Difference between revisions of "Prostate" - New World Encyclopedia
Rick Swarts (talk | contribs) |
({{Contracted}}) |
||
| Line 1: | Line 1: | ||
| − | {{Claimed}} | + | {{Claimed}}{{Contracted}} |
{{Infobox Anatomy | | {{Infobox Anatomy | | ||
Name = {{PAGENAME}} | | Name = {{PAGENAME}} | | ||
Revision as of 14:02, 5 June 2007
| Prostate | |
|---|---|
| Male Anatomy | |
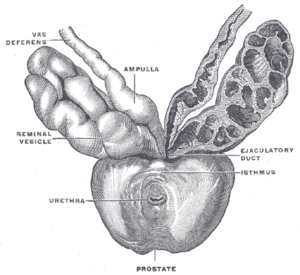
| Prostate with seminal vesicles and seminal ducts, viewed from in front and above. | |
| Latin | prostata |
| Gray's | subject #263 1251 |
| Artery | internal pudendal artery, inferior vesical artery, and middle rectal artery |
| Vein | internal iliac vein |
| Nerve | inferior hypogastric plexus |
| Lymph | external iliac lymph nodes, internal iliac lymph nodes |
| Precursor | Endodermic evaginations of the urethra |
| MeSH | Prostate |
| Dorlands/Elsevier | p_36/12671161 |
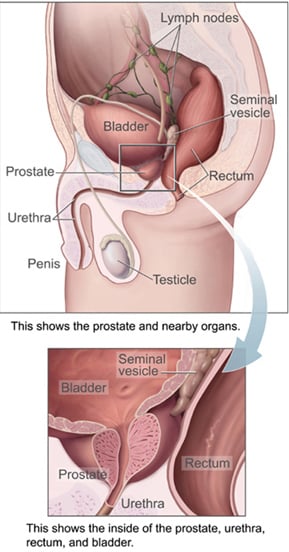
The prostate or prostate gland is a exocrine gland of the male mammalian reproductive system, located at the base of the urinary bladder. It is a compound tubuloalveolar gland (start out as branched tubular, tube-shaped, and branches further to terminate in alveoli). The prostate differs considerably between species anatomically, chemically, and physiologically. It secretes a fluid that is a substantial part of the semen and can regulate urine flow.
In human males, the prostate gland is the size and shape of a chestnut, surrounds the urethra, and consists of 15 to 50 glands that open into the urethra. The alkaline fluid secreted by the prostate is believed to aid in sperm motility. There is no such gland in females.
Structure of human prostate
The prostate is located under and in front of the bladder. A healthy human prostate is slightly larger than a walnut and somewhat triangular, being more rounded at the top, with the more pointed apex directed downward and forward.
The prostate surrounds the urethra just below the urinary bladder. The urethra is a tube which connects the urinary bladder to the outside of the body. The urethra has an excretory function in both genders to pass urine to the outside, and also a reproductive function in the male, as a passage for sperm. In the first part of the uretha, the prostatic urethra, there are several openings, inclduing one where sperm enters and the prostatic ducts where fluid from the prostate enters. The urthra runs through the prostate and opens at the end of the penis. Within the prostate, the urethra coming from the bladder is called the prostatic urethra and merges with the two ejaculatory ducts. (The male urethra has two functions: to carry urine from the bladder during urination and to carry semen during ejaculation.) the prostate has numerous, branched, tubular glands (15 to 50) that open into the urethra. These glands are surrounded by connective tissue (stroma). There are also two ejaculatory ducts from the seminal vesicles (which are located above and behind the prostate) that penetrate the prostate gland and carry sperm and fluid from the seminal vesicles and enter the urethra within the prostate
thin, viscid, milky, alkaline srrounds beginning of urethra two lobes connected anteriorily by by an isthmus and posteriouly by a middle lobe
The glands secrete an alkaline fluid
The prostate and can be felt during a rectal exam.
The ducts are lined with transitional epithelium.
The prostate can be divided in two different ways: by zone, or by lobe.
Zones
The "zone" classification is more often used in pathology.
The prostate gland has four distinct glandular regions, two of which arise from different segments of the prostatic urethra:
| Name | Percent | Description |
| The Peripheral Zone (PZ) | Comprises up to 70% of the normal prostate gland in young men | The sub-capsular portion of the posterior aspect of the prostate gland which surrounds the distal urethra. It is from this portion of the gland that more than 70% of prostatic cancers originate. |
| The Central Zone (CZ) | Constitutes approximately 25% of the normal prostate gland | This zone surrounds the ejaculatory ducts. Central zone tumours account for more than 25% of all prostate cancers. |
| The Transition Zone (TZ) | Responsible for 5% of the prostate volume | This zone is very rarely associated with carcinoma. The transition zone surrounds the proximal urethra and is the region of the prostate gland which grows throughout life and is responsible for the disease of benign prostatic enlargement. |
| The Anterior Fibro-muscular zone (or stroma) | Accounts for approximately 5% of the prostatic weight | This zone is usually devoid of glandular components, and composed only, as its name suggests, of muscle and fibrous tissue. |
Lobes
The "lobe" classification is more often used in gross anatomy.
| anterior lobe (or isthmus) | roughly corresponds to part of Transitional Zone |
| posterior lobe | roughly corresponds to Peripheral Zone |
| lateral lobes | spans all zones |
| median lobe (or middle lobe) | roughly corresponds to part of Central Zone |
Function
The main function of the prostate is to store and secrete a clear, slightly alkaline fluid that constitutes 10-30% of the volume of the seminal fluid that, along with spermatozoa, constitutes semen. The rest of the seminal fluid is produced by the two seminal vesicles. Believed to help sperm motility because sperm more optimally mobile in relatively alkaline medium, and thus conutners the more acidic fluid form testes and sminal vesciles, and nuetralizes acidity of vagina.
