Health
Dr. Randle, the original Wikipedia article was just a stub, or portal article linked to other health related topics. I added short content here from the following articles: environmental health, mental health, public health and population health. You will have to decide whether these should actually be there or not, and if so, the order.Rick Swarts 18:24, 13 April 2006 (UTC)
- For the science of human and animal health, see Health science.
Health is a term that refers to a combination of the absence of illness, the ability to cope with everyday activities, physical fitness, and high quality of life. In any organism, health can be said to be a "state of balance," or analogous to homeostasis, and it also implies good prospects for continued survival. Wellness is a term sometimes used to describe the psychological state of being healthy, but is most often used in the field of alternative medicine to describe one's state of being.
The most widely accepted definition is that of the World Health Organization (WHO). It states that "health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity" (WHO, 1946). In more recent years, this statement has been modified to include the ability to lead a "socially and economically productive life." The WHO definition is not without criticism, as some argue that health cannot be defined as a state at all, but must be seen as a process of continuous adjustment to the changing demands of living and of the changing meanings we give to life. The WHO definition is therefore considered by many as an idealistic goal rather than a realistic proposition.
Health is maintained through the science of medicine, but can also be improved by individual effort. Physical fitness, weight loss, healthy eating, stress management training and stopping smoking and other substance abuse are examples of steps to improve one's health. Workplace programs are recognized by an increasingly large number of companies for their value in improving health and well-being of their employees, and increasing morale, loyalty and productivity at work. A company may provide a gym with exercise equipment, start smoking cessation programs, provide nutrition, weight or stress management training. Other programs may include health risk assessments and health screenings.
Alternative medicine can sometimes be used to improve health. However, with the lack of scientific proof through double blind testing, the placebo effect should be assumed to provide the health improvement in the case of successful alternative treatments until such testing can provide proof of any effects besides placebo. This is because as someone who feels well from their (possibly subconcious) belief in the therapies may lower their stress levels, resulting in beneficial effects on numerous factors, including blood pressure, gastrointestinal functioning, and immune response. The field of psychoneuroimmunology explores these links.
An increasing measure of the health of populations is height, which is strongly regulated by nutrition and health care, among other standard of living and quality of life matters. The study of human growth, its regulators and its implications is known as auxology.
Environmental health
Environmental health comprises those aspects of human health, including quality of life, that are determined by physical, chemical, biological, social, and psychosocial factors in the environment. It also refers to the theory and practice of assessing, correcting, controlling, and preventing those factors in the environment that can potentially affect adversely the health of present and future generations [1].
Environmental health as used by the WHO Regional Office for Europe, includes both the direct pathological effects of chemicals, radiation and some biological agents, and the effects (often indirect) on health and wellbeing of the broad physical, psychological, social and aesthetic environment which includes housing, urban development, land use and transport. [2]
Nutrition,soil contamination, water pollution, air pollution,light pollution, waste control and public health are integral aspects of environmental health.
When well-being of a whole population is measured, these become economic and political concerns. Increasingly wellness concerns are affecting fiscal policy and prompting some advocates to call for monetary reform (to end systematic pollution credit, governments actually paying to create human health harms).
Environmental health services are defined by the World Health Organization as:
- those services which implement environmental health policies through monitoring and control activities. They also carry out that role by promoting the improvement of environmental parameters and by encouraging the use of environmentally friendly and healthy technologies and behaviours. They also have a leading role in developing and suggesting new policy areas.
The Environmental Health profession had its modern-day roots in the sanitary and public health movement of the United Kingdom. This was epitomised by Sir Edwin Chadwick who was instrumental in the repeal of the poor laws and was the founding president of the Chartered Institute of Environmental Health.
Mental health
Mental health is a concept that refers to a human individual's emotional and psychological well-being. Merriam-Webster defines mental health as "A state of emotional and psychological well-being in which an individual is able to use his or her cognitive and emotional capabilities, function in society, and meet the ordinary demands of everyday life."
According to the World Health Organization (WHO), there is no one "official" definition of mental health: "Mental health has been defined variously by scholars from different cultures. Concepts of mental health include subjective well-being, perceived self-efficacy, autonomy, competence, intergenerational dependence, and self-actualization of one's intellectual and emotional potential, among others. From a cross-cultural perspective, it is nearly impossible to define mental health comprehensively. It is, however, generally agreed that mental health is broader than a lack of mental disorders." [3] Cultural differences, subjective assessments, and competing professional theories all affect how "mental health" is defined. In general, most experts agree that "mental health" and "mental illness" are not opposites. In other words, the absence of a recognized mental disorder is not necessarily an indicator of mental health.
