regulating emotions, and remembering details. Due to the rates of brain maturation and the increasing demands for executive control as a person gets older, ADHD impairments may not fully manifest themselves until adolescence or even early adulthood.<ref name="Brown_2008">Thomas E. Brown, [https://pubmed.ncbi.nlm.nih.gov/18803914/ ADD/ADHD and Impaired Executive Function in Clinical Practice] ''Current Psychiatry Reports'' 10(5) (October 2008):407–411. Retrieved January 22, 2024.</ref> Conversely, brain maturation trajectories, potentially exhibiting diverging longitudinal trends in ADHD, may support a later improvement in executive functions after reaching adulthood. |
| | | | |
| − | ADHD has also been associated with motivational deficits in children. Children with ADHD often find it difficult to focus on long-term over short-term rewards, and exhibit impulsive behaviour for short-term rewards.<ref name="Motivation">{{cite journal |vauthors=Modesto-Lowe V, Chaplin M, Soovajian V, Meyer A |date=July 2013 |title=Are motivation deficits underestimated in patients with ADHD? A review of the literature |journal=Postgraduate Medicine |volume=125 |issue=4 |pages=47–52 |doi=10.3810/pgm.2013.07.2677 |pmid=23933893 |s2cid=24817804 |quote=Behavioral studies show altered processing of reinforcement and incentives in children with ADHD. These children respond more impulsively to rewards and choose small, immediate rewards over larger, delayed incentives. Interestingly, a high intensity of reinforcement is effective in improving task performance in children with ADHD. Pharmacotherapy may also improve task persistence in these children. ... Previous studies suggest that a clinical approach using interventions to improve motivational processes in patients with ADHD may improve outcomes as children with ADHD transition into adolescence and adulthood.}}</ref> | + | ADHD has also been associated with motivational deficits in children. Children with ADHD often find it difficult to focus on long-term over short-term rewards, and exhibit impulsive behavior for short-term rewards.<ref>Vania Modesto-Lowe, Margaret Chaplin, Victoria Soovajian, and Andrea Meyer, [https://pubmed.ncbi.nlm.nih.gov/23933893/ Are motivation deficits underestimated in patients with ADHD? A review of the literature] ''Postgraduate Medicine'' 125(4) (July 2013):47–52. Retrieved January 22, 2024.</ref> |
| | | | |
| − | === Paradoxical reaction to neuroactive substances === | + | === Paradoxical reaction === |
| − | Another sign of the structurally altered signal processing in the central nervous system in this group of people is the conspicuously common [[Paradoxical reaction]]. These are unexpected reactions in the opposite direction to the normal effect, or otherwise significant different reactions. These are reactions to neuroactive substances such as [[local anesthetic]] at the dentist, [[sedative]], [[caffeine]], [[antihistamine]], weak [[neuroleptics]], and central and peripheral [[painkillers]]. | + | Another sign of the structurally altered signal processing in the central nervous system in this group of people is the conspicuously common [[Paradoxical reaction]]. These are unexpected reactions to a chemical substance, such as a medical drug, that is opposite to what would usually be expected, or an otherwise significantly different reactions. They may occur with neuroactive substances such as [[local anesthetic]] at the dentist, [[sedative]], [[caffeine]], [[antihistamine]], weak [[neuroleptics]], and central and peripheral [[painkillers]]. |
| | | | |
| | ==Management== | | ==Management== |
| − | [[Attention deficit hyperactivity disorder management|ADHD management]] recommendations vary and usually involve some combination of medications, [[psychotherapy|counseling]], and lifestyle changes.<ref name="NIH2016">{{cite web |title=Attention Deficit Hyperactivity Disorder |date=March 2016 |url=http://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd/index.shtml |website=National Institute of Mental Health |access-date=5 March 2016 |url-status=live |archive-url=https://web.archive.org/web/20160723192735/http://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd/index.shtml |archive-date=23 July 2016}}</ref> The British guideline emphasises environmental modifications and education about ADHD for individuals and carers as the first response. If symptoms persist, parent-training, medication, or psychotherapy (especially [[cognitive behavioural therapy]]) can be recommended based on age.<ref name="NICE_2019">{{Cite book |author=National Institute for Health and Care Excellence |url=https://www.nice.org.uk/guidance/ng87/ |title=Attention deficit hyperactivity disorder: diagnosis and management |publisher=National Guideline Centre (UK) |year=2019 |isbn=978-1-4731-2830-9 |series=NICE Guideline, No. 87 |location=London |pages= |oclc=1126668845 |access-date=9 January 2021 |archive-date=12 January 2021 |archive-url=https://web.archive.org/web/20210112035209/https://www.nice.org.uk/guidance/ng87/ |url-status=live }}</ref> Canadian and American guidelines recommend medications and behavioural therapy together, except in preschool-aged children for whom the first-line treatment is behavioural therapy alone.<ref name="CADDRA">{{cite web |title=Canadian ADHD Practice Guidelines |work=Canadian ADHD Resource Alliance |url=http://www.caddra.ca/cms4/pdfs/caddraGuidelines2011Introduction.pdf |access-date=4 February 2011 |archive-date=21 January 2021 |archive-url=https://web.archive.org/web/20210121222344/https://www.caddra.ca/cms4/pdfs/caddraGuidelines2011Introduction.pdf |url-status=live }}</ref><ref name="CDC guideline">{{cite web |title=Attention-Deficit / Hyperactivity Disorder (ADHD): Recommendations |url=https://www.cdc.gov/ncbddd/adhd/guidelines.html |publisher=Centers for Disease Control and Prevention |access-date=13 July 2015 |date=24 June 2015 |url-status=live |archive-date=7 July 2015 |archive-url=https://web.archive.org/web/20150707181535/http://www.cdc.gov/ncbddd/adhd/guidelines.html}}</ref><ref name="APP2019">{{cite journal |vauthors=Wolraich ML, Hagan JF, Allan C, Chan E, Davison D, Earls M, Evans SW, Flinn SK, Froehlich T, Frost J, Holbrook JR, Lehmann CU, Lessin HR, Okechukwu K, Pierce KL, Winner JD, Zurhellen W |display-authors=6 |title=Clinical Practice Guideline for the Diagnosis, Evaluation, and Treatment of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents |journal=Pediatrics |volume=144 |issue=4 |pages=e20192528 |date=October 2019 |pmid=31570648 |pmc=7067282 |doi=10.1542/peds.2019-2528 }}</ref>
| + | While there is no cure for ADHD, it is possible to reduce symptoms and improve functioning. ADHD management recommendations vary and usually involve some combination of medications, [[psychotherapy|counseling]], education or training, and lifestyle changes.<ref name="NIH2016">[https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd#part_2291 Attention Deficit Hyperactivity Disorder] ''National Institute of Mental Health''. Retrieved January 2, 2024. </ref> The British guideline emphasizes environmental modifications and education about ADHD for individuals and carers as the first response. If symptoms persist, parent-training, medication, or psychotherapy (especially [[cognitive behavioral therapy]]) can be recommended based on age.<ref name=NICE>[https://www.nice.org.uk/guidance/ng87 Attention deficit hyperactivity disorder: diagnosis and management] ''National Institute for Health and Care Excellence (NICE)'', September 13, 2019. Retrieved January 22, 2024. </ref> Canadian and American guidelines recommend medications and behavioral therapy together, except in preschool-aged children for whom the first-line treatment is behavioral therapy alone.<ref>[https://www.caddra.ca/cms4/pdfs/caddraGuidelines2011Introduction.pdf Canadian ADHD Practice Guidelines] ''Canadian Attention Deficit Hyperactivity Disorder Resource Alliance (CADDRA)'', 2010. Retrieved January 22, 2024.</ref> <ref>[https://www.cdc.gov/ncbddd/adhd/guidelines.html ADHD Treatment Recommendations] ''Centers for Disease Control and Prevention (CDC)''. Retrieved January 22, 2024.</ref> |
| | | | |
| − | While treatment may improve long-term outcomes, it does not get rid of negative outcomes entirely.<ref name="pmid22947230">{{cite journal |vauthors=Shaw M, Hodgkins P, Caci H, Young S, Kahle J, Woods AG, Arnold LE |title=A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: effects of treatment and non-treatment |journal=BMC Medicine |volume=10 |page=99 |date=September 2012 |pmid=22947230 |pmc=3520745 |doi=10.1186/1741-7015-10-99 |doi-access=free }}</ref>
| + | ===Behavioral therapies=== |
| | + | [[behavioral therapy|Behavioral therapies]] are the recommended first-line treatment in those who have mild symptoms or who are preschool-aged, and there is strong evidence for their effectiveness. Psychological therapies used include: [[psychoeducation]]al input, behavior therapy, [[cognitive behavioral therapy]], [[interpersonal psychotherapy]], [[family therapy]], school-based interventions, social skills training, behavioral peer intervention, organization training, and [[parent management training]].<ref name=NICE/> |
| | | | |
| − | ===Behavioural therapies===
| + | Parent training may improve a number of behavioral problems including oppositional and non-compliant behaviors. Social skills training, behavioral modification, and medication may have some limited beneficial effects in peer relationships. |
