Calcitonin
Calcitonin/calcitonin-related polypeptide, alpha
| ||||||||||||||
| Identifiers | ||||||||||||||
| Symbol(s) | CALCA; CALC1; CGRP; CGRP-I; CGRP1; CT; KC; MGC126648 | |||||||||||||
| External IDs | OMIM: 114130 MGI: 2151253 HomoloGene: 1319 | |||||||||||||
| ||||||||||||||
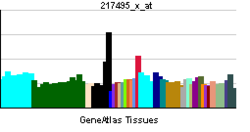
| RNA expression pattern | ||||||||||||||
| Orthologs | ||||||||||||||
| Human | Mouse | |||||||||||||
| Entrez | 796 | 12310 | ||||||||||||
| Ensembl | ENSG00000110680 | ENSMUSG00000030669 | ||||||||||||
| Uniprot | P01258 | Q99JA0 | ||||||||||||
| Refseq | NM_001033952 (mRNA) NP_001029124 (protein) |
NM_001033954 (mRNA) NP_001029126 (protein) | ||||||||||||
| Location | Chr 11: 14.94 - 14.95 Mb | Chr 7: 114.42 - 114.43 Mb | ||||||||||||
| Pubmed search | [1] | [2] | ||||||||||||
Calcitonin is a 32-amino acid polypeptide hormone that is produced in humans primarily by the parafollicular (also known as C-cells) of the thyroid, and in many other animals in the ultimobranchial body.[1] It acts to reduce blood calcium (Ca2+), opposing the effects of parathyroid hormone (PTH) [2]
note:Parathyroid hormone (PTH), or parathormone, is secreted by the parathyroid glands as a polypeptide containing 84 amino acids. It acts to increase the concentration of calcium (Ca2+) in the blood, whereas calcitonin (a hormone produced by the parafollicular cells (C cells) of the thyroid gland) acts to decrease calcium concentration. PTH acts to increase the concentration of calcium in the blood by acting upon parathyroid hormone receptor in three parts of the body:[3]
The ultimobranchial body or gland is a small organ found in the neck region of many animals.
In humans, the ultimobranchial body is an embryological structure that gives rise to the calcitonin-producing cells—also called parafollicular cells or clear cells—of the thyroid gland. In humans, this body is a derivative of the ventral recess of the fourth pharyngeal pouch (or fifth)[4]
It has been found in fish, reptiles, birds, and mammals. Its importance in humans has not been as well established as its importance in other animals.[5]
Biosynthesis
Calcitonin is formed by the proteolytic cleavage of a larger prepropeptide, which is the product of the CALC1 gene (CALCA ). The CALC1 gene belongs to a superfamily of related protein hormone precursors including islet amyloid precursor protein, calcitonin gene-related peptide, and the precursor of adrenomedullin.
Physiology
The hormone participates in calcium (Ca2+) and phosphorus metabolism. In many ways, calcitonin has the counter effects of parathyroid hormone (PTH).
To be specific, calcitonin reduces blood Ca2+ levels in three ways:
- Decreasing Ca2+ absorption by the intestines[6]
- Decreasing osteoclast activity in bones[7]
- Decreasing Ca2+ and phosphate reabsorption by the kidney tubules[8]
Actions
Its actions, in a broad sense, are:
- Bone mineral metabolism:
- - Prevent postprandial hypercalcemia resulting from absorption of Ca2+ from foods during a meal
- - Promote mineralization of skeletal bone
- - Protect against Ca2+ loss from skeleton during periods of Ca2+ stress such as pregnancy and lactation
- Vitamin D regulation
- A satiety hormone:
- - Inhibit food intake in rats and monkeys
- - May have CNS action involving the regulation of feeding and appetite
Receptor
The calcitonin receptor, found primarily on osteoclasts, is a G protein-coupled receptor, which is coupled by Gs to adenylyl cyclase and thereby to the generation of cAMP in target cells.
History
Calcitonin was purified in 1962 by Copp and Cheney.[9] While it was initially considered a secretion of the parathyroid glands, it was later identified as the secretion of the C-cells of the thyroid gland.
Pharmacology
Salmon calcitonin is used for the treatment of:
- Postmenopausal osteoporosis
- Hypercalcaemia
- Paget's disease
- Bone metastases
- Phantom limb pain[10]
The following information is from the UK Electronic Medicines Compendium[11]
General characteristics of the active substance
Salmon calcitonin is rapidly absorbed and eliminated. Peak plasma concentrations are attained within the first hour of administration.
Animal studies have shown that calcitonin is primarily metabolised via proteolysis in the kidney following parenteral administration. The metabolites lack the specific biological activity of calcitonin. Bioavailability following subcutaneous and intramuscular injection in humans is high and similar for the two routes of administration (71% and 66%, respectively).
Calcitonin has short absorption and elimination half-lives of 10-15 minutes and 50-80 minutes, respectively. Salmon calcitonin is primarily and almost exclusively degraded in the kidneys, forming pharmacologically-inactive fragments of the molecule. Therefore, the metabolic clearance is much lower in patients with end-stage renal failure than in healthy subjects. However, the clinical relevance of this finding is not known. Plasma protein binding is 30% to 40%.
Characteristics in patients
There is a relationship between the subcutaneous dose of calcitonin and peak plasma concentrations. Following parenteral administration of 100 IU calcitonin, peak plasma concentration lies between about 200 and 400 pg/ml. Higher blood levels may be associated with increased incidence of nausea and vomiting.
Preclinical safety data
Conventional long-term toxicity, reproduction, mutagenicity, and carcinogenicity studies have been performed in laboratory animals. Salmon calcitonin is devoid of embryotoxic, teratogenic, and mutagenic potential.