One way to think about mental health is by looking at how effectively and successfully a person functions. Feeling capable and competent; being able to handle normal levels of stress, maintain satisfying relationships, and lead an independent life; and being able to "bounce back," or recover from difficult situations, are all signs of mental health.
Some experts consider mental health as a continuum. Thus, an individual's mental health may have many different possible values. Mental wellness is generally viewed as a positive attribute, such that a person can reach enhanced levels of mental health, even if they do not have any diagnosable mental illness. This definition of mental health highlights emotional well being, the capacity to live a full and creative life and the flexibility to deal with life's inevitable challenges. Many therapeutic systems and self-help books offer methods and philosophies espousing presumably effective strategies and techniques for further improving the mental wellness of otherwise healthy people.
Public health
Public health is concerned with threats to the overall health of a community based on population health analysis. Many organizations define health and how to promote health differently. The World Health Organization, the United Nations body that sets standards and provides global surveillance of disease, defines health as: "A state of complete physical, mental and social well-being and not merely the absence of disease or infirmity."
The population in question can be as big as a handful of people or, in the case of a pandemic, whole continents. Public health has many sub-fields, but is typically divided into the categories of epidemiology, biostatistics and health services. environmental, social and behavioral health, and occupational Health, are also important fields in public health.
The focus of a public health intervention is to prevent rather than treat a disease through surveillance of cases and the promotion of healthy behaviors. In addition to these activities, in many cases treating a disease can be vital to preventing it in others, such as during an outbreak of an infectious disease. Vaccination programs and distribution of condoms are examples of public health measures.
Many countries have their own government agencies, sometimes known as ministries of health, to respond to domestic health issues. In the United States, the frontline of public health initiatives are state and local health departments. The Surgeon General-led United States Public Health Service, and the Centers for Disease Control and Prevention in Atlanta, although based in the United States, are also involved with several international health issues in addition to their national duties.
There is a vast discrepancy between access to healthcare and public health intiatives between developed nations and developing nations. In the developing world, many public health infrastructures are still forming. There may not be enough trained health workers or monetary resources to provide even a basic level of medical care and disease prevention. As a result, a large majority of disease and mortality in the developing world results from and contributes to extreme poverty. In many countries in Africa, governments spend less than USD$10 per person on healthcare, while, in the United States, the federal government spent approximately USD$4,500 per capita in 2000.
Many diseases are preventable through simple, non-medical methods. Public health plays a very important role in prevention efforts in the developing world, either through the local health system or through international non-governmental organizations.
The major postgraduate degree related to this field is the Master of Public Health (M.P.H.) or Master of Health Science, while the United States medical residency specialty is General Preventive Medicine and Public Health.
History of public health
In some ways, public health is a modern concept, although it has roots in antiquity. From the early beginnings of human civilization, it was recognized that polluted water and lack of proper waste disposal may spread vector-borne diseases. Early religions attempted to regulate behavior that specifically related to health, from types of food eaten, to the extent which certain behaviors could be indulged, such as drinking alcohol or sexual relations. The establishment of governments placed responsibility on leaders to develop public health policies and programs to gain some understanding of the causes of disease to ensure stability, prosperity, and maintain order.
Early public health interventions
By Roman times, it was well understood that proper diversion of human waste was a necessary tenet of public health in urban areas. The Chinese developed the practice of variolation following a smallpox epidemic around 1000 B.C.E. An individual without the disease could gain some measure of immunity against it by inhaling the dried crusts that formed around lesions of infected individuals. Also, children were protected by innoculating a scratch on their forearms with the pus from a lesion. This practice was not documented in the West until the early-1700s, and was used on a very limited basis. The practice of vaccination did not become prevalent until the 1820s, following the work of Edward Jenner to treat smallpox.
During the 14th century Black Death in Europe, it was believed that removing bodies of the dead would further prevent the spread of the bacterial infection. This did little to stem the plague, however, which was actually spread by rodent-borne fleas. Burning areas of cities resulted in much greater benefit, since it removed the rodent infestations. The development of quarantine in the medieval period helped mitigate the effects of other infectious diseases. However, according to Michel Foucault, the plague model of governmentality was to be opposed to the later cholera model. Cholera, which second pandemic devastated Europe between 1829 and 1851, was first fought by the use of what Foucault called "social medecine", which focused on flux, circulation of air, location of cemeteries, etc. All those concerns were thus mixed with urbanistic concerns of the management of populations, which Foucault designed by the concept of "biopower".