| − | There is good evidence for the use of [[behavioural therapy|behavioural therapies]] in ADHD. They are the recommended first-line treatment in those who have mild symptoms or who are preschool-aged.<ref>{{cite journal | vauthors = Fabiano GA, Pelham WE, Coles EK, Gnagy EM, Chronis-Tuscano A, O'Connor BC | title = A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder | journal = Clinical Psychology Review | volume = 29 | issue = 2 | pages = 129–140 | date = March 2009 | pmid = 19131150 | doi = 10.1016/j.cpr.2008.11.001 | quote = there is strong and consistent evidence that behavioral treatments are effective for treating ADHD. | doi-access = free }}</ref><ref name="Clinics09">{{cite journal | vauthors = Kratochvil CJ, Vaughan BS, Barker A, Corr L, Wheeler A, Madaan V | title = Review of pediatric attention deficit/hyperactivity disorder for the general psychiatrist | journal = The Psychiatric Clinics of North America | volume = 32 | issue = 1 | pages = 39–56 | date = March 2009 | pmid = 19248915 | doi = 10.1016/j.psc.2008.10.001 }}</ref> Psychological therapies used include: [[psychoeducation]]al input, behavior therapy, [[cognitive behavioral therapy]],<ref>{{cite journal | vauthors = Lopez PL, Torrente FM, Ciapponi A, Lischinsky AG, Cetkovich-Bakmas M, Rojas JI, Romano M, Manes FF | display-authors = 6 | title = Cognitive-behavioural interventions for attention deficit hyperactivity disorder (ADHD) in adults | journal = The Cochrane Database of Systematic Reviews | volume = 2018 | issue = 3 | pages = CD010840 | date = March 2018 | pmid = 29566425 | pmc = 6494390 | doi = 10.1002/14651858.CD010840.pub2 }}</ref> [[interpersonal psychotherapy]], [[family therapy]], school-based interventions, social skills training, behavioural peer intervention, organization training,<ref name="Evans2014">{{cite journal | vauthors = Evans SW, Owens JS, Bunford N | title = Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder | journal = Journal of Clinical Child and Adolescent Psychology | volume = 43 | issue = 4 | pages = 527–551 | date = 2014 | pmid = 24245813 | pmc = 4025987 | doi = 10.1080/15374416.2013.850700 }}</ref> and [[parent management training]].<ref name="NICE 2009" /> [[Neurofeedback]] has greater treatment effects than non-active controls for up to 6 months and possibly a year following treatment, and may have treatment effects comparable to active controls (controls proven to have a clinical effect) over that time period.<ref>{{cite journal | vauthors = Van Doren J, Arns M, Heinrich H, Vollebregt MA, Strehl U, K Loo S | title = Sustained effects of neurofeedback in ADHD: a systematic review and meta-analysis | journal = European Child & Adolescent Psychiatry | volume = 28 | issue = 3 | pages = 293–305 | date = March 2019 | pmid = 29445867 | pmc = 6404655 | doi = 10.1007/s00787-018-1121-4 | publisher = Springer Science and Business Media LLC }}</ref> Despite efficacy in research, there is insufficient regulation of neurofeedback practice, leading to ineffective applications and false claims regarding innovations.<ref>{{cite journal | vauthors = Enriquez-Geppert S, Smit D, Pimenta MG, Arns M | title = Neurofeedback as a Treatment Intervention in ADHD: Current Evidence and Practice | journal = Current Psychiatry Reports | volume = 21 | issue = 6 | pages = 46 | date = May 2019 | pmid = 31139966 | pmc = 6538574 | doi = 10.1007/s11920-019-1021-4 | publisher = Springer Science and Business Media LLC }}</ref> Parent training may improve a number of behavioural problems including oppositional and non-compliant behaviours.<ref name="Dal2017">{{cite journal | vauthors = Daley D, Van Der Oord S, Ferrin M, Cortese S, Danckaerts M, Doepfner M, Van den Hoofdakker BJ, Coghill D, Thompson M, Asherson P, Banaschewski T, Brandeis D, Buitelaar J, Dittmann RW, Hollis C, Holtmann M, Konofal E, Lecendreux M, Rothenberger A, Santosh P, Simonoff E, Soutullo C, Steinhausen HC, Stringaris A, Taylor E, Wong IC, Zuddas A, Sonuga-Barke EJ | display-authors = 6 | title = Practitioner Review: Current best practice in the use of parent training and other behavioural interventions in the treatment of children and adolescents with attention deficit hyperactivity disorder | journal = Journal of Child Psychology and Psychiatry, and Allied Disciplines | volume = 59 | issue = 9 | pages = 932–947 | date = September 2018 | pmid = 29083042 | doi = 10.1111/jcpp.12825 | url = http://eprints.nottingham.ac.uk/45391/ | access-date = 21 November 2018 | publisher = Wiley | url-status = live | s2cid = 31044370 | archive-date = 25 September 2017 | archive-url = https://web.archive.org/web/20170925140540/http://eprints.nottingham.ac.uk/45391/ | hdl = 11343/293788 | hdl-access = free }}</ref>
| |
| − | | |
| − | There is little high-quality research on the effectiveness of family therapy for ADHD—but the existing evidence shows that it is similar to community care, and better than placebo.<ref>{{cite journal |vauthors=Bjornstad G, Montgomery P |title=Family therapy for attention-deficit disorder or attention-deficit/hyperactivity disorder in children and adolescents |journal=The Cochrane Database of Systematic Reviews |issue=2 |pages=CD005042 |date=April 2005 |pmid=15846741 |doi=10.1002/14651858.CD005042.pub2 |s2cid=27339381 |veditors=Bjornstad GJ }}</ref> ADHD-specific support groups can provide information and may help families cope with ADHD.<ref name="Brain encyclopedia">{{cite encyclopedia |vauthors=Turkington C, Harris J |title=Attention deficit hyperactivity disorder (ADHD) |url={{google books|6hbKkynRxPYC |pages=42|plainurl=yes}} |encyclopedia=The Encyclopedia of the Brain and Brain Disorders |year=2009 |publisher=Infobase Publishing |isbn=978-1-4381-2703-3 |pages=[https://books.google.com/books?id=6hbKkynRxPYC&pg=PA47 47] |via=Google Books }}</ref>
| |
| − | | |
| − | Social skills training, behavioural modification, and medication may have some limited beneficial effects in peer relationships. Stable, high-quality friendships with [[Deviance (sociology)|non-deviant]] peers protect against later psychological problems.<ref name="pmid20490677">{{cite journal |vauthors=Mikami AY |title=The importance of friendship for youth with attention-deficit/hyperactivity disorder |journal=Clinical Child and Family Psychology Review |volume=13 |issue=2 |pages=181–198 |date=June 2010 |pmid=20490677 |pmc=2921569 |doi=10.1007/s10567-010-0067-y }}</ref> | |
| | | | |
| | ===Medication=== | | ===Medication=== |
| − | | + | The use of stimulants to treat ADHD was first described in 1937: Charles Bradley gave "problem" children Benzedrine to alleviate headaches and found it unexpectedly improved their school performance, social interactions, and emotional responses. Although Bradley's studies were basically ignored for nearly 25 years, they were an important precursor to studies of [[amphetamine]]s like Ritalin and their use in managing ADHD.<ref>Madeleine P. Strohl, [https://pubmed.ncbi.nlm.nih.gov/21451781/ Bradley's Benzedrine studies on children with behavioral disorders] ''Yale J Biol Med.'' 84(1) (March 2011):27-33. Retrieved January 22, 2024.</ref> |
| − | | |
| − | The use of stimulants to treat ADHD was first described in 1937.<ref>{{cite journal |vauthors=Patrick KS, Straughn AB, Perkins JS, González MA |title=Evolution of stimulants to treat ADHD: transdermal methylphenidate |journal=Human Psychopharmacology |volume=24 |issue=1 |pages=1–17 |date=January 2009 |pmid=19051222 |pmc=2629554 |doi=10.1002/hup.992 }}</ref> Charles Bradley gave the children with behavioral disorders Benzedrine and found it improved academic performance and behavior.<ref>{{cite journal |vauthors=Gross MD |title=Origin of stimulant use for treatment of attention deficit disorder |journal=The American Journal of Psychiatry |volume=152 |issue=2 |pages=298–299 |date=February 1995 |pmid=7840374 |issn=0002-953X |eissn=1535-7228| lccn=22024537 |oclc=1480183 |doi=10.1176/ajp.152.2.298b }}</ref><ref>{{Cite journal |vauthors=Brown W |date=1998 |title=Charles Bradley, M.D. |journal=American Journal of Psychiatry |issn=0002-953X |eissn=1535-7228| lccn=22024537 |volume=155 |issue=7 |oclc=1480183 |page=968 |doi=10.1176/ajp.155.7.968 }}</ref> | |
| − | | |
| | | | |
| | ====Stimulants==== | | ====Stimulants==== |
| − | [[Methylphenidate]] and [[amphetamine]] or its derivatives are often first-line treatments for ADHD.<ref name="Dodson_2005" /><ref>{{Cite journal |last1=Storebø |first1=Ole Jakob |last2=Storm |first2=Maja Rosenberg Overby |last3=Pereira Ribeiro |first3=Johanne |last4=Skoog |first4=Maria |last5=Groth |first5=Camilla |last6=Callesen |first6=Henriette E. |last7=Schaug |first7=Julie Perrine |last8=Darling Rasmussen |first8=Pernille |last9=Huus |first9=Christel-Mie L. |last10=Zwi |first10=Morris |last11=Kirubakaran |first11=Richard |last12=Simonsen |first12=Erik |last13=Gluud |first13=Christian |date=27 March 2023 |title=Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD) |journal=The Cochrane Database of Systematic Reviews |volume=2023 |issue=3 |pages=CD009885 |doi=10.1002/14651858.CD009885.pub3 |issn=1469-493X |pmc=10042435 |pmid=36971690 |pmc-embargo-date=27 March 2024 }}</ref> About 70 per cent respond to the first stimulant tried and as few as 10 per cent respond to neither amphetamines nor methylphenidate.<ref name="CNS09" /> Stimulants may also reduce the risk of unintentional injuries in children with ADHD.<ref name="Ruiz-Goikoetxea_2017">{{cite journal |vauthors=Ruiz-Goikoetxea M, Cortese S, Aznarez-Sanado M, Magallón S, Alvarez Zallo N, Luis EO, de Castro-Manglano P, Soutullo C, Arrondo G |display-authors=6 |title=Risk of unintentional injuries in children and adolescents with ADHD and the impact of ADHD medications: A systematic review and meta-analysis |journal=Neuroscience and Biobehavioral Reviews |volume=84 |pages=63–71 |date=January 2018 |pmid=29162520 |doi=10.1016/j.neubiorev.2017.11.007 |doi-access=free }}</ref> [[Magnetic resonance imaging]] studies suggest that long-term treatment with amphetamine or methylphenidate decreases abnormalities in brain structure and function found in subjects with ADHD.