An increased incidence of pituitary adenomas has been reported in rats given synthetic salmon calcitonin for 1 year. This is considered a species-specific effect and of no clinical relevance. Salmon calcitonin does not cross the placental barrier.
In lactating animals given calcitonin, suppression of milk production has been observed. Calcitonin is secreted into the milk.
Pharmaceutical manufacture
Calcitonin was extracted from the Ultimobranchial glands (thyroid-like glands) of fish, particularly salmon. Salmon calcitonin resembles human calcitonin, but is more active. At present, it is produced either by recombinant DNA technology or by chemical peptide synthesis. The pharmacological properties of the synthetic and recombinant peptides have been demonstrated to be qualitatively and quantitatively equivalent.[11]
Use of calcitonin in osteoarthritis
Oral calcitonin may have a chondroprotective role in osteoarthritis (OA), according to data in rats presented in December, 2005, at the 10th World Congress of the Osteoarthritis Research Society International (OARSI) in Boston, Massachusetts. Although calcitonin is an established antiresorptive agent, its disease-modifying effects on chondrocytes and cartilage metabolisms have not been well established until now.
This new study, however, may help to explain how calcitonin affects osteoarthritis. “Calcitonin acts both directly on osteoclasts, resulting in inhibition of bone resorption and following attenuation of subchondral bone turnover, and directly on chondrocytes, attenuating cartilage degradation and stimulating cartilage formation,” says researcher Morten Karsdal, MSC, PhD, of the department of pharmacology at Nordic Bioscience in Herlev, Denmark. “Therefore, calcitonin may be a future efficacious drug for OA.”[12]
See also
- Procalcitonin
- Miacalcin
ReferencesISBN links support NWE through referral fees
- ↑ Sect. 5, Ch. 6: Anatomy, Structure, and Synthesis of Calcitonin (CT)
- ↑ Medical Physiology, Boron & Boulpaep, ISBN 1-4160-2328-3, Elsevier Saunders 2005. Updated edition. Endocrine system chapter.
- ↑ Physiology at MCG 5/5ch6/s5ch6_11
- ↑ Endocrine Glands
- ↑ Sect. 5, Ch. 6: Biological Actions of CT
- ↑ Sect. 5, Ch. 6: Effects of CT on the Small Intestine
- ↑ Sect. 5, Ch. 6: Effects of CT on Bone
- ↑ Sect. 5, Ch. 6: Effects of CT on Kidneys
- ↑ Copp DH, Cheney B. Calcitonin-a hormone from the parathyroid, which lowers the calcium-level of the blood. Nature 1962;193:381-2. PMID 13881213
- ↑ "Calcitonin in phantom limb pain": Ann Pharmacother. 1999 Apr;33(4):499-501 PMID: 10332543
- ↑ 11.0 11.1 http://emc.medicines.org.uk/ UK Electronic Medicines Compendium
- ↑ Kleinman, Denise Mann (2006-01-04). Oral Calcitonin May Delay Onset of Joint Disease and Relieve Pain of OA. Musculoskelital Report. Retrieved 2008-05-20.
- Wood, D., and T. G. Odle. 2006. In J. L. Longe, The Gale Encyclopedia of Cancer. Detroit, MI: Gale. ISBN 1414403623.
J. Biochem, 1976, Vol. 79, No. 2 353-359
© 1976 Japanese Biochemical Society research-article Amino Acid Sequence of Eel Calcitonin Toshiharu NODA1 and Kozo NARITA
http://smart.embl-heidelberg.de/smart/do_annotation.pl?DOMAIN=SM00113
Simple Modular Architecture Research Tool
Further reading
- MacIntyre I, Alevizaki M, Bevis PJ, Zaidi M (1987). Calcitonin and the peptides from the calcitonin gene.. Clin. Orthop. Relat. Res. (217): 45-55.
- Di Angelantonio S, Giniatullin R, Costa V, et al. (2004). Modulation of neuronal nicotinic receptor function by the neuropeptides CGRP and substance P on autonomic nerve cells.. Br. J. Pharmacol. 139 (6): 1061-73.
- Findlay DM, Sexton PM (2005). Calcitonin.. Growth Factors 22 (4): 217-24.
- Sponholz C, Sakr Y, Reinhart K, Brunkhorst F (2007). Diagnostic value and prognostic implications of serum procalcitonin after cardiac surgery: a systematic review of the literature.. Critical care (London, England) 10 (5): R145.
- Schneider HG, Lam QT (2007). Procalcitonin for the clinical laboratory: a review.. Pathology 39 (4): 383-90.
| Hormones and endocrine glands - edit |
|---|
|
Hypothalamus: GnRH - TRH - CRH - GHRH - somatostatin - dopamine | Posterior pituitary: vasopressin - oxytocin | Anterior pituitary: GH - ACTH - TSH - LH - FSH - prolactin - MSH - endorphins - lipotropin Thyroid: T3 and T4 - calcitonin | Parathyroid: PTH | Adrenal medulla: epinephrine - norepinephrine | Adrenal cortex: aldosterone - cortisol - DHEA | Pancreas: glucagon- insulin - somatostatin | Ovary: estradiol - progesterone - inhibin - activin | Testis: testosterone - AMH - inhibin | Pineal gland: melatonin | Kidney: renin - EPO - calcitriol - prostaglandin | Heart atrium: ANP Stomach: gastrin | Duodenum: CCK - GIP - secretin - motilin - VIP | Ileum: enteroglucagon | Liver: IGF-1 Placenta: hCG - HPL - estrogen - progesterone Adipose tissue: leptin, adiponectin Target-derived NGF, BDNF, NT-3 |
| ||||||||||||||
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.