Difference between revisions of "Peptic ulcer" - New World Encyclopedia
Rick Swarts (talk | contribs) (→Types) |
Rick Swarts (talk | contribs) |
||
| Line 28: | Line 28: | ||
Longe (2006) also recognizes peptic ulcers as occuring in the jejunum, the portion of the [[small intestine]] after the duodenum. | Longe (2006) also recognizes peptic ulcers as occuring in the jejunum, the portion of the [[small intestine]] after the duodenum. | ||
| − | + | Contrary to general belief, more peptic ulcers arise in the duodenum (first part of the small intestine, just after the stomach) than in the stomach. | |
ABout 2% of the population in the United States are estimated to have active peptic ulcers, and 10% will develop such ulcers during their lifetime (Longe 2006). The male female ratio is 3:1 (Longe 2006). Duodenal ulcers occur in all age groups but are most common between the age of 20 and 45; gastric ulcers are most common between the age of 55 and 70 (Longe 2006). While the incidences of duodenal ulcers in the United States has been declining, incidences of gastric ulcers in rising (Longe 2006). | ABout 2% of the population in the United States are estimated to have active peptic ulcers, and 10% will develop such ulcers during their lifetime (Longe 2006). The male female ratio is 3:1 (Longe 2006). Duodenal ulcers occur in all age groups but are most common between the age of 20 and 45; gastric ulcers are most common between the age of 55 and 70 (Longe 2006). While the incidences of duodenal ulcers in the United States has been declining, incidences of gastric ulcers in rising (Longe 2006). | ||
| Line 34: | Line 34: | ||
==Causes== | ==Causes== | ||
| − | The linings in the gastrointestinal tract normally can resist the digestive acids produced. | + | The linings in the gastrointestinal tract normally can resist the digestive acids produced. Ulcers develop when this protective ability is reduced and the lining breaks down. |
| + | The most common causes of peptic ulcers are bacterial infection, NSAIDS (nonsteroidal anti-inflammatory drugs), and disorders that cause oversecretion of digestive juices. | ||
| + | * '''''Helicobacter pylori'' infection'''. A major causative factor is chronic [[inflammation]] due to ''Helicobacter pylori'', a rod-shaped, gram-negative [[bacterium|bacteria]] that colonizes the mucous tissues (the [[Pyloric antrum|antral]] [[mucosa]]) in the digestive tract. The [[immune system]] is unable to clear the infection, despite the appearance of [[antibody|antibodies]]. Thus, the bacterium can cause a chronic active [[gastritis]] (type B gastritis), resulting in a defect in the regulation of [[gastrin]] production by that part of the stomach, and gastrin secretion is increased. [[Gastrin]], in turn, stimulates the production of [[gastric acid]] by parietal cells. The acid erodes the [[mucosa]] and causes the ulcer. This bacterium is the most common cause of duodenal ulcers, being considered the causal factor in about 90% of the cases. | ||
| + | |||
| + | *'''NSAIDS'''. Another major cause of peptic ulcers is the use of [[NSAID]]s, a group of painkillers that includes [[aspirin]], [[ibuprofen]] (Advil, Motrin), ketoprofen ( Orudis), flubiprofen (Ansaid, Ocufen), and indomethacin (Indacin) (Longe 2006). The gastric mucosa protects itself from gastric acid with a layer of mucous, the secretion of which is stimulated by certain prostaglandins. NSAIDs block the function of [[cyclooxygenase]] 1 (''cox-1''), which is essential for the production of these prostaglandins. Longe (2006) reports that the single most common cause of gastric ulcers is the use of NSAIDS, and that [[aspirin]] is the one most likely to cause ulcers. (Other reports place ''Helicobacter pylori'' as the primary cause in gastric ulcers.) Newer NSAIDs ([[celecoxib]], [[rofecoxib]]) only inhibit ''cox-2'', which is less essential in the gastric mucosa, and roughly halve the risk of NSAID-related gastric ulceration. | ||
| + | |||