The prostate also contains some smooth muscles that help expel semen during ejaculation.
Secretions
Prostatic secretions vary between species. They are generally composed of simple sugars, and are often slightly basic.
In human prostatic secretions, the protein content is less than 1% and includes proteolytic enzymes, acid phosphatase, and prostate-specific antigen. The secretions also contain zinc and citric acid.
Regulation
To work properly, the prostate needs male hormones (androgens), which are responsible for male sex characteristics.
The main male hormone is testosterone, which is produced mainly by the testicles. Some male hormones are produced in small amounts by the adrenal glands.
Development
The prostate gland represents the modified wall of the proximal portion of the male urethra and develops by the 9th week of embryonic life. Condensation ofmesenchyme, urethra and Wolffian ducts gives rise to the adult prostate gland, a composite organ made up of several glandular and non-glandular components tightly fused within a common capsule.
Skene's glands found in many females are homologous to the prostate gland in males.
Prostate disorders
Prostatitis
Prostatitis is inflammation of the prostate gland. There are different forms of prostatitis, each with different causes and outcomes. Acute prostatitis and chronic bacterial prostatitis are treated with antibiotics; chronic non-bacterial prostatitis or male chronic pelvic pain syndrome, which comprises about 95% of prostatitis diagnoses, is treated by a large variety of modalities including alpha blockers, physical therapy, psychotherapy, antihistamines, anxiolytics, nerve modulators and more.[1] Benign prostatic hyperplasia (BPH) occurs in older men; the prostate often enlarges to the point where urination becomes difficult. If the prostate grows too large it may constrict the urethra and impede the flow of urine, making urination difficult and painful and in extreme cases completely impossible. BPH can be treated with medication or with surgery that removes part of the prostate. The surgery most often used in such cases is called transurethral resection of the prostate (TURP or TUR). In TURP, an instrument is inserted through the urethra to remove prostate tissue that is pressing against the upper part of the urethra and restricting the flow of urine. Older men often have corpora amylacea (amyloid), dense accumulations of calcified proteinaceous material, in the ducts of their prostates. The corpora amylacea may obstruct the lumens of the prostatic ducts, and may underlie some cases of BPH.
Prostate Cancer
Prostate cancer is one of the most common cancers affecting elderly men in developed countries and a major cause of death. Regular rectal exams are recommended for older men to detect prostate cancer early. Research has shown that regular ("more than five times per week"[2]) masturbation can cut the risk of prostate cancer by up to 66%. This is because regular ejaculation reduces the buildup of carcinogenic deposits in sperm which can damage the cells lining the prostate. This also applies to frequent sexual intercourse. Once the lining of the prostate is affected with cancer, the only known treatments are surgery and radiation therapy. Both may limit the ability to have erection afterwards.
Male Sexual Response
During orgasm sperm are transmitted from the ductus deferens into the male urethra via the ejaculatory ducts, which lie within the prostate gland. The prostate is often referred to as the male g-spot. Some men are able to achieve orgasm solely through stimulation of the prostate gland. Men who report the sensation of prostate stimulation often give descriptions similar to women's accounts of G-spot stimulation.[3] When combined with penile stimulation, some men report that prostate stimulation increases the volume of their ejaculation.
Additional images
Prostate Cancer
In 1993, the Journal of the American Medical Association revealed a connection between vasectomy and an increased risk of prostate cancer. Reported studies of 48,000 and 29,000 men who had vasectomies showed 66 percent and 56 percent higher rates of prostate cancer, respectively. The risk increase with age and the number of years since the vasectomy was performed. Failure to receive available treatments may result in metastases to bone, and rectal, seminal vesicle, bladder or lymph nodes are also often involved in the spread of prostate cancer[citation needed].
However, in March of the same year, the National Institute of Child Health and Human Development held a conference cosponsored by the National Cancer Institute and others to review the available data and information on the link between prostate cancer and vasectomies. It was determined that an association between the two was very weak at best, and even if having a vasectomy increased one's risk, the risk was relatively small.
In 1997, the NCI and held a conference with the prostate cancer Progressive Review Group (a committee of scientists, medical personel, and others). Their final report, published in 1998 stated that evidence that vasectomies help to develop prostate cancer was weak at best.[4]
ReferencesISBN links support NWE through referral fees
The text of this article was originally taken from NIH Publication No. 02-4806, a public domain resource [1].
- ↑ Pharmacological treatment options for prostatitis/chronic pelvic pain syndrome (html) (2006). Retrieved 2006-12-11.
- ↑ http://news.bbc.co.uk/1/hi/health/3072021.stm
- ↑ Ladas, AK and Whipple, B; Perry, JD [1982]. The G spot and other discoveries about human sexuality. New York: Holt, Rinehart, and Winston.
- ↑ http://www.cancer.gov/cancertopics/factsheet/Risk/vasectomy
External links
- Active Sex Life Seen as Protecting Prostate from NPR.org
- "What I need to know about prostate problems" by the US National Institutes of Health.
- "Drug hope in prostate cancer care", from BBC News
- "Prostatic specialist surgeon"
- UK Prostate Link
- Men's Health NZ Information on prostate health and testosterone
- Template:SUNYAnatomyFigs - "Mid-sagittal section of the male pelvis."
- "Virtual Prostate" animation by George Washington University Medical Center
- Template:ViennaCrossSection
Template:Male reproductive system
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.