<ref name="Neuroplasticity 1">{{cite journal |vauthors=Hart H, Radua J, Nakao T, Mataix-Cols D, Rubia K |title=Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication, and age effects |journal=JAMA Psychiatry |volume=70 |issue=2 |pages=185–198 |date=February 2013 |pmid=23247506 |doi=10.1001/jamapsychiatry.2013.277 |doi-access=free }}</ref><ref name="Neuroplasticity 2">{{cite journal |vauthors=Spencer TJ, Brown A, Seidman LJ, Valera EM, Makris N, Lomedico A, Faraone SV, Biederman J |display-authors=6 |title=Effect of psychostimulants on brain structure and function in ADHD: a qualitative literature review of magnetic resonance imaging-based neuroimaging studies |journal=The Journal of Clinical Psychiatry |volume=74 |issue=9 |pages=902–917 |date=September 2013 |pmid=24107764 |pmc=3801446 |doi=10.4088/JCP.12r08287 }}</ref><ref name="Neuroplasticity 3">{{cite journal |vauthors=Frodl T, Skokauskas N |title=Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects |journal=Acta Psychiatrica Scandinavica |volume=125 |issue=2 |pages=114–126 |date=February 2012 |pmid=22118249 |doi=10.1111/j.1600-0447.2011.01786.x |quote=Basal ganglia regions like the right globus pallidus, the right putamen, and the nucleus caudatus are structurally affected in children with ADHD. These changes and alterations in limbic regions like {{abbr|ACC|anterior cingulate cortex}} and amygdala are more pronounced in non-treated populations and seem to diminish over time from child to adulthood. Treatment seems to have positive effects on brain structure. |s2cid=25954331 |doi-access=free }}</ref> A 2018 review found the greatest short-term benefit with methylphenidate in children, and amphetamines in adults.<ref>{{cite journal |vauthors=Cortese S, Adamo N, Del Giovane C, Mohr-Jensen C, Hayes AJ, Carucci S, Atkinson LZ, Tessari L, Banaschewski T, Coghill D, Hollis C, Simonoff E, Zuddas A, Barbui C, Purgato M, Steinhausen HC, Shokraneh F, Xia J, Cipriani A |display-authors=6 |title=Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis |journal=The Lancet. Psychiatry |volume=5 |issue=9 |pages=727–738 |date=September 2018 |pmid=30097390 |pmc=6109107 |doi=10.1016/S2215-0366(18)30269-4}}</ref> Studies and meta-analyses show that amphetamine is slightly-to-modestly more effective than methylphenidate at reducing symptoms,<ref>{{Cite journal |last1=Stuhec |first1=Matej |last2=Lukić |first2=Petar |last3=Locatelli |first3=Igor |date=February 2019 |title=Efficacy, Acceptability, and Tolerability of Lisdexamfetamine, Mixed Amphetamine Salts, Methylphenidate, and Modafinil in the Treatment of Attention-Deficit Hyperactivity Disorder in Adults: A Systematic Review and Meta-analysis |journal=Annals of Pharmacotherapy |language=en |volume=53 |issue=2 |pages=121–133 |doi=10.1177/1060028018795703 |pmid=30117329 |s2cid=52019992 |issn=1060-0280}}</ref><ref>{{Cite journal |last1=Faraone |first1=Stephen V. |last2=Biederman |first2=Joseph |last3=Roe |first3=Christine |date=October 2002 |title=Comparative Efficacy of Adderall and Methylphenidate in Attention-deficit/Hyperactivity Disorder: A Meta-Analysis |journal=Journal of Clinical Psychopharmacology |language=en-US |volume=22 |issue=5 |pages=468–473 |doi=10.1097/00004714-200210000-00005 |pmid=12352269 |s2cid=19726926 |issn=0271-0749}}</ref> and they are more effective pharmacotherapy for ADHD than [[Alpha-adrenergic agonist#α2 agonist|α2-agonists]]<ref>{{cite journal |journal=Journal of the Korean Academy of Child and Adolescent Psychiatry |doi=10.5765/jkacap.210034 |vauthors=Seok-Hyun N, Myung L, Tae P |title=Stimulant Induced Movement Disorders in Attention Deficit Hyperactivity Disorder |pmc=8984208 |pmid=35418800 |date=1 April 2022 |volume=33 |issue=2 |pages=27–34}}</ref> but methylphenidate has comparable efficacy to non-stimulants such as atomoxetine. | + | [[Methylphenidate]] and [[amphetamine]] or its derivatives are often first-line treatments for ADHD.<ref>Ole Jakob Storebø et al., [https://pubmed.ncbi.nlm.nih.gov/36971690/ Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD)] ''Cochrane Database Syst Rev.'' 3(3) (March 27, 2023:CD009885. Retrieved January 22, 2024.</ref> Studies show that amphetamine is slightly-to-modestly more effective than methylphenidate at reducing symptoms.<ref>Stephen V. Faraone, Joseph Biederman, and Christine Roe, [https://pubmed.ncbi.nlm.nih.gov/12352269/ Efficacy, Acceptability, and Tolerability of Lisdexamfetamine, Mixed Amphetamine Salts, Methylphenidate, and Modafinil in the Treatment of Attention-Deficit Hyperactivity Disorder in Adults: A Systematic Review and Meta-analysis] ''Annals of Pharmacotherapy'' 53(2) (2002):121–133. Retrieved January 22, 2024. </ref> |
| | | | |
| | ====Non-stimulants==== | | ====Non-stimulants==== |
| | Two non-stimulant medications, [[atomoxetine]] and [[viloxazine]], are approved by the FDA and in other countries for the treatment of ADHD. They produce comparable efficacy and tolerability to methylphenidate, but all three tend to be modestly more tolerable and less effective than amphetamines. | | Two non-stimulant medications, [[atomoxetine]] and [[viloxazine]], are approved by the FDA and in other countries for the treatment of ADHD. They produce comparable efficacy and tolerability to methylphenidate, but all three tend to be modestly more tolerable and less effective than amphetamines. |
| | | | |
| − | | + | Two [[Alpha-2 agonists|alpha-2a agonists]], extended-release formulations of [[guanfacine]] and [[clonidine]], are approved by the FDA and in other countries for the treatment of ADHD (effective in children and adolescents but effectiveness has still not been shown for adults). They appear to be modestly less effective than the stimulants (amphetamine and methylphenidate) and non-stimulants (atomoxetine and viloxazine) at reducing symptoms, but can be useful alternatives or used in conjunction with a stimulant.<ref>Sharon B. Wigal, [https://pubmed.ncbi.nlm.nih.gov/19621975/ Efficacy and safety limitations of attention-deficit hyperactivity disorder pharmacotherapy in children and adults] ''CNS Drugs'' (23)(Suppl 1) (2009):21–31. Retrieved January 22, 2024.</ref> |
| − | '''Alpha-2a agonists'''
| |
| − | | |
| − | Two [[Alpha-2 agonists|alpha-2a agonists]], extended-release formulations of [[guanfacine]] and [[clonidine]], are approved by the FDA and in other countries for the treatment of ADHD (effective in children and adolescents but effectiveness has still not been shown for adults).<ref>{{cite journal |vauthors=Childress AC, Sallee FR |title=Revisiting clonidine: an innovative add-on option for attention-deficit/hyperactivity disorder |journal=Drugs of Today |volume=48 |issue=3 |pages=207–217 |date=March 2012 |pmid=22462040 |doi=10.1358/dot.2012.48.3.1750904}}</ref><ref name="Huss Chen Ludolph 2016 pp. 1–25">{{cite journal |vauthors=Huss M, Chen W, Ludolph AG |title=Guanfacine Extended Release: A New Pharmacological Treatment Option in Europe |journal=Clinical Drug Investigation |volume=36 |issue=1 |pages=1–25 |date=January 2016 |pmid=26585576 |pmc=4706844 |doi=10.1007/s40261-015-0336-0 |publisher=Springer Science and Business Media LLC }}</ref> They appear to be modestly less effective than the stimulants (amphetamine and methylphenidate) and non-stimulants (atomoxetine and viloxazine) at reducing symptoms,<ref>{{Cite journal |last1=Biederman |first1=Joseph |last2=Melmed |first2=Raun D. |last3=Patel |first3=Anil |last4=McBurnett |first4=Keith |last5=Konow |first5=Jennifer |last6=Lyne |first6=Andrew |last7=Scherer |first7=Noreen |collaboration=SPD503 Study Group |date=January 2008 |title=A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder |journal=Pediatrics |volume=121 |issue=1 |pages=e73–84 |doi=10.1542/peds.2006-3695 |issn=1098-4275 |pmid=18166547|s2cid=25551406 }}</ref><ref>{{Cite journal |last1=Palumbo |first1=Donna R. |last2=Sallee |first2=Floyd R. |last3=Pelham |first3=William E. |last4=Bukstein |first4=Oscar G. |last5=Daviss |first5=W. Burleson |last6=McDermott |first6=Michael P. |date=February 2008 |title=Clonidine for Attention-Deficit/Hyperactivity Disorder: I. Efficacy and Tolerability Outcomes |journal=Journal of the American Academy of Child & Adolescent Psychiatry |volume=47 |issue=2 |pages=180–188 |doi=10.1097/chi.0b013e31815d9af7 |pmid=18182963 |issn=0890-8567}}</ref> but can be useful alternatives or used in conjunction with a stimulant.<ref name="CNS09" /> | |
| | | | |
| | === Exercise === | | === Exercise === |
| − | Regular [[physical exercise]], particularly [[aerobic exercise]], is an effective [[adjunct therapy|add-on treatment]] for ADHD in children and adults, particularly when combined with stimulant medication (although the best intensity and type of aerobic exercise for improving symptoms are not currently known).<ref name="Kamp_2014">{{cite journal |vauthors=Kamp CF, Sperlich B, Holmberg HC |title=Exercise reduces the symptoms of attention-deficit/hyperactivity disorder and improves social behaviour, motor skills, strength and neuropsychological parameters |journal=Acta Paediatrica |volume=103 |issue=7 |pages=709–714 |date=July 2014 |pmid=24612421 |doi=10.1111/apa.12628 |quote=We may conclude that all different types of exercise ... attenuate the characteristic symptoms of ADHD and improve social behaviour, motor skills, strength and neuropsychological parameters without any undesirable side effects. Available reports do not reveal which type, intensity, duration and frequency of exercise is most effective |s2cid=45881887 |url=http://urn.kb.se/resolve?urn=urn:nbn:se:miun:diva-22594|doi-access=free }}</ref> The long-term effects of regular aerobic exercise in ADHD individuals include better behaviour and motor abilities, improved [[executive functions]] (including attention, inhibitory control, and [[planning]], among other cognitive domains), faster [[mental chronometry|information processing speed]], and better memory.<ref name="Rommel_2013">{{cite journal |vauthors=Rommel AS, Halperin JM, Mill J, Asherson P, Kuntsi J |date=September 2013 |title=Protection from genetic diathesis in attention-deficit/hyperactivity disorder: possible complementary roles of exercise |journal=Journal of the American Academy of Child and Adolescent Psychiatry |volume=52 |issue=9 |pages=900–910 |doi=10.1016/j.jaac.2013.05.018 |pmc=4257065 |pmid=23972692 |quote=The findings from these studies provide some support for the notion that exercise has the potential to act as a protective factor for ADHD.}}</ref> Parent-teacher ratings of behavioural and socio-emotional outcomes in response to regular aerobic exercise include: better overall function, reduced ADHD symptoms, better self-esteem, reduced levels of anxiety and depression, fewer somatic complaints, better academic and classroom behaviour, and improved social behaviour. Exercising while on stimulant medication augments the effect of stimulant medication on executive function.