| + | *'''Other causes'''. After ''Helicobacter pylori'' and NSAIDS, there are other causes that account for the remaining about five percent of ulcers. One is Zollinger-Ellison syndrome in which small tumors secrete the hormone gastrin the stimulates the producitng of digestive acids (Longe 2006). | ||
| + | |||
| + | ===Stress and other factors=== | ||
| + | |||
| + | Ulcers can also be caused or worsened by drugs such as [[Aspirin]] and other [[NSAID]]s. About 4% of stomach ulcers are caused by a [[malignant]] tumor, so multiple biopsies are needed to make sure. Duodenal ulcers are generally [[benign]]. | ||
| − | |||
| − | |||
===Stress and ulcers=== | ===Stress and ulcers=== | ||
| + | |||
| + | [[Tobacco smoking]], [[Blood type|blood group]], [[spice]]s and other factors that were suspected to cause ulcers until late in the 20th century, are actually of relatively minor importance in the development of peptic ulcers.<ref>For nearly 100 years, scientists and doctors thought that ulcers were caused by stress, spicy food, and alcohol. Treatment involved bed rest and a bland diet. Later, researchers added stomach acid to the list of causes and began treating ulcers with antacids. [http://digestive.niddk.nih.gov/ddiseases/pubs/hpylori/ National Digestive Diseases Information Clearinghouse]</ref> | ||
| + | |||
| + | |||
| + | |||
| + | |||
| + | |||
Despite the finding that a [[bacterial infection]] is the cause of ulcers in more than 75% of cases, [[bacterial infection]] does not appear to explain all ulcers and researchers continue to look at stress as a possible cause, or at least a complication in the development of ulcers. | Despite the finding that a [[bacterial infection]] is the cause of ulcers in more than 75% of cases, [[bacterial infection]] does not appear to explain all ulcers and researchers continue to look at stress as a possible cause, or at least a complication in the development of ulcers. | ||
| Line 53: | Line 68: | ||
A study on mice showed that both long-term water-immersion-restraint stress and ''H. pylori'' infection were independently associated with the development of peptic ulcers (PMID 12465722). | A study on mice showed that both long-term water-immersion-restraint stress and ''H. pylori'' infection were independently associated with the development of peptic ulcers (PMID 12465722). | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
There is debate as to whether ''Stress'' in the psychological sense can influence the development of peptic ulcers (see [[Peptic Ulcer#Stress and ulcers|Stress and ulcers]]). [[Burn (injury)|Burns]] and [[head trauma]], however, can lead to "stress ulcers", and it is reported in many patients who are on [[mechanical ventilation]]. | There is debate as to whether ''Stress'' in the psychological sense can influence the development of peptic ulcers (see [[Peptic Ulcer#Stress and ulcers|Stress and ulcers]]). [[Burn (injury)|Burns]] and [[head trauma]], however, can lead to "stress ulcers", and it is reported in many patients who are on [[mechanical ventilation]]. | ||
| Line 72: | Line 79: | ||
[[Gastrinoma]]s ([[Zollinger Ellison syndrome]]), rare gastrin-secreting tumors, cause multiple and difficult to heal ulcers. | [[Gastrinoma]]s ([[Zollinger Ellison syndrome]]), rare gastrin-secreting tumors, cause multiple and difficult to heal ulcers. | ||
| + | |||
| + | [[Glucocorticoid]]s lead to atrophy of all [[epithelium|epithelial]] tissues. Their role in ulcerogenesis is relatively small. | ||
Revision as of 02:54, 5 July 2007
| ICD-10 | K25-26 |
|---|---|
| ICD-O: | {{{ICDO}}} |
| ICD-9 | 531-534 |
| OMIM | {{{OMIM}}} |
| MedlinePlus | {{{MedlinePlus}}} |
| eMedicine | {{{eMedicineSubj}}}/{{{eMedicineTopic}}} |
| DiseasesDB | {{{DiseasesDB}}} |
A peptic ulcer is an ulcer of the area of the gastrointestinal tract that is usually acidic and includes the lower part of the esophagus, the stomach, and the duodenum (first part of the small intestine). Some also include the jejunum (second part of the small intestine) (Longe 2006). This condition also is known as peptic ulcer disease or PUD. "Peptic" refers to the enzyme pepsin, a digestive protease in the stomach that digests food proteins into peptides.