The science of epidemiology was founded by John Snow's identification of a polluted public water well as the cause of an 1854 cholera outbreak in London. John believed in the germ theory of disease as opposed to the prevailing miasma theory. Although miasma theory taught correctly that disease is a result of poor sanitation, it was based only upon the prevailing theory of spontaneous generation. Microorganisms, which are now known to cause many of the most common infectious diseases, were first observed around 1680 by Anton van Leeuwenhoek. But the modern era of public health did not begin until the 1880s, when the culmination of Robert Koch's germ theory and Louis Pasteur's production of artificial vaccines revolutionized the study of infectious disease.
Modern public health
As the rate of infectious diseases in the developed world decreased through the 20th century, public health began to put more focus on chronic diseases such as cancer and heart disease. Meanwhile, the developing world remained plagued by largely preventable infectious diseases, exacerbated by malnutrition and poverty.
Since the 1980s, the growing field of population health has broadened the focus of public health from individual behaviors and risk factors to population-level issues such as inequality, poverty, and education. Richard Wilkinson has been a major contributor to this area of study.
Modern public health is often concerned with the addressing determinants of health across a population, rather than advocating for individual behaviour change. There is a recognition that our health is affected by many factors including where we live, genetics, our income, our educational status and our social relationships - these are known as "social determinants of health." A social gradient in health runs through society, with those that are poorest generally suffering the worst health. However even those in the middle classes will generally have worse health outcomes than those of a higher social stratum (WHO, 2003). The new public health seeks to address these health inequalities by advocating for population-based policies that improve the health of the whole population in an equitable fashion.
With the passing of the years, the increasing of natural disasters, and the threats of terrorism with WMD (Weapons of Mass Destruction), the Department of Defense of United States, must take measures to stay alert and prepare for a possible major incident in our Nation. Experiences like the one on September 11, 2001 is one of the motivation in creating a NRP (National Response Plan) on December 2004, where all our Health Care System and the EMS (Emergency Management System) together with Federal, State, Local, tribal, private-sector, and nongovernmental organizations will be unified in the same plan. The Public Health Department has a new challenge to integrate in their program to a solid knowledge of prevention, preparedness, response, and recovery in case of a natural disaster, terrorism attack or other emergency situation inside of the United States Homeland Security. Public Health and Medical services as part of the Emergency Support Function will work together in detailing the missions, policies, structures, and responsibilities. Due to the constant changes in our life and lifestyles, Public Health Department will keep working and functioning according to all those challenges for the wellbeing of the American people.
Public health programs
Today, most governments recognize the importance of public health programs in reducing the incidence of disease, disability, and the effects of aging, although public health generally receives significantly less government funding compared with medicine. In recent years, public health programs providing vaccinations have made incredible strides in promoting health, including the eradication of smallpox, a disease that plagued humanity for thousands of years.
One of the most important public health issues facing the world currently is HIV/AIDS. Tuberculosis, which claimed the lives of authors Franz Kafka and Charlotte Bronte, and composer Franz Schubert, among others, is also reemerging as a major concern due to the rise of HIV/AIDS-related infections and the development of strains resistant to standard antibiotics.
A controversial aspect of public health is that related to the control of smoking. Many nations have implemented major initiatives to cut smoking, such as increased taxation and bans on smoking in some or all public places. Proponents argue that smoking is one of the major killers in all developed countries, and that they have a duty to reduce the death rate, both through limiting passive smoking and by providing fewer opportunities for smokers to smoke. Opponents say that this undermines individual freedom and personal responsibility, (often using the phrase nanny state in the UK) and worrying that the state may take power to remove more and more choice in the name of better population health overall.
Population health
Population health is an approach to health that aims to improve the health of an entire population. One major step in achieving this aim is to reduce health inequities among population groups. Population health seeks to step beyond the individual-level focus of mainstream medicine and public health by addressing a broad range of factors that impact health on a population-level, such as environment, social structure, resource distribution, etc. An important theme in population health is importance of social determinants of health and the relatively minor impact that medicine and healthcare have on improving health overall.