<ref name="Den_Heijer_2016">{{cite journal |display-authors=6 |vauthors=Den Heijer AE, Groen Y, Tucha L, Fuermaier AB, Koerts J, Lange KW, Thome J, Tucha O |date=February 2017 |title=Sweat it out? The effects of physical exercise on cognition and behavior in children and adults with ADHD: a systematic literature review |journal=Journal of Neural Transmission |volume=124 |issue=Suppl 1 |pages=3–26 |doi=10.1007/s00702-016-1593-7 |pmc=5281644 |pmid=27400928 |quote=Beneficial chronic effects of cardio exercise were found on various functions as well, including executive functions, attention and behavior.}}</ref> It is believed that these short-term effects of exercise are mediated by an increased abundance of synaptic dopamine and norepinephrine in the brain.<ref name="Den_Heijer_2016" /> | + | Regular [[physical exercise]], particularly [[aerobic exercise]], is an effective [[adjunct therapy|add-on treatment]] for ADHD in children and adults, particularly when combined with stimulant medication. The long-term effects of regular aerobic exercise in ADHD individuals include better behavior and motor abilities, improved [[executive functions]] (including attention, inhibitory control, and [[planning]], among other cognitive domains), faster [[mental chronometry|information processing speed]], and better memory. Parent-teacher ratings in response to regular aerobic exercise include: better overall function, reduced ADHD symptoms, better [[self-estee]]m, reduced levels of anxiety and depression, fewer somatic complaints, better academic and classroom behavior, and improved social behavior.<ref>Anne E Den Heijer et al, [https://pubmed.ncbi.nlm.nih.gov/27400928/ Sweat it out? The effects of physical exercise on cognition and behavior in children and adults with ADHD: a systematic literature review] ''Journal of Neural Transmission'' 124(Suppl 1) (2017):3–26. Retrieved January 22, 2024.</ref> |
| | | | |
| | ==Prognosis== | | ==Prognosis== |
| − | ADHD persists into adulthood in about 30–50% of cases.<ref name="Balint_2008">{{cite journal |vauthors=Bálint S, Czobor P, Mészáros A, Simon V, Bitter I |title=A felnottkori figyelemhiányos/hiperaktivitás-zavarban tapasztalható neuropszichológiai deficit: irodalmi áttekintés |language=hu |journal=Psychiatria Hungarica |volume=23 |issue=5 |pages=324–335 |year=2008 |pmid=19129549 |trans-title=Neuropsychological impairments in adult attention deficit hyperactivity disorder: A literature review |id=[[PsycNET]] [https://psycnet.apa.org/record/2008-18348-001 2008-18348-001] |issn=0237-7896 |publisher=Magyar Pszichiátriai Társaság }}</ref> Those affected are likely to develop coping mechanisms as they mature, thus compensating to some extent for their previous symptoms.<ref name="Art.218" /> Children with ADHD have a higher risk of unintentional injuries.<ref name="Ruiz-Goikoetxea_2017" /> Effects of medication on functional impairment and [[Quality of life (healthcare)|quality of life]] (e.g. reduced risk of accidents) have been found across multiple domains.<ref>{{cite journal |vauthors=Faraone SV, Asherson P, Banaschewski T, Biederman J, Buitelaar JK, Ramos-Quiroga JA, Rohde LA, Sonuga-Barke EJ, Tannock R, Franke B |display-authors=6 |title=Attention-deficit/hyperactivity disorder |journal=Nature Reviews. Disease Primers |volume=1 |page=15020 |date=August 2015 |pmid=27189265 |doi=10.1038/nrdp.2015.20 |s2cid=7171541 |citeseerx=10.1.1.497.1346 |type=Review }}</ref> Rates of smoking among those with ADHD are higher than in the general population at about 40%.<ref>{{cite journal |vauthors=McClernon FJ, Kollins SH |title=ADHD and smoking: from genes to brain to behavior |journal=Annals of the New York Academy of Sciences |volume=1141 |pages=131–147 |date=October 2008 |issue=1 |pmid=18991955 |pmc=2758663 |doi=10.1196/annals.1441.016 |bibcode=2008NYASA1141..131M }}</ref> | + | ADHD is a life-long condition, but for many it is possible to manage symptoms effectively, thus not meet the criteria for ADHD in adulthood. The long-term outlook (prognosis) of ADHD depends on whether treatment is received early on. With behavior therapy and/or medication, most children go on to live healthy lives. However, without treatment, people with ADHD may experience lifelong complications.<ref>[https://my.clevelandclinic.org/health/diseases/4784-attention-deficithyperactivity-disorder-adhd Attention-Deficit/Hyperactivity Disorder (ADHD)] ''Cleveland Clinic''. Retrieved January 22, 2024.</ref> |
| | | | |
| | ==Controversy== | | ==Controversy== |
| − | ADHD, its diagnosis, and its treatment have been controversial since the 1970s.<ref name="May_2008" /><ref name="Foreman_2006">{{cite journal |vauthors=Foreman DM |title=Attention deficit hyperactivity disorder: legal and ethical aspects |journal=Archives of Disease in Childhood |volume=91 |issue=2 |pages=192–194 |date=February 2006 |pmid=16428370 |pmc=2082674 |doi=10.1136/adc.2004.064576 }}</ref> The controversies involve clinicians, teachers, policymakers, parents, and the media. ADHD was officially known as '''attention deficit disorder''' ('''ADD''') from 1980 to 1987; prior to the 1980s, it was known as '''hyperkinetic reaction of childhood'''. | + | ADHD, its diagnosis, and its treatment have been controversial since the 1970s. Controversies involve clinicians, teachers, policymakers, parents, and the media. |
| − | | |
| − | Positions range from the view that ADHD is within the normal range of behavior<ref name="NICE2009-part2" /><ref name="Faraone_2005">{{cite journal |vauthors=Faraone SV |title=The scientific foundation for understanding attention-deficit/hyperactivity disorder as a valid psychiatric disorder |journal=European Child & Adolescent Psychiatry |volume=14 |issue=1 |pages=1–10 |date=February 2005 |pmid=15756510 |s2cid=143646869 |doi=10.1007/s00787-005-0429-z}}</ref> to the hypothesis that ADHD is a genetic condition.<ref>{{cite news |vauthors=Boseley S |date=30 September 2010 |title=Hyperactive children may have genetic disorder, says study |newspaper=The Guardian |url=https://www.theguardian.com/society/2010/sep/30/hyperactive-children-genetic-disorder-study |url-status=live |archive-date=8 July 2017 |archive-url=https://web.archive.org/web/20170708164457/https://www.theguardian.com/society/2010/sep/30/hyperactive-children-genetic-disorder-study}}</ref> Other areas of controversy include the use of stimulant medications in children,<ref name="May_2008" /> the method of diagnosis, and the possibility of overdiagnosis.<ref name="Cormier_2008">{{cite journal |vauthors=Cormier E |title=Attention deficit/hyperactivity disorder: a review and update |journal=Journal of Pediatric Nursing |volume=23 |issue=5 |pages=345–357 |date=October 2008 |pmid=18804015 |doi=10.1016/j.pedn.2008.01.003 }}</ref> In 2009, the National Institute for Health and Care Excellence, while acknowledging the controversy, states that the current treatments and methods of diagnosis are based on the dominant view of the academic literature.<ref name="NICE2009-Diagnosis">{{cite book |title=Attention Deficit Hyperactivity Disorder: Diagnosis and Management of ADHD in Children, Young People and Adults |author=National Collaborating Centre for Mental Health |series=NICE Clinical Guidelines |volume=72 |publisher=British Psychological Society |location=Leicester |isbn=978-1-85433-471-8 |date=2009 |url=https://www.ncbi.nlm.nih.gov/books/NBK53652/ |chapter=Diagnosis |pages=[https://www.ncbi.nlm.nih.gov/books/NBK53659/#ch5.s40 116–7], [https://www.ncbi.nlm.nih.gov/books/NBK53659/#ch5.s42 119] |chapter-url=https://www.ncbi.nlm.nih.gov/books/NBK53659/ |via=NCBI Bookshelf |url-status=live |archive-url=https://web.archive.org/web/20160113133612/http://www.ncbi.nlm.nih.gov/books/NBK53652/ |archive-date=13 January 2016 }}</ref> In 2014, [[Keith Conners]], one of the early advocates for recognition of the disorder, spoke out against overdiagnosis in a ''[[New York Times]]'' article.<ref name="NYT2013">{{cite news |vauthors=Schwarz A |title=The Selling of Attention Deficit Disorder |url=https://www.nytimes.com/2013/12/15/health/the-selling-of-attention-deficit-disorder.html |access-date=26 February 2015 |newspaper=The New York Times |date=14 December 2013 |url-status=live |archive-url=https://web.archive.org/web/20150301054334/http://www.nytimes.com/2013/12/15/health/the-selling-of-attention-deficit-disorder.html |archive-date=1 March 2015}}</ref> In contrast, a 2014 peer-reviewed medical literature review indicated that ADHD is underdiagnosed in adults.<ref name="Ginsberg_2014" />
| |
| | | | |
| − | With widely differing rates of diagnosis across countries, states within countries, races, and ethnicities, some suspect factors other than the presence of the symptoms of ADHD are playing a role in diagnosis, such as cultural norms.<ref name="Elder-2010">{{cite journal | vauthors = Elder TE | title = The importance of relative standards in ADHD diagnoses: evidence based on exact birth dates | journal = Journal of Health Economics | volume = 29 | issue = 5 | pages = 641–656 | date = September 2010 | pmid = 20638739 | pmc = 2933294 | doi = 10.1016/j.jhealeco.2010.06.003 }}</ref><ref name="Ford-Jones_2015">{{cite journal | vauthors = Ford-Jones PC | title = Misdiagnosis of attention deficit hyperactivity disorder: 'Normal behaviour' and relative maturity | journal = Paediatrics & Child Health | volume = 20 | issue = 4 | pages = 200–202 | date = May 2015 | pmid = 26038639 | pmc = 4443828 | doi = 10.1093/pch/20.4.200 }}</ref> Some sociologists consider ADHD to be an example of the [[medicalization]] of deviant behaviour, that is, the turning of the previously {{nowrap|non-medical}} issue of school performance into a medical one.<ref name="Parrillo_2008">{{Cite book |url=https://books.google.com/books?id=mRGr_B4Y1CEC |title=Encyclopedia of Social Problems |vauthors=Parrillo VN |publisher=SAGE |year=2008 |isbn=9781412941655 |page=63 |access-date=2 May 2009 |archive-url=https://web.archive.org/web/20200104002705/https://books.google.com/books?id=mRGr_B4Y1CEC |archive-date=4 January 2020 |url-status=live}}</ref> Most healthcare providers accept ADHD as a genuine disorder, at least in the small number of people with severe symptoms.