An ulcer is a lesion or eroded area on the surface of the skin or mucous membranes characterized by tissue disintegration. Essentially, it impacts the epithelium—the tissue that covers organs and surfaces of the bodies of animals, including both outside surfaces (the skin) and inside cavities. As such, an ulcer can impact such areas as the the oral cavity, the lower extremities, feet, the eyes (most often the cornea), and so forth. However, in common usage, ulcer often is used to refer to peptic ulcers, which are disorders in the upper digestive tract.
The most common peptic ulcers are gastric ulcers, which occur in the stomach, and duodenal ulcers, which occur in the first part of the small intestine (duodenum). About 80% of all ulcers in the digestive tract are duodenal ulcers, and 16% are peptic ulcers (Longe 2005).
Ulcers in general have a varity of causes, including injury, circulatory problems, infectious agents, disease, trauma, and so forth. While stress and diet were commonly attributed as causes of peptic ulcers, peptic ulcers are now linked primarily to infection by the bacterium Helicobacter pylori, as well as use to use of nonsteroidal anti-inflammatory drugs (NSAIDS, such as aspirin, ibuprofen, etc.), and in some cases overproduction of digestive juices (Zollinger-Ellison syndrome), among others.
Longe (2006) lists the use of NSAIDS as the single most common cause of gastric ulcers. These drugs, which can be obtained without prescription, often are overused, as people look to treat symptoms of headaches, sore muscles, and other complaints without addressing the underlying causes of the complaints. Such causes reflect the importance of personal responsibility for one's health and perhaps the need for dietary or lifestyle changes.
Types
Peptic ulcers are the most common ulcers of the gastrointestinal tract. A peptic ulcer may arise at various locations:
- Stomach (called gastric ulcer)
- Duodenum (called duodenal ulcer)
- Esophagus (called esophageal ulcer)
- A Meckel's diverticulum
Longe (2006) also recognizes peptic ulcers as occuring in the jejunum, the portion of the small intestine after the duodenum.
Contrary to general belief, more peptic ulcers arise in the duodenum (first part of the small intestine, just after the stomach) than in the stomach.
ABout 2% of the population in the United States are estimated to have active peptic ulcers, and 10% will develop such ulcers during their lifetime (Longe 2006). The male female ratio is 3:1 (Longe 2006). Duodenal ulcers occur in all age groups but are most common between the age of 20 and 45; gastric ulcers are most common between the age of 55 and 70 (Longe 2006). While the incidences of duodenal ulcers in the United States has been declining, incidences of gastric ulcers in rising (Longe 2006).
Causes
The linings in the gastrointestinal tract normally can resist the digestive acids produced. Ulcers develop when this protective ability is reduced and the lining breaks down.
The most common causes of peptic ulcers are bacterial infection, NSAIDS (nonsteroidal anti-inflammatory drugs), and disorders that cause oversecretion of digestive juices.
- Helicobacter pylori infection. A major causative factor is chronic inflammation due to Helicobacter pylori, a rod-shaped, gram-negative bacteria that colonizes the mucous tissues (the antral mucosa) in the digestive tract. The immune system is unable to clear the infection, despite the appearance of antibodies. Thus, the bacterium can cause a chronic active gastritis (type B gastritis), resulting in a defect in the regulation of gastrin production by that part of the stomach, and gastrin secretion is increased. Gastrin, in turn, stimulates the production of gastric acid by parietal cells. The acid erodes the mucosa and causes the ulcer. This bacterium is the most common cause of duodenal ulcers, being considered the causal factor in about 90% of the cases.
- NSAIDS. Another major cause of peptic ulcers is the use of NSAIDs, a group of painkillers that includes aspirin, ibuprofen (Advil, Motrin), ketoprofen ( Orudis), flubiprofen (Ansaid, Ocufen), and indomethacin (Indacin) (Longe 2006). The gastric mucosa protects itself from gastric acid with a layer of mucous, the secretion of which is stimulated by certain prostaglandins. NSAIDs block the function of cyclooxygenase 1 (cox-1), which is essential for the production of these prostaglandins. Longe (2006) reports that the single most common cause of gastric ulcers is the use of NSAIDS, and that aspirin is the one most likely to cause ulcers. (Other reports place Helicobacter pylori as the primary cause in gastric ulcers.) Newer NSAIDs (celecoxib, rofecoxib) only inhibit cox-2, which is less essential in the gastric mucosa, and roughly halve the risk of NSAID-related gastric ulceration.