From a population health perspective, health has been defined not simply as a state free from disease but as "the capacity of people to adapt to, respond to, or control life's challenges and changes" (Frankish et al., 1996).
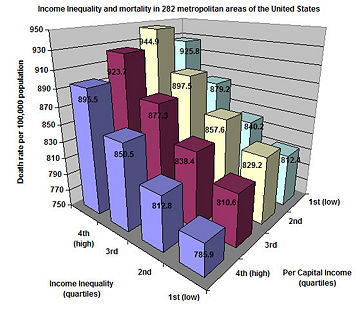
Recently, there has been increasing interest from epidemiologists on the subject of economic inequality and its relation to the health of populations. There is a very robust correlation between socioeconomic status and health. This correlation suggests that it is not only the poor who tend to be sick when everyone else is healthy, but that there is a continual gradient, from the top to the bottom of the socioeconomic ladder, relating status to health. This phenomenon is often called the "SES Gradient". Lower socioeconomic status has been linked to chronic stress, heart disease, ulcers, type 2 diabetes, rheumatoid arthritis, certain types of cancer, and premature aging.
Despite the reality of the SES Gradient, there is debate as to its cause. A number of researchers (A. Leigh, C. Jencks, A. Clarkwest - see also Russell Sage working papers) see a definite link between economic status and mortality due to the greater economic resources of the better-off, but they find little correlation due to social status differences.
Other researchers such as Richard Wilkinson, J. Lynch , and G.A. Kaplan have found that socioeconomic status strongly affects health even when controlling for economic resources and access to health care. Most famous for linking social status with health are the Whitehall studies - a series of studies conducted on civil servants in London. The studies found that, despite the fact that all civil servants in England have the same access to health care, there was a strong correlation between social status and health. The studies found that this relationship stayed strong even when controlling for health-effecting habits such as exercise, smoking and drinking. Furthermore, it has been noted that no amount of medical attention will help decrease the likelihood of someone getting type 1 diabetes or rheumatoid arthritis - yet both are more common among populations with lower socioeconomic status. Lastly, it has been found that amongst the wealthiest quarter of countries on earth (a set stretching from Luxembourg to Slovakia) there is no relation between a country's wealth and general population health [4] - suggesting that past a certain level, absolute levels of wealth have little impact on population health, but relative levels within a country do.
The concept of psychosocial stress attempts to explain how psychosocial phenomenon such as status and social stratification can lead to the many diseases associated with the SES Gradient. Higher levels of economic inequality tend to intensify social hierarchies and generally degrades the quality of social relations - leading to greater levels of stress and stress related diseases. Richard Wilkinson found this to be true not only for the poorest members of society, but also for the wealthiest. Economic inequality is bad for everyone's health.
Inequality does not only affect the health of human populations. David H. Abbott at the Wisconsin National Primate Research Center found that among many primate species, less egalitarian social structures correlated with higher levels of stress hormones among socially subordinate individuals. Research by Robert Sapolsky of Stanford University provides similar findings.
Notes and references
- World Health Organization, Constitution, World Health Organization, Geneva, 1946. Available online at http://w3.whosea.org/aboutsearo/pdf/const.pdf. Accessed October 24, 2005.
- WHO (1979) Health for All, Sr. Nos. 1, 2
- WHO Definition of Health Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference, 1946
- Control of Communicable Diseases Manual edited by James B. Chin, APHA, 2000
- Encyclopedia of public health edited by Lester Breslow, Macmillan Reference 2002
- The Solid Facts: Social Determinants of Health edited by Richard Wilkinson and Michael Marmot, WHO, 2003
- CCC. (2006), Public Health Emergency Response Guide for State, Local, and Tribal Public Health Directors. Retrieved April10, 2006, from: http://www.bt.cdc.gov/planning/responseguide.asp
- Department of Homeland Security (2004) National Response Plan. Retrieved April 11, 2006, from http://www.dhs.gov/interweb/assetlibrary/NRPbaseplan.pdf
- Frankish, CJ et al. "Health Impact Assessment as a Tool for Population Health Promotion and Public Policy." Institute of Health Promotion Research, University of British Columbia, Vancouver: 1996.
External links
- World Health Organization
- National Center for Health Statistics (USA)
- 'Your-Health-Articles' contains extensive authors though not necessarily accredited
- National Institute of Health (USA)
- Centers for Disease Control and Prevention (USA)
- Health news blog
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.