| + | Positions range from the view that ADHD is a valid [[Mental disorder|psychiatric disorder]] characterized by behavioral problems,<ref>Stephen V. Faraone, [https://pubmed.ncbi.nlm.nih.gov/15756510/ The scientific foundation for understanding attention-deficit/hyperactivity disorder as a valid psychiatric disorder] ''European Child & Adolescent Psychiatry'' 14(1) (February 2005):1–10. Retrieved January 22, 2024.</ref> possibly a genetic condition,<ref name=Sarah>Sarah Boseley, [https://www.theguardian.com/society/2010/sep/30/hyperactive-children-genetic-disorder-study Hyperactive children may suffer from genetic disorder, says study] ''The Guardian'' (September 29, 2010). Retrieved January 22, 2024.</ref> to blaming parents for poorly disciplining their children or feeding them too much sugar,<ref name=Sarah/> or regarding it as one end of a normal continuum of a set of centrally important cognitive and behavioral traits, and thus "treatment" being understood as enhancing performance to improve functioning rather than correcting the effects of a disorder.<ref>Ralph Lewis, [https://www.psychologytoday.com/us/blog/finding-purpose/202101/is-adhd-real-disorder-or-one-end-normal-continuum Is ADHD a Real Disorder or One End of a Normal Continuum?] ''Psychology Today'' (January 6, 2021). Retrieved January 22, 2024.</ref> |
| | + | |
| | + | Other areas of controversy include the use of stimulant medications in children, the method of diagnosis, and the possibility of overdiagnosis.<ref name="Cormier_2008">Eileen Cormier, [https://pubmed.ncbi.nlm.nih.gov/18804015/ Attention deficit/hyperactivity disorder: a review and update] ''Journal of Pediatric Nursing'' 23(5) (October 2008):345-357. Retrieved January 22, 2024.</ref> On the other hand, a 2014 peer-reviewed medical literature review indicated that ADHD is under-diagnosed in adults.<ref>Ylva Ginsberg, Javier Quintero,Ernie Anand, Marta Casillas, and Himanshu P. Upadhyaya, [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4195639/ Underdiagnosis of Attention-Deficit/Hyperactivity Disorder in Adult Patients: A Review of the Literature] ''The Primary Care Companion for CNS Disorders'' 16(3) (2014). Retrieved January 22, 2024. </ref> |
| | | | |
| | + | Numerous factors intrinsic to a child or youth can affect their diagnosis of ADHD including, gender, age, race, and socioeconomic status, in addition to the severity of symptoms. With widely differing rates of diagnosis across countries, states within countries, races, and ethnicities, some suspect factors other than the presence of the symptoms of ADHD are playing a role in diagnosis, such as cultural norms. Multiple individuals have significant impact in the identification and diagnosis of ADHD including parents, healthcare providers, and teachers, and aspects of the environment. Their different cultural and ethnic backgrounds may lead to different views and perceptions of behavioral norms and when to consider behavior inappropriate or indicative of a clinical disorder such as ADHD.<ref>Alaa M. Hamed, Aaron J. Kauer, and Hanna E. Stevens, [https://www.frontiersin.org/articles/10.3389/fpsyt.2015.00168/full Why the Diagnosis of Attention Deficit Hyperactivity Disorder Matters] ''Frontiers in Psychiatry'' 6 (November 26, 2015). Retrieved January 22, 2024.</ref> |
| | | | |
| − | ADHD is now a well-validated clinical diagnosis in children and adults, and the debate in the scientific community mainly centers on how it is diagnosed and treated.<ref name="Silver_2004">{{cite book |vauthors=Silver LB |title=Attention-deficit/hyperactivity disorder |publisher=American Psychiatric Publishing |edition=3rd |year=2004 |isbn=978-1-58562-131-6 |pages=4–7 }}</ref><ref name="Schonwald_2006">{{cite journal |vauthors=Schonwald A, Lechner E |title=Attention deficit/hyperactivity disorder: complexities and controversies |journal=Current Opinion in Pediatrics |volume=18 |issue=2 |pages=189–195 |date=April 2006 |pmid=16601502 |doi=10.1097/01.mop.0000193302.70882.70 |s2cid=27286123 }}</ref> | + | ADHD is now a well-validated clinical diagnosis in children and adults, and debate in the scientific community mainly concerns how it is diagnosed and treated.<ref> Larry B. Silver, ''Attention-Deficit/Hyperactivity Disorder: A Clinical Guide to Diagnosis and Treatment for Health and Mental Health Professionals'' (American Psychiatric Association Publishing, 2003, ISBN 978-1585621316). </ref> |
| | | | |
| | == Notes == | | == Notes == |
| Line 259: |
Line 244: |
| | * Dulcan, Mina K., Rachel R. Ballard, Poonam Jha, and Julie M. Sadhu. ''Concise Guide to Child and Adolescent Psychiatry''. American Psychiatric Publishing, 2017. ISBN 978-1615370788 | | * Dulcan, Mina K., Rachel R. Ballard, Poonam Jha, and Julie M. Sadhu. ''Concise Guide to Child and Adolescent Psychiatry''. American Psychiatric Publishing, 2017. ISBN 978-1615370788 |
| | * Millichap, J. Gordon. ''Attention Deficit Hyperactivity Disorder Handbook''. Springer, 2009. ISBN 978-1441913968 | | * Millichap, J. Gordon. ''Attention Deficit Hyperactivity Disorder Handbook''. Springer, 2009. ISBN 978-1441913968 |
| | + | * Nolen-Hoeksema, Susan. ''Abnormal Psychology''. McGraw Hill, 2022. ISBN 978-1265237769 |
| | * Ramsay, J. Russell, and Anthony L. Rostain. ''Cognitive-Behavioral Therapy for Adult ADHD: An Integrative Psychosocial and Medical Approach''. Routledge, 2007. ISBN 978-0415955010 | | * Ramsay, J. Russell, and Anthony L. Rostain. ''Cognitive-Behavioral Therapy for Adult ADHD: An Integrative Psychosocial and Medical Approach''. Routledge, 2007. ISBN 978-0415955010 |
| | + | * Silver, Larry B. ''Attention-Deficit/Hyperactivity Disorder: A Clinical Guide to Diagnosis and Treatment for Health and Mental Health Professionals''. American Psychiatric Association Publishing, 2003. ISBN 978-1585621316 |
| | * Weiss, Margaret, Lily Trokenberg Hechtman, and Gabrielle Weiss. ''ADHD in Adulthood: A Guide to Current Theory, Diagnosis, and Treatment''. Johns Hopkins University Press, 2001. ISBN 978-0801868221 | | * Weiss, Margaret, Lily Trokenberg Hechtman, and Gabrielle Weiss. ''ADHD in Adulthood: A Guide to Current Theory, Diagnosis, and Treatment''. Johns Hopkins University Press, 2001. ISBN 978-0801868221 |
| | * Wiener, Jerry M., and Mina K. Dulcan (eds.). ''Textbook Of Child and Adolescent Psychiatry''. American Psychiatric Publishing, 2003. ISBN 978-1585620579 | | * Wiener, Jerry M., and Mina K. Dulcan (eds.). ''Textbook Of Child and Adolescent Psychiatry''. American Psychiatric Publishing, 2003. ISBN 978-1585620579 |
| Line 265: |
Line 252: |
| | | | |
| | == External links == | | == External links == |
| − | All links retrieved | + | All links retrieved January 22, 2024. |
| | | | |
| | * [https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd Attention-Deficit/Hyperactivity Disorder] ''National Institute of Mental Health'' (NIMH) | | * [https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd Attention-Deficit/Hyperactivity Disorder] ''National Institute of Mental Health'' (NIMH) |
| Line 273: |
Line 260: |
| | * [https://www.healthline.com/health/adhd Everything You Need to Know About ADHD] ''HealthLine'' | | * [https://www.healthline.com/health/adhd Everything You Need to Know About ADHD] ''HealthLine'' |
| | * [https://www.hopkinsmedicine.org/health/conditions-and-diseases/adhdadd Attention-Deficit / Hyperactivity Disorder (ADHD) in Children] ''Johns Hopkins Medicine'' | | * [https://www.hopkinsmedicine.org/health/conditions-and-diseases/adhdadd Attention-Deficit / Hyperactivity Disorder (ADHD) in Children] ''Johns Hopkins Medicine'' |
| | + | * [https://my.clevelandclinic.org/health/diseases/4784-attention-deficithyperactivity-disorder-adhd Attention-Deficit/Hyperactivity Disorder (ADHD)] ''Cleveland Clinic'' |
| | * [https://icd.who.int/browse11/l-m/en#/http%3A%2F%2Fid.who.int%2Ficd%2Fentity%2F821852937 6A05 Attention deficit hyperactivity disorder] ''ICD-11'' | | * [https://icd.who.int/browse11/l-m/en#/http%3A%2F%2Fid.who.int%2Ficd%2Fentity%2F821852937 6A05 Attention deficit hyperactivity disorder] ''ICD-11'' |
| | | | |
| Attention Deficit Hyperactivity Disorder
|
|
| Symptoms | Inattention, carelessness, hyperactivity, executive dysfunction, disinhibition, emotional dysregulation, impulsivity, impaired working memory |
|---|
| Usual onset | Symptoms should onset in developmental period unless ADHD occurred after traumatic brain injury (TBI). |
|---|
| Causes | Genetic (inherited, de novo) and to a lesser extent, environmental factors (exposure to biohazards during pregnancy, traumatic brain injury) |
|---|
| Diagnostic method | Based on symptoms after other possible causes have been ruled out |
|---|
| Differential diagnosis | Normally active child, bipolar disorder, cognitive disengagement syndrome, conduct disorder, major depressive disorder, autism spectrum disorder, oppositional defiant disorder, learning disorder, intellectual disability, anxiety disorder, borderline personality disorder, fetal alcohol spectrum disorder |
|---|
| Treatment | Psychotherapy, lifestyle changes, medication |
|---|
| Medication | CNS stimulants (methylphenidate, amphetamine), non-stimulants (atomoxetine, viloxazine), alpha-2a agonists (guanfacine XR, clonidine XR) |
|---|
| Frequency | 0.8–1.5% |
|---|
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by executive dysfunction occasioning symptoms of inattention, hyperactivity, impulsivity and emotional dysregulation that are excessive and pervasive, impairing in multiple contexts, and otherwise age-inappropriate. Although people with ADHD struggle to sustain attention on tasks that entail delayed rewards or consequences, they are often able to maintain an unusually prolonged and intense level of attention for tasks they do find interesting or rewarding; this is known as hyperfocus.
ADHD, its diagnosis, and its treatment have been considered controversial since the 1970s, with issues including over-diagnosis, use of stimulants as treatment for children, as well as disagreements on the nature of the disorder. ADHD is now a well-validated clinical diagnosis in children and adults, and the debate in the scientific community mainly centers on how it is diagnosed and treated. ADHD management recommendations usually involve some combination of medications, counseling, and lifestyle changes. For the majority of individuals, such treatment enables them to live productive and fulfilling lives.
History
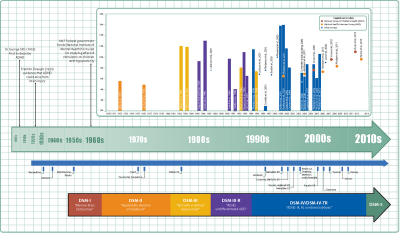
Timeline of ADHD diagnostic criteria, prevalence, and treatment
[1]Hyperactivity has long been part of the human condition. Sir Alexander Crichton described "mental restlessness" in his book An Inquiry Into The Nature And Origin Of Mental Derangement written in 1798. He made observations about children showing signs of being inattentive and having the "fidgets."[2]
The first clear description of ADHD is credited to George Still in 1902 during a series of lectures he gave to the Royal College of Physicians of London.[3] He noted that both nature and nurture could be influencing this disorder.
The terminology used to describe the condition has changed over time.
Prior to the DSM, terms included minimal brain damage in the 1930s.[4] Other terms include: minimal brain dysfunction in the DSM-I (1952), hyperkinetic reaction of childhood in the DSM-II (1968), and attention-deficit disorder with or without hyperactivity in the DSM-III (1980).[1] In 1987, this was changed to Attention deficit hyperactivity disorder (ADHD) in the DSM-III-R, and in 1994 the DSM-IV in split the diagnosis into three subtypes: ADHD inattentive type, ADHD hyperactive-impulsive type, and ADHD combined type.[5] These terms were kept in the DSM-5 in 2013[6] and in the DSM-5-TR in 2022.[7]
Signs and symptoms
ADHD is characterized by symptoms of inattention, hyperactivity, impulsivity, and emotional dysregulation that are excessive and pervasive, impairing in multiple contexts, and otherwise age-inappropriate.[6][7][8] The signs and symptoms can be difficult to define, as it is hard to draw a line at where normal levels of inattention, hyperactivity, and impulsivity end and significant levels requiring interventions begin.[9]
In children, problems paying attention may result in poor school performance. ADHD is associated with other neurodevelopmental and mental disorders as well as some non-psychiatric disorders, which can cause additional impairment, especially in modern society. Although people with ADHD struggle to sustain attention on tasks that entail delayed rewards or consequences, they are often able to maintain an unusually prolonged and intense level of attention for tasks they do find interesting or rewarding; this is known as hyperfocus.