- Other causes. After Helicobacter pylori and NSAIDS, there are other causes that account for the remaining about five percent of ulcers. One is Zollinger-Ellison syndrome in which small tumors secrete the hormone gastrin the stimulates the producitng of digestive acids (Longe 2006).
Stress and other factors
Ulcers can also be caused or worsened by drugs such as Aspirin and other NSAIDs. About 4% of stomach ulcers are caused by a malignant tumor, so multiple biopsies are needed to make sure. Duodenal ulcers are generally benign.
Stress and ulcers
Tobacco smoking, blood group, spices and other factors that were suspected to cause ulcers until late in the 20th century, are actually of relatively minor importance in the development of peptic ulcers.[1]
Despite the finding that a bacterial infection is the cause of ulcers in more than 75% of cases, bacterial infection does not appear to explain all ulcers and researchers continue to look at stress as a possible cause, or at least a complication in the development of ulcers.
An expert panel convened by the Academy of Behavioral Medicine research concluded that ulcers are not purely an infectious disease and that psychological factors do play a significant role.[2] Researchers are examining how stress might promote H. pylori infection. For example, Helicobacter pylori thrives in an acidic environment, and stress has been demonstrated to cause the production of excess stomach acid.
The discovery that Helicobacter pylori is a cause of peptic ulcer has tempted many to conclude that psychological factors are unimportant. But this is dichotomised thinking. There is solid evidence that psychological stress triggers many ulcers and impairs response to treatment, while helicobacter is inadequate as a monocausal explanation as most infected people do not develop ulcers. Psychological stress probably functions most often as a cofactor with H pylori. It may act by stimulating the production of gastric acid or by promoting behavior that causes a risk to health. Unravelling the aetiology of peptic ulcer will make an important contribution to the biopsychosocial model of disease.[3]
A study of peptic ulcer patients in a Thai hospital showed that chronic stress was strongly associated with an increased risk of peptic ulcer, and a combination of chronic stress and irregular mealtimes was a significant risk factor (PMID 12948263).
A study on mice showed that both long-term water-immersion-restraint stress and H. pylori infection were independently associated with the development of peptic ulcers (PMID 12465722).
There is debate as to whether Stress in the psychological sense can influence the development of peptic ulcers (see Stress and ulcers). Burns and head trauma, however, can lead to "stress ulcers", and it is reported in many patients who are on mechanical ventilation.
Smoking leads to atherosclerosis and vascular spasms, causing vascular insufficiency and promoting the development of ulcers through ischemia.
Overuse of Laxatives are also known to cause peptic ulcers.
A family history is often present in duodenal ulcers, especially when blood group O is also present. Inheritance appears to be unimportant in gastric ulcers.
Gastrinomas (Zollinger Ellison syndrome), rare gastrin-secreting tumors, cause multiple and difficult to heal ulcers.
Glucocorticoids lead to atrophy of all epithelial tissues. Their role in ulcerogenesis is relatively small.
Symptoms and signs
Symptoms of a peptic ulcer can be:
- Abdominal pain, classically epigastric with severity relating to mealtimes, after around 3 hours of taking a meal (duodenal ulcers are classically relieved by food, while gastric ulcers are exacerbated by it);
- Bloating and abdominal fullness
- Waterbrash (rush of saliva after an episode of regurgitation to dilute the acid in esophagus)
- Nausea, and lots of vomiting
- Loss of appetite and weight loss;
- Hematemesis (vomiting of blood);
- Melena (tarry, foul-smelling faeces due to oxidised iron from hemoglobin)
- Rarely, an ulcer can lead to a gastric or duodenal perforation. This is extremely painful and requires immediate surgery.
A history of heartburn, gastroesophageal reflux disease (GERD) and use of certain forms of medication can raise the suspicion for peptic ulcer. Medicines associated with peptic ulcer include NSAID (non-steroid anti-inflammatory drugs) that inhibit cyclooxygenase, and most glucocorticoids (e.g. dexamethasone and prednisolone).
