Sciatica
| Sciatica Classification and external resources | |
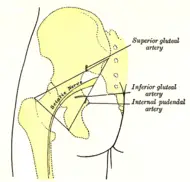
| Left gluteal region, showing surface markings for arteries and sciatic nerve. | |
| ICD-10 | M54.3-M54.4 |
| ICD-9 | 724.3 |
| eMedicine | emerg/303 |
| MeSH | D012585 |
SCIATICA
Sciatica is otherwise known as Sciatic nerve dysfunction or lumbar radiculopathy. This condition occurs when the sciatic nerve, which is the longest nerve in the body, becomes inflamed due to injury or compression.
The sciatic nerve is the primary nerve of the leg, orginating from the back of the pelvis and extending through the buttocks and down the back of the thighs. This nerve controls the muscles of the back of the knee and lower leg and provides sensation to the back of the thigh, part of the lower leg and the sole of the foot.
Sciatica involves pain, weakness, numbness in the lower back and legs. Some also experience a tingling sensation in the legs. It is a form of peripheral neuropathy.
A problem in a single nerve group, such as the sciatic nerve, is classified as a mononeuropathy. But when the nerve is partially damaged, the effects may seem similar to conditions such as tibial nerve dysfunction or common peroneal nerve dysfunction, which arise when certain branches of the Sciatic nerve are damaged. A ruptured lumbar disk in the spine may also cause symptoms that simulate the symptoms of sciatic nerve dysfunction.
Causes
Sciatica is usually caused by a prolapsed disk in the spine that presses on the sciatic nerve.
Discs are rings with tough exteriors and soft inside, which are located between the bones of the spine and function as shock absorbers. When a weak disc herniates (buges out), the bulge presses or even crushes the sciatic nerve, causing Sciatica.
Discs can become strained and weak because of a number of reasons:
- Twisting and bending movements
- Heavy lifting
- Bad posture
- Pregnancy
- Obesity
Other medical conditions may also put pressure on the sciatic nerve:
- Diabetes
- Tumor
- Abscess
- Blood clot or bleeding in the pelvis
- Nerve disorders
Causes also include direct trauma inflicted by an injection into the buttocks, fractures on the pelvis, gunshot wounds, prolonged external pressure on the nerve, pressure on the nerve from nearby body structures and nerve entrapment, which occurs when pressure is applied on the nerve when it passes through a narrow structure. The damage slows or prevents conduction of impulses through the nerve.
There are cases when the definite cause for Sciatica cannot be identified.
Risks
Sciatica may lead to complications such as:
- Partial or complete loss of leg movement
- Partial or complete loss of sensation in the leg
- Recurrent or unnoticed injury to the leg
- Side effects from medications such as painkillers
Signs & Symptoms
Dull, mild pain to sharp, extreme pain may occur anywhere along the entire length of the Sciatic nerve. The pain could lasts for weeks or occur only now and then, especially when sneezing or coughing. Physical activity may make the pain more intense.
Other symtoms include:
- Numbness
- Burning sensation
- Tingling sensation (known as pins and needles)
- Weakness in the affected area
- Difficulty in walking
- Inability to move the foot
- Inability to bend the knee
Each individual may experience symptoms differently. For some, the symptoms are worse at night.
Diagnosis
Diagnostic procedures for Sciatica begin with analysis of the patient’s complete medical history and symptoms, and a physical examination. The patient may also be put through a number of flexibility and muscle-strength tests. This is followed by and a set of laboratory tests.
A neuromuscular examination of the legs could reveal:
- Weakness of knee bending or foot movement
- Difficulty bending the foot inward or down
- Anormality in reflexes with weak or absent ankle-jerk reflex
- Pain down the leg reproduced while lifting the leg straight up off the examining table
Clinical tests that reveal sciatic nerve dysfunction may include:
- EMG (a recording of electrical activity in muscles)
- Nerve conduction tests
- Blood tests
- X-rays
- CT scans
- MRI imaging
These test are also used to pinpoint the affected area of the spine and to rule out more severe spinal problems.
Treatment
Specific treatment for sciatica will be determined by factors such as:
- Age
- Overall health
- Medical history
- Extent of the disease
- Expectations for the course of the disease
- The patient’s tolerance / preference for specific medications, procedures or therapies
In some cases, no treatment is required and recovery is spontaneous. Where Sciatica heals on its own with rest and time.
But if the condition persists, treatment is required to relieve pain and maximize mobility:
Pain Relief
To keep the patient comfortable, nonsteroidal anti-inflammatory drugs or pain killers are prescribed. Depending on the severity of the condition, these may vary from a simple analgesic to phenytoin, carbamazepine, or tricyclic antidepressants such as amitriptyline. Applying heat or cold to the affected area may also help.
When pain is so severe that the person is disabled, an epidural is administered. This is injected in the spine to bring quick relief. Though steroids may help with nerve inflammation, their use should be avoided or minimized to reduce the risk of medication side effects.
Physical Activity
Exercise goes a long way in helping reduce inflammation in the sciatic nerve. Walking, stretching and resuming normal work is sufficient for most. Though additional physical therapy exercises are recommended for some in order to maintain muscle strength.
The use of braces, splints, orthopedic shoes or other supportive devices may help compensate for lost or impaired function. Vocational counseling, occupational therapy, occupational changes, job retraining or similar interventions may also be recommended.
Surgery
This is recommended only if sciatica becomes overwhelming and lasts for a prolonged period. Surgery to repair the prolapsed disk will involve removing a part of the bulging disc, so that it is no longer pressing against the nerve.
Prevention
Prevention varies depending on the cause of the nerve damage. But, generally avoid prolonged sitting or lying with pressure on the buttocks.
Some form of regular exercises can also help prevent this condition.
ReferencesISBN links support NWE through referral fees
Retrieved from:
• “http://www.uchospitals.edu”
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.