Inattention, hyperactivity (restlessness in adults), disruptive behavior, and impulsivity are common in ADHD. Academic difficulties are frequent as are problems with relationships.[10] Elevated accident-proneness has been found in ADHD patients.[11]
Significantly more males than females are diagnosed with ADHD. It has been suggested that this could be due to gender differences in how ADHD presents. Boys and men tend to display more hyperactive and impulsive behavior while girls and women are more likely to have inattentive symptoms. There are also gender differences in how these symptomatic and behavioral differences are manifested.[12]
Symptoms are expressed differently and more subtly as the individual ages:
Whereas the core symptoms of hyperactivity, impulsivity and inattention, are well characterised in children, these symptoms may have different and more subtle expressions in adult life. [13]
Hyperactivity tends to become less overt with age and turns into inner restlessness, difficulty relaxing or remaining still, talkativeness or constant mental activity in teens and adults with ADHD:
For instance, where children with ADHD may run and climb excessively, or have difficulty in playing or engaging quietly in leisure activities, adults with ADHD are more likely to experience inner restlessness, inability to relax, or over talkativeness. Hyperactivity may also be expressed as excessive fidgeting, the inability to sit still for long in situations when sitting is expected (at the table, in the movie, in church or at symposia), or being on the go all the time. ... For example, physical overactivity in children could be replaced in adulthood by constant mental activity, feelings of restlessness and difficulty engaging in sedentary activities.[13]
Impulsivity in adulthood may appear as thoughtless behavior, impatience, irresponsible spending and sensation-seeking behaviors, while inattention may appear as becoming easily bored, difficulty with organization, remaining on task and making decisions, and sensitivity to stress:
Impulsivity may be expressed as impatience, acting without thinking, spending impulsively, starting new jobs and relationships on impulse, and sensation seeking behaviours. ... Inattention often presents as distractibility, disorganization, being late, being bored, need for variation, difficulty making decisions, lack of overview, and sensitivity to stress.[13]
Although not listed as an official symptom for this condition, emotional dysregulation or mood lability is generally understood to be a common symptom of ADHD.[13]
Diagnosis
ADHD is diagnosed by an assessment of a person's behavioral and mental development, including ruling out the effects of drugs, medications, and other medical or psychiatric problems as explanations for the symptoms. ADHD diagnosis often takes into account feedback from parents and teachers.[14]
In North America and Australia, the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders (currently DSM-5) criteria are used for diagnosis, while European countries usually use the World Health Organization's International Classification of Diseases (currently ICD-11). ADHD is alternately classified as neurodevelopmental disorder[15] or a disruptive behavior disorder along with Oppositional defiant disorder (ODD), Conduct disorder (CD), and antisocial personality disorder.[16]
Self-rating scales, such as the ADHD rating scale and the Vanderbilt ADHD diagnostic rating scale, are used in the screening and evaluation of ADHD.[17]
Classification
ADHD is divided into three primary presentations:
- predominantly inattentive (ADHD-PI or ADHD-I)
- predominantly hyperactive-impulsive (ADHD-PH or ADHD-HI)
- combined presentation (ADHD-C).
The table below lists the symptoms for ADHD-I and ADHD-HI from the two major classification systems. Symptoms which can be better explained by another psychiatric or medical condition which an individual has are not considered to be a symptom of ADHD for that person.
Symptoms
| Presentations
|
DSM-5[6] and DSM-5-TR[7] symptoms
|
ICD-11[8] symptoms
|
| Inattention
|
Six or more of the following symptoms in children, and five or more in adults, excluding situations where these symptoms are better explained by another psychiatric or medical condition:
- Frequently overlooks details or makes careless mistakes
- Often has difficulty maintaining focus on one task or play activity
- Often appears not to be listening when spoken to, including when there is no obvious distraction
- Frequently does not finish following instructions, failing to complete tasks
- Often struggles to organize tasks and activities, to meet deadlines, and to keep belongings in order
- Is frequently reluctant to engage in tasks which require sustained attention
- Frequently loses items required for tasks and activities
- Is frequently easily distracted by extraneous stimuli, including thoughts in adults and older teenagers
- Often forgets daily activities, or is forgetful while completing them.
|
Multiple symptoms of inattention that directly negatively impact occupational, academic or social functioning. Symptoms may not be present when engaged in highly stimulating tasks with frequent rewards. Symptoms are generally from the following clusters:
- Struggles to maintain focus on tasks that aren't highly stimulating/rewarding or that require continuous effort; details are often missed, and careless mistakes are frequent in school and work tasks; tasks are often abandoned before they are completed.
- Easily distracted (including by own thoughts); may not listen when spoken to; frequently appears to be lost in thought
- Often loses things; is forgetful and disorganized in daily activities.
The individual may also meet the criteria for hyperactivity-impulsivity, but the inattentive symptoms are predominant.
|
| Hyperactivity-Impulsivity
|
Six or more of the following symptoms in children, and five or more in adults, excluding situations where these symptoms are better explained by another psychiatric or medical condition:
- Is often fidgeting or squirming in seat
- Frequently has trouble sitting still during dinner, class, in meetings, etc.
- Frequently runs around or climbs in inappropriate situations. In adults and teenagers, this may be present only as restlessness.
- Often cannot quietly engage in leisure activities or play
- Frequently seems to be "on the go" or appears uncomfortable when not in motion
- Often talks excessively
- Often answers a question before it is finished, or finishes people's sentences
- Often struggles to wait their turn, including waiting in lines
- Frequently interrupts or intrudes, including into others' conversations or activities, or by using people's things without asking.
|
Multiple symptoms of hyperactivity/impulsivity that directly negatively impact occupational, academic or social functioning. Typically, these tend to be most apparent in environments with structure or which require self-control. Symptoms are generally from the following clusters:
- Excessive motor activity; struggles to sit still, often leaving their seat; prefers to run about; in younger children, will fidget when attempting to sit still; in adolescents and adults, a sense of physical restlessness or discomfort with being quiet and still.
- Talks too much; struggles to quietly engage in activities.
- Blurts out answers or comments; struggles to wait their turn in conversation, games, or activities; will interrupt or intrude on conversations or games.
- A lack of forethought or consideration of consequences when making decisions or taking action, instead tending to act immediately (e.g., physically dangerous behaviours including reckless driving; impulsive decisions).
The individual may also meet the criteria for inattention, but the hyperactive-impulsive symptoms are predominant.
|
| Combined
|
Meet the criteria for both inattentive and hyperactive-impulsive ADHD.
|
Criteria are met for both inattentive and hyperactive-impulsive ADHD, with neither clearly predominating.
|
DSM-5
As with many other psychiatric disorders, a formal diagnosis should be made by a qualified professional based on a set number of criteria. In the United States, these criteria are defined by the American Psychiatric Association in the DSM. Based on the DSM-5 criteria published in 2013 and the DSM-5-TR criteria published in 2022, there are three presentations of ADHD:
- ADHD, predominantly inattentive type, presents with symptoms including being easily distracted, forgetful, daydreaming, disorganization, poor concentration, and difficulty completing tasks.
- ADHD, predominantly hyperactive-impulsive type, presents with excessive fidgeting and restlessness, hyperactivity, and difficulty waiting and remaining seated.
- ADHD, combined type, a combination of the first two presentations.
Symptoms must be present for six months or more to a degree that is much greater than others of the same age. This requires at least six symptoms of either inattention or hyperactivity/impulsivity for those under 17 and at least five symptoms for those 17 years or older. The symptoms must be present in at least two settings (such as social, school, work, or home), and must directly interfere with or reduce quality of functioning.[6] Additionally, several symptoms must have been present before age twelve.[7]
The DSM-5 and the DSM-5-TR also provide two diagnoses for individuals who have symptoms of ADHD but do not entirely meet the requirements. Other Specified ADHD allows the clinician to describe why the individual does not meet the criteria, whereas Unspecified ADHD is used where the clinician chooses not to describe the reason.
ICD-11
In the eleventh revision of the World Health Organization's ICD-11, the disorder is classified as Attention deficit hyperactivity disorder (code 6A05). The defined subtypes are similar to those of the DSM-5: predominantly inattentive presentation (6A05.0); predominantly hyperactive-impulsive presentation(6A05.1); combined presentation (6A05.2). The ICD-11 also includes the two residual categories for individuals who do not entirely match any of the defined subtypes: other specified presentation (6A05.Y) where the clinician includes detail on the individual's presentation; and presentation unspecified (6A05.Z) where the clinician does not provide detail.[8]
Adults
Adults with ADHD are diagnosed under the same criteria as children, including that their signs must have been present by the age of six to twelve. The individual is the best source for information in diagnosis, however others may provide useful information about the individual's symptoms currently and in childhood; a family history of ADHD also adds weight to a diagnosis.
While the core symptoms of ADHD are similar in children and adults, they often present differently: Excessive physical activity seen in children may present as feelings of restlessness and constant mental activity in adults. Adults with ADHD may start relationships impulsively, display sensation-seeking behaviour, and be short-tempered. Addictive behavior such as substance abuse and gambling are common.[13]
Differential diagnosis
The DSM provides potential differential diagnoses – potential alternate explanations for specific symptoms. Assessment and investigation of clinical history determines which is the most appropriate diagnosis. The DSM-5 suggests ODD, intermittent explosive disorder, and other neurodevelopmental disorders (such as stereotypic movement disorder and Tourette's disorder), in addition to specific learning disorder, intellectual developmental disorder, ASD, reactive attachment disorder, anxiety disorders, depressive disorders, bipolar disorder, disruptive mood dysregulation disorder, substance use disorder, personality disorders, psychotic disorders, medication-induced symptoms, and neurocognitive disorders. Many but not all of these are also common comorbidities of ADHD.[6] The DSM-5-TR also suggests post-traumatic stress disorder.[7]
Primary sleep disorders may affect attention and behavior and the symptoms of ADHD may affect sleep. It is thus recommended that children with ADHD be regularly assessed for sleep problems. Sleepiness in children may result in symptoms ranging from the classic ones of yawning and rubbing the eyes, to hyperactivity and inattentiveness. Obstructive sleep apnea can also cause ADHD-type symptoms.
Comorbidities
Psychiatric
Various neurodevelopmental conditions are common comorbidities. Autism spectrum disorder (ASD) and ADHD can be diagnosed in the same person.[7] ADHD is not considered a learning disability, but it very frequently causes academic difficulties and Intellectual disabilities.[7]
ADHD is often comorbid with disruptive, impulse control, and conduct disorders. Oppositional defiant disorder (ODD), characterized by angry or irritable mood, argumentative or defiant behavior and vindictiveness which are age-inappropriate, occurs in about 25 percent of children with an inattentive presentation and 50 percent of those with a combined presentation. Conduct disorder (CD), characterized by aggression, destruction of property, deceitfulness, theft and violations of rules, occurs in about 25 percent of adolescents with ADHD.[7]
Anxiety disorders have been found to occur more commonly in the ADHD population, as have mood disorders (especially bipolar disorder and major depressive disorder).