In patients over 45 with more than 2 weeks of the above symptoms, the odds for peptic ulceration are high enough to warrant rapid investigation by EGD (see below).
The timing of the symptoms in relation to the meal may differentiate between gastric and duodenal ulcers: A gastric ulcer would give epigastric pain during the meal, as gastric acid is secreted, or after the meal, as the alkaline duodenal contents reflux into the stomach. Symptoms of duodenal ulcers would manifest mostly before the meal — when acid (production stimulated by hunger) is passed into the duodenum. However, this is not a reliable sign in clinical practice.
Complications
- Perforated ulcer (anterior. Surface) with sudden onset of the pain, a chemical peritonitis followed by bacterial peritonitis
- Posterior penetration (posterior. Surface), maybe to pancreas=>increased amylase-pain=>radiating to back, unrelated to meals.
- Hemorrhage (post. Surface), bleeding from Gasteroduodenal artery.
- Gastric Outlet Obstruction (Goo) which happens usually because of edema or scarring, most often occurs in the setting of duodenal or pyloric channel ulcers
Diagnosis
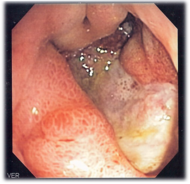
An esophagogastroduodenoscopy (EGD), a form of endoscopy, also known as a gastroscopy, is carried out on patients in whom a peptic ulcer is suspected. By direct visual identification, the location and severity of an ulcer can be described. Moreover, if no ulcer is present, EGD can often provide an alternative diagnosis.
The diagnosis of Helicobacter pylori can be by:
- Breath testing (does not require EGD);
- Direct culture from an EGD biopsy specimen;
- Direct detection of urease activity in a biopsy specimen;
- Measurement of antibody levels in blood (does not require EGD). It is still somewhat controversial whether a positive antibody without EGD is enough to warrant eradication therapy.
The possibility of other causes of ulcers, notably malignancy (gastric cancer) needs to be kept in mind. This is especially true in ulcers of the greater (large) curvature of the stomach; most are also a consequence of chronic H. pylori infection.
If a peptic ulcer perforates, air will leak from the inside of the gastrointestinal tract (which always contains some air) to the peritoneal cavity (which normally never contains air). This leads to "free gas" within the peritoneal cavity. If the patient stands erect, as when having a chest X-ray, the gas will float to a position underneath the diaphragm. Therefore, gas in the peritoneal cavity, shown on an erect chest X-ray or supine lateral abdominal X-ray, is an omen of perforated peptic ulcer disease.
Macroscopical appearance
Gastric ulcer is most often localized on the lesser curvature of the stomach. It is a round to oval parietal defect ("hole"), 2 to 4 cm diameter, with a smooth base and perpendicular borders. These borders are not elevated or irreguliar as in gastric cancer - ulcerative form. Surrounding mucosa may present radial folds, as a consequence of the parietal scarring.
Microscopical appearance
Gastric peptic ulcer is a mucosal defect which penetrates the muscularis mucosae and muscularis propria, produced by acid-pepsin aggression. Ulcer margins are perpendicular and present chronic gastritis. During the active phase, the base of the ulcer shows 4 zones: inflammatory exudate, fibrinoid necrosis, granulation tissue and fibrous tissue. The fibrous base of the ulcer may contain vessels with thickened wall or with thrombosis.[4]
Treatment
Younger patients with ulcer-like symptoms are often treated with antacids or H2 antagonists before EGD is undertaken. Bismuth compounds may actually reduce or even clear organisms.
Patients who are taking nonsteroidal anti-inflammatories (NSAIDs) may also be prescribed a prostaglandin analogue (Misoprostol) in order to help prevent peptic ulcers, which may be a side-effect of the NSAIDs.
When H. pylori infection is present, the most effective treatments are combinations of 2 antibiotics (e.g. Erythromycin, Ampicillin, Amoxicillin, Tetracycline, Metronidazole) and 1 proton pump inhibitor (PPI). An effective combination would be Amoxicillin + Metronidazole + Pantoprazole (a PPI). In the absence of H. pylori, long-term higher dose PPIs are often used.