Sleep disorders and ADHD commonly co-exist. However, they can also occur as a side effect of medications used to treat ADHD.
There are other psychiatric conditions which are often co-morbid with ADHD, such as substance use disorders, commonly seen with alcohol or cannabis.[13] Other psychiatric conditions include reactive attachment disorder and eating disorders.
Trauma
ADHD, trauma, and Adverse Childhood Experiences are also comorbid, which could in part be potentially explained by the similarity in presentation between different diagnoses. The symptoms of ADHD and PTSD can have significant behavioral overlap—in particular, motor restlessness, difficulty concentrating, distractibility, irritability/anger, emotional constriction or dysregulation, poor impulse control, and forgetfulness are common in both.
Non-psychiatric
Some non-psychiatric conditions are also comorbidities of ADHD. This includes epilepsy, a neurological condition characterized by recurrent seizures. There are well established associations between ADHD and obesity, asthma and sleep disorders. Children with ADHD have a higher risk for migraine headaches, but have no increased risk of tension-type headaches. In addition, children with ADHD may also experience headaches as a result of medication.
Suicide risk
Systematic reviews conducted in 2017 and 2020 found strong evidence that ADHD is associated with increased suicide risk across all age groups, as well as growing evidence that an ADHD diagnosis in childhood or adolescence represents a significant future suicidal risk factor. However, the relationship between ADHD and suicidal spectrum behaviors remains unclear. There is no clear data on whether there is a direct relationship between ADHD and suicidality, or whether ADHD increases suicide risk through comorbidities.[18]
Causes
The precise causes of ADHD are unknown in the majority of cases. For most people with ADHD, many genetic and environmental risk factors accumulate to cause the disorder. The environmental risks for ADHD most often exert their influence in the early prenatal period.
Genetics
Family, twin, and adoption studies show that ADHD runs in families, with an average heritability of 74 percent.[19] The siblings of children with ADHD are three to four times more likely to develop the disorder than siblings of children without the disorder.[20]
There are multiple gene variants which each slightly increase the likelihood of a person having ADHD; it is polygenic and arises through the combination of many gene variants which each have a small effect.[19]
For genetic variation to be used as a tool for diagnosis, more validating studies need to be performed.
Environment
In addition to genetics, environmental factors might play a role in ADHD development.causing ADHD.[21]
Environmental risk factors that have been identified as risk factors for ADHD include:[22]
- Maternal smoking, alcohol consumption, and drug use during pregnancy
- Premature birth, or a low birth weight
- Environmental toxins, including exposure to lead and pesticides, and air pollution
- Some illnesses, such as bacterial diseases (such as encephalitis)
Studies have shown a relationship between media use and ADHD-related behaviors.[23] In October 2018, PNAS USA published a systematic review of four decades of research on the relationship between children and adolescents' screen media use and ADHD-related behaviors and concluded that a statistically small relationship between children's media use and ADHD-related behaviors exists.[24]
Pathophysiology
Brain structure
Once neuroimaging studies became possible, studies conducted in the 1990s provided support for the pre-existing theory that neurological differences - particularly in the frontal lobes - were involved in ADHD.
In children with ADHD, there is a general reduction of volume in certain brain structures, with a proportionally greater decrease in the volume in the left-sided prefrontal cortex.[25] Other brain structures in the prefrontal-striatal-cerebellar and prefrontal-striatal-thalamic circuits have also been found to differ between people with and without ADHD, while the subcortical volumes of the accumbens, amygdala, caudate, hippocampus, and putamen appears smaller in individuals with ADHD compared with controls.[26] Structural MRI studies have also revealed differences in white matter, with marked differences in inter-hemispheric asymmetry between ADHD and typically developing youths.[27]
Function MRI (fMRI) studies have revealed a number of differences between ADHD and control brains. Mirroring what is known from structural findings, fMRI studies have shown evidence for a higher connectivity between subcortical and cortical regions, such as between the caudate and prefrontal cortex. The degree of hyperconnectivity between these regions correlated with the severity of inattention or hyperactivity [28]
Executive function
The symptoms of ADHD arise from a deficiency in certain executive functions - the cognitive processes that are required to successfully select and monitor behaviors that facilitate the attainment of one's chosen goals. The executive function impairments that occur in ADHD individuals result in problems with staying organized, time keeping, excessive procrastination, maintaining concentration, paying attention, ignoring distractions, regulating emotions, and remembering details. Due to the rates of brain maturation and the increasing demands for executive control as a person gets older, ADHD impairments may not fully manifest themselves until adolescence or even early adulthood.[29] Conversely, brain maturation trajectories, potentially exhibiting diverging longitudinal trends in ADHD, may support a later improvement in executive functions after reaching adulthood.
ADHD has also been associated with motivational deficits in children. Children with ADHD often find it difficult to focus on long-term over short-term rewards, and exhibit impulsive behavior for short-term rewards.[30]
Paradoxical reaction
Another sign of the structurally altered signal processing in the central nervous system in this group of people is the conspicuously common Paradoxical reaction. These are unexpected reactions to a chemical substance, such as a medical drug, that is opposite to what would usually be expected, or an otherwise significantly different reactions. They may occur with neuroactive substances such as local anesthetic at the dentist, sedative, caffeine, antihistamine, weak neuroleptics, and central and peripheral painkillers.
Management
While there is no cure for ADHD, it is possible to reduce symptoms and improve functioning. ADHD management recommendations vary and usually involve some combination of medications, counseling, education or training, and lifestyle changes.[31] The British guideline emphasizes environmental modifications and education about ADHD for individuals and carers as the first response. If symptoms persist, parent-training, medication, or psychotherapy (especially cognitive behavioral therapy) can be recommended based on age.[32] Canadian and American guidelines recommend medications and behavioral therapy together, except in preschool-aged children for whom the first-line treatment is behavioral therapy alone.[33] [34]
Behavioral therapies
Behavioral therapies are the recommended first-line treatment in those who have mild symptoms or who are preschool-aged, and there is strong evidence for their effectiveness. Psychological therapies used include: psychoeducational input, behavior therapy, cognitive behavioral therapy, interpersonal psychotherapy, family therapy, school-based interventions, social skills training, behavioral peer intervention, organization training, and parent management training.[32]
Parent training may improve a number of behavioral problems including oppositional and non-compliant behaviors. Social skills training, behavioral modification, and medication may have some limited beneficial effects in peer relationships.
Medication
The use of stimulants to treat ADHD was first described in 1937: Charles Bradley gave "problem" children Benzedrine to alleviate headaches and found it unexpectedly improved their school performance, social interactions, and emotional responses. Although Bradley's studies were basically ignored for nearly 25 years, they were an important precursor to studies of amphetamines like Ritalin and their use in managing ADHD.[35]
Stimulants
Methylphenidate and amphetamine or its derivatives are often first-line treatments for ADHD.[36] Studies show that amphetamine is slightly-to-modestly more effective than methylphenidate at reducing symptoms.[37]
Non-stimulants
Two non-stimulant medications, atomoxetine and viloxazine, are approved by the FDA and in other countries for the treatment of ADHD. They produce comparable efficacy and tolerability to methylphenidate, but all three tend to be modestly more tolerable and less effective than amphetamines.
Two alpha-2a agonists, extended-release formulations of guanfacine and clonidine, are approved by the FDA and in other countries for the treatment of ADHD (effective in children and adolescents but effectiveness has still not been shown for adults). They appear to be modestly less effective than the stimulants (amphetamine and methylphenidate) and non-stimulants (atomoxetine and viloxazine) at reducing symptoms, but can be useful alternatives or used in conjunction with a stimulant.[38]
Exercise
Regular physical exercise, particularly aerobic exercise, is an effective add-on treatment for ADHD in children and adults, particularly when combined with stimulant medication. The long-term effects of regular aerobic exercise in ADHD individuals include better behavior and motor abilities, improved executive functions (including attention, inhibitory control, and planning, among other cognitive domains), faster information processing speed, and better memory. Parent-teacher ratings in response to regular aerobic exercise include: better overall function, reduced ADHD symptoms, better self-esteem, reduced levels of anxiety and depression, fewer somatic complaints, better academic and classroom behavior, and improved social behavior.[39]
Prognosis
ADHD is a life-long condition, but for many it is possible to manage symptoms effectively, thus not meet the criteria for ADHD in adulthood. The long-term outlook (prognosis) of ADHD depends on whether treatment is received early on. With behavior therapy and/or medication, most children go on to live healthy lives. However, without treatment, people with ADHD may experience lifelong complications.[40]
Controversy
ADHD, its diagnosis, and its treatment have been controversial since the 1970s. Controversies involve clinicians, teachers, policymakers, parents, and the media.
Positions range from the view that ADHD is a valid psychiatric disorder characterized by behavioral problems,[41] possibly a genetic condition,[42] to blaming parents for poorly disciplining their children or feeding them too much sugar,[42] or regarding it as one end of a normal continuum of a set of centrally important cognitive and behavioral traits, and thus "treatment" being understood as enhancing performance to improve functioning rather than correcting the effects of a disorder.[43]
Other areas of controversy include the use of stimulant medications in children, the method of diagnosis, and the possibility of overdiagnosis.[44] On the other hand, a 2014 peer-reviewed medical literature review indicated that ADHD is under-diagnosed in adults.[45]
Numerous factors intrinsic to a child or youth can affect their diagnosis of ADHD including, gender, age, race, and socioeconomic status, in addition to the severity of symptoms. With widely differing rates of diagnosis across countries, states within countries, races, and ethnicities, some suspect factors other than the presence of the symptoms of ADHD are playing a role in diagnosis, such as cultural norms. Multiple individuals have significant impact in the identification and diagnosis of ADHD including parents, healthcare providers, and teachers, and aspects of the environment. Their different cultural and ethnic backgrounds may lead to different views and perceptions of behavioral norms and when to consider behavior inappropriate or indicative of a clinical disorder such as ADHD.[46]
ADHD is now a well-validated clinical diagnosis in children and adults, and debate in the scientific community mainly concerns how it is diagnosed and treated.[47]
Notes
- ↑ 1.0 1.1 ADHD Throughout the Years Center For Disease Control and Prevention. Retrieved January 19, 2024.
- ↑ Sir Alexander Crichton, An Inquiry Into The Nature And Origin Of Mental Derangement (Legare Street Press, 2022 (original 1798), ISBN 978-1017488913).
- ↑ George Still, The Goulstonian Lectures on some Abnormal Psychical Conditions in Children The Lancet 159(4102) (April 12, 1902):1008-1013. Retrieved January 19, 2024.
- ↑ Margaret Weiss, Lily Trokenberg Hechtman, and Gabrielle Weiss, ADHD in Adulthood: A Guide to Current Theory, Diagnosis, and Treatment (Johns Hopkins University Press, 2001, ISBN 978-0801868221).