Treatment of H. pylori usually leads to clearing of infection, relief of symptoms and eventual healing of ulcers. Recurrence of infection can occur and retreatment may be required, if necessary with other antibiotics. Since the widespread use of PPI's in the 1990s, surgical procedures (like "highly selective vagotomy") for uncomplicated peptic ulcers became obsolete.
Perforated peptic ulcer is a surgical emergency and requires surgical repair of the perforation. Most bleeding ulcers require endoscopy urgently to stop bleeding with cautery or injection.
Epidemiology
In Western countries the prevalence of Helicobacter pylori infections roughly matches age (i.e., 20% at age 20, 30% at age 30, 80% at age 80 etc). Prevalence is higher in third world countries. Transmission is by food, contaminated groundwater, and through human saliva (such as from kissing or sharing food utensils.)
A minority of cases of Helicobacter infection will eventually lead to an ulcer and a larger proportion of people will get non-specific discomfort, abdominal pain or gastritis.
History
In 1997, the Centers for Disease Control and Prevention, with other government agencies, academic institutions, and industry, launched a national education campaign to inform health care providers and consumers about the link between H. pylori and ulcers. This campaign reinforced the news that ulcers are a curable infection, and the fact that health can be greatly improved and money saved by disseminating information about H. pylori.[5]
Helicobacter pylori was rediscovered in 1982 by two Australian scientists Robin Warren and Barry Marshall[6]. In their original paper, Warren and Marshall contended that most stomach ulcers and gastritis were caused by colonization with this bacterium, not by stress or spicy food as had been assumed before.[7]
The H. pylori hypothesis was poorly received, so in an act of self-experimentation Marshall drank a petri-dish containing a culture of organisms extracted from a patient and soon developed gastritis. His symptoms disappeared after two weeks, but he took antibiotics to kill the remaining bacteria at the urging of his wife, since halitosis is one of the symptoms of infection.[8] This experiment was published in 1984 in the Australian Medical Journal and is among the most cited articles from the journal.
In 2005, the Karolinska Institute in Stockholm awarded the Nobel Prize in Physiology or Medicine to Dr. Marshall and his long-time collaborator Dr. Warren "for their discovery of the bacterium Helicobacter pylori and its role in gastritis and peptic ulcer disease". Professor Marshall continues research related to H. pylori and runs a molecular biology lab at UWA in Perth, Western Australia.
John Lykoudis was a general practitioner in Greece who treated patients from peptic ulcer disease with antibiotics long before it was commonly recognized that bacteria were a dominant cause for the disease.[9]
ReferencesISBN links support NWE through referral fees
- ↑ For nearly 100 years, scientists and doctors thought that ulcers were caused by stress, spicy food, and alcohol. Treatment involved bed rest and a bland diet. Later, researchers added stomach acid to the list of causes and began treating ulcers with antacids. National Digestive Diseases Information Clearinghouse
- ↑ [1]
- ↑ [2]
- ↑ [3]
- ↑ Ulcer, Diagnosis and Treatment - CDC Bacterial, Mycotic Diseases
- ↑ Marshall BJ (1983). Unidentified curved bacillus on gastric epithelium in active chronic gastritis. Lancet 1 (8336): 1273–1275. PMID 6134060.
- ↑ Marshall BJ, Warren JR (1984). Unidentified curved bacilli in the stomach patients with gastritis and peptic ulceration. Lancet 1 (8390): 1311–1315. PMID 6145023.
- ↑ [4]
- ↑ Basil Rigas, Efstathios D. Papavasassiliou. John Lykoudis. The general parctitioner in Greece who in 1958 discovered the etiology of, and a treatment for, peptic ulcer disease. in Barry Marshall (editor), Helicobacter Pioneers. Firsthand accounts from the scientists who discovered helicobacters, 1892-1982, 2002, ISBN 0-86793-035-7.
- Blakemore, C., and S. Jennett. 2001. The Oxford Companion to the Body. New York: Oxford University Press. ISBN 019852403X.
- Halpern, G. M. 2004. Ulcer Free!: Nature's Safe & Effective Remedy for Ulcers. Garden City Park, N.Y.: Square One Publishers. ISBN 0757002536.
- Longe, J. L. 2006. The Gale Encyclopedia of Medicine. Detroit: Thomson Gale. ISBN 1414403682.
External links
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.