- ↑ J. Gordon Millichap, Attention Deficit Hyperactivity Disorder Handbook (Springer, 2009, ISBN 978-1441913968).
- ↑ 6.0 6.1 6.2 6.3 6.4 American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5 (American Psychiatric Publishing, 2013, ISBN 978-0890425541).
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition Text Revision: DSM-5-TR (American Psychiatric Publishing, 2022, ISBN 0890425760).
- ↑ 8.0 8.1 8.2 6A05 Attention deficit hyperactivity disorder ICD-11. Retrieved January 20, 2024.
- ↑ J. Russell Ramsay and Anthony L. Rostain, Cognitive-Behavioral Therapy for Adult ADHD: An Integrative Psychosocial and Medical Approach (Routledge, 2007, ISBN 978-0415955010).
- ↑ What is ADHD? Centers for Disease Control and Prevention. Retrieved January 21, 2024.
- ↑ Nathalie Brunkhorst-Kanaan, Berit Libutzki, Andreas Reif, Henrik Larsson, Rhiannon V. McNeill, and Sarah Kittel-Schneider, ADHD and accidents over the life span – A systematic review Neuroscience & Biobehavioral Reviews (125) (2021):582–591. Retrieved January 19, 2024.
- ↑ Female vs Male ADHD The ADHD Centre (December 21, 2022). Retrieved January 19, 2024.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 European consensus statement on diagnosis and treatment of adult ADHD: The European Network Adult ADHD BMC Psychiatry 10(67) (2010). Retrieved January 20, 2024.
- ↑ Mina K. Dulcan, Rachel R. Ballard, Poonam Jha, and Julie M. Sadhu, Concise Guide to Child and Adolescent Psychiatry (American Psychiatric Publishing, 2017, ISBN 978-1615370788).
- ↑ Caroline S. Clauss-Ehlers, Encyclopedia of Cross-Cultural School Psychology (Springer, 2010, ISBN 978-0387717982).
- ↑ Jerry M. Wiener and Mina K. Dulcan (eds.), Textbook Of Child and Adolescent Psychiatry (American Psychiatric Publishing, 2003, ISBN 978-1585620579).
- ↑ Eric A. Youngstrom, Mitchell J. Prinstein, Eric J. Mash, and Russell A. Barkley (eds.), Assessment of Disorders in Childhood and Adolescence (The Guilford Press, 2020, ISBN 978-1462543632).
- ↑ P. Garas and J. Balazs, Long-Term Suicide Risk of Children and Adolescents With Attention Deficit and Hyperactivity Disorder-A Systematic Review, Frontiers in Psychiatry 11 (December 21, 2020):557909.
- ↑ 19.0 19.1 Stephen V. Faraone and Henrik Larsson, Genetics of attention deficit hyperactivity disorder Molecular Psychiatry 24(4) (2019):562–575. Retrieved January 22, 2024.
- ↑ Susan Nolen-Hoeksema, Abnormal Psychology (McGraw Hill, 2022, ISBN 978-1265237769).
- ↑ Research on ADHD Centers for Disease Control and Prevention. Retrieved January 22, 2024.
- ↑ Exploring the Links Between ADHD and Environmental Factors The ADHD Centre (July 13, 2023). Retrieved January 22, 2024.
- ↑ S.W.C. Nikkelen, P.M. Valkenburg, Mariëtte Huizinga, and B.J. Bushman, Media use and ADHD-related behaviors in children and adolescents: A meta-analysis Developmental Psychology 50(9) (2014):2228–2241. Retrieved January 22, 2024.
- ↑ Ine Beyens, Patti M, Valkenburg, and Jessica Taylor Piotrowski, Screen media use and ADHD-related behaviors: Four decades of researchProceedings of the National Academy of Sciences of the United States of America (PNAS USA) 115(40) (October 2, 2018):9875–9881. Retrieved January 22, 2024.
- ↑ Amy L Krain and F. Xavier Castellanos, Brain development and ADHD Clinical Psychology Review 26(4) (August 2005):433–444. Retrieved January 22, 2024.
- ↑ Martine Hoogman et al., Subcortical brain volume differences in participants with attention deficit hyperactivity disorder in children and adults: a cross-sectional mega-analysis Lancet Psychiatry 4(4) (April 2017):310-319. Retrieved January 22, 2024.
- ↑ P.K. Douglas et al., Hemispheric brain asymmetry differences in youths with attention-deficit/hyperactivity disorder Neuroimage Clin. 18 (February 2018):744–752. Retrieved January 22, 2024.
- ↑ Stefano Damiani et al., Beneath the surface: hyper-connectivity between caudate and salience regions in ADHD fMRI at rest European Child & Adolescent Psychiatry 30(4) (April 2021):619–631. Retrieved January 22, 2024.
- ↑ Thomas E. Brown, ADD/ADHD and Impaired Executive Function in Clinical Practice Current Psychiatry Reports 10(5) (October 2008):407–411. Retrieved January 22, 2024.
- ↑ Vania Modesto-Lowe, Margaret Chaplin, Victoria Soovajian, and Andrea Meyer, Are motivation deficits underestimated in patients with ADHD? A review of the literature Postgraduate Medicine 125(4) (July 2013):47–52. Retrieved January 22, 2024.
- ↑ Attention Deficit Hyperactivity Disorder National Institute of Mental Health. Retrieved January 2, 2024.
- ↑ 32.0 32.1 Attention deficit hyperactivity disorder: diagnosis and management National Institute for Health and Care Excellence (NICE), September 13, 2019. Retrieved January 22, 2024.
- ↑ Canadian ADHD Practice Guidelines Canadian Attention Deficit Hyperactivity Disorder Resource Alliance (CADDRA), 2010. Retrieved January 22, 2024.
- ↑ ADHD Treatment Recommendations Centers for Disease Control and Prevention (CDC). Retrieved January 22, 2024.
- ↑ Madeleine P. Strohl, Bradley's Benzedrine studies on children with behavioral disorders Yale J Biol Med. 84(1) (March 2011):27-33. Retrieved January 22, 2024.
- ↑ Ole Jakob Storebø et al., Methylphenidate for children and adolescents with attention deficit hyperactivity disorder (ADHD) Cochrane Database Syst Rev. 3(3) (March 27, 2023:CD009885. Retrieved January 22, 2024.
- ↑ Stephen V. Faraone, Joseph Biederman, and Christine Roe, Efficacy, Acceptability, and Tolerability of Lisdexamfetamine, Mixed Amphetamine Salts, Methylphenidate, and Modafinil in the Treatment of Attention-Deficit Hyperactivity Disorder in Adults: A Systematic Review and Meta-analysis Annals of Pharmacotherapy 53(2) (2002):121–133. Retrieved January 22, 2024.
- ↑ Sharon B. Wigal, Efficacy and safety limitations of attention-deficit hyperactivity disorder pharmacotherapy in children and adults CNS Drugs (23)(Suppl 1) (2009):21–31. Retrieved January 22, 2024.
- ↑ Anne E Den Heijer et al, Sweat it out? The effects of physical exercise on cognition and behavior in children and adults with ADHD: a systematic literature review Journal of Neural Transmission 124(Suppl 1) (2017):3–26. Retrieved January 22, 2024.
- ↑ Attention-Deficit/Hyperactivity Disorder (ADHD) Cleveland Clinic. Retrieved January 22, 2024.
- ↑ Stephen V. Faraone, The scientific foundation for understanding attention-deficit/hyperactivity disorder as a valid psychiatric disorder European Child & Adolescent Psychiatry 14(1) (February 2005):1–10. Retrieved January 22, 2024.
- ↑ 42.0 42.1 Sarah Boseley, Hyperactive children may suffer from genetic disorder, says study The Guardian (September 29, 2010). Retrieved January 22, 2024.
- ↑ Ralph Lewis, Is ADHD a Real Disorder or One End of a Normal Continuum? Psychology Today (January 6, 2021). Retrieved January 22, 2024.
- ↑ Eileen Cormier, Attention deficit/hyperactivity disorder: a review and update Journal of Pediatric Nursing 23(5) (October 2008):345-357. Retrieved January 22, 2024.
- ↑ Ylva Ginsberg, Javier Quintero,Ernie Anand, Marta Casillas, and Himanshu P. Upadhyaya, Underdiagnosis of Attention-Deficit/Hyperactivity Disorder in Adult Patients: A Review of the Literature The Primary Care Companion for CNS Disorders 16(3) (2014). Retrieved January 22, 2024.
- ↑ Alaa M. Hamed, Aaron J. Kauer, and Hanna E. Stevens, Why the Diagnosis of Attention Deficit Hyperactivity Disorder Matters Frontiers in Psychiatry 6 (November 26, 2015). Retrieved January 22, 2024.
- ↑ Larry B. Silver, Attention-Deficit/Hyperactivity Disorder: A Clinical Guide to Diagnosis and Treatment for Health and Mental Health Professionals (American Psychiatric Association Publishing, 2003, ISBN 978-1585621316).
References
ISBN links support NWE through referral fees
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition: DSM-5. American Psychiatric Publishing, 2013. ISBN 978-0890425541
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition Text Revision: DSM-5-TR. American Psychiatric Publishing, 2022. ISBN 0890425760
- Clauss-Ehlers, Caroline S. Encyclopedia of Cross-Cultural School Psychology. Springer, 2010. ISBN 978-0387717982
- Crichton, Sir Alexander. An Inquiry Into The Nature And Origin Of Mental Derangement. Legare Street Press, 2022 (original 1798). ISBN 978-1017488913
- Dulcan, Mina K., Rachel R. Ballard, Poonam Jha, and Julie M. Sadhu. Concise Guide to Child and Adolescent Psychiatry. American Psychiatric Publishing, 2017. ISBN 978-1615370788
- Millichap, J. Gordon. Attention Deficit Hyperactivity Disorder Handbook. Springer, 2009. ISBN 978-1441913968
- Nolen-Hoeksema, Susan. Abnormal Psychology. McGraw Hill, 2022. ISBN 978-1265237769
- Ramsay, J. Russell, and Anthony L. Rostain. Cognitive-Behavioral Therapy for Adult ADHD: An Integrative Psychosocial and Medical Approach. Routledge, 2007. ISBN 978-0415955010
- Silver, Larry B. Attention-Deficit/Hyperactivity Disorder: A Clinical Guide to Diagnosis and Treatment for Health and Mental Health Professionals. American Psychiatric Association Publishing, 2003. ISBN 978-1585621316
- Weiss, Margaret, Lily Trokenberg Hechtman, and Gabrielle Weiss. ADHD in Adulthood: A Guide to Current Theory, Diagnosis, and Treatment. Johns Hopkins University Press, 2001. ISBN 978-0801868221
- Wiener, Jerry M., and Mina K. Dulcan (eds.). Textbook Of Child and Adolescent Psychiatry. American Psychiatric Publishing, 2003. ISBN 978-1585620579
- Youngstrom, Eric A., Mitchell J. Prinstein, Eric J. Mash, and Russell A. Barkley (eds.). Assessment of Disorders in Childhood and Adolescence. The Guilford Press, 2020. ISBN 978-1462543632
External links
All links retrieved January 22, 2024.
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article
in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.