Difference between revisions of "Antibiotic" - New World Encyclopedia
| Line 1: | Line 1: | ||
{{Contracted}} | {{Contracted}} | ||
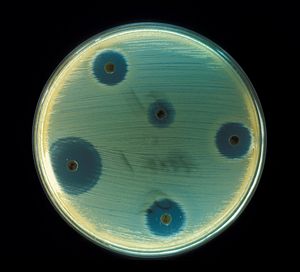
| − | [[Image:Staphylococcus aureus (AB Test).jpg|right|thumb|300px|'' | + | [[Image:Staphylococcus aureus (AB Test).jpg|right|thumb|300px|''Staphylococcus aureus'' - Antibiotics test plate.]] |
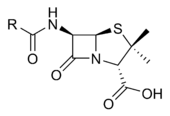
An '''antibiotic''' is a drug that kills or prevents the growth of [[bacterium|bacteria]]. They have no effect against viruses, fungi, or parasites. Antibiotics are one class of antimicrobials, a larger group which also includes anti-viral, anti-fungal, and anti-parasitic drugs. They are relatively harmless to the host, and therefore can be used to treat infections. The term, coined by Selman Waksman, originally described only those formulations derived from living organisms, in contrast to "chemotherapeutic agents", which are purely synthetic. Nowadays the term "antibiotic" is also applied to synthetic antimicrobials, such as the sulfa drugs. Antibiotics are generally small [[molecule]]s with a molecular weight less than 2000. They are not [[enzyme]]s. Some antibiotics have been derived from mold, for example the [[penicillin|penicillin class]]. | An '''antibiotic''' is a drug that kills or prevents the growth of [[bacterium|bacteria]]. They have no effect against viruses, fungi, or parasites. Antibiotics are one class of antimicrobials, a larger group which also includes anti-viral, anti-fungal, and anti-parasitic drugs. They are relatively harmless to the host, and therefore can be used to treat infections. The term, coined by Selman Waksman, originally described only those formulations derived from living organisms, in contrast to "chemotherapeutic agents", which are purely synthetic. Nowadays the term "antibiotic" is also applied to synthetic antimicrobials, such as the sulfa drugs. Antibiotics are generally small [[molecule]]s with a molecular weight less than 2000. They are not [[enzyme]]s. Some antibiotics have been derived from mold, for example the [[penicillin|penicillin class]]. | ||
| Line 308: | Line 308: | ||
Common forms of antibiotic misuse include failure to take the entire prescribed course of the antibiotic, usually because the patient feels better, but before the infecting organism is completely eradicated. In addition to treatment failure, these practices can result in antibiotic resistance in which the bacteria survive the abbreviated treatment. Taking antibiotics in inappropriate situations is another common form of antibiotic misuse. Common examples of this would be the use of antibacterials for viral infections such as the [[common cold]]. | Common forms of antibiotic misuse include failure to take the entire prescribed course of the antibiotic, usually because the patient feels better, but before the infecting organism is completely eradicated. In addition to treatment failure, these practices can result in antibiotic resistance in which the bacteria survive the abbreviated treatment. Taking antibiotics in inappropriate situations is another common form of antibiotic misuse. Common examples of this would be the use of antibacterials for viral infections such as the [[common cold]]. | ||
| − | Currently, it is estimated that greater than 50% of the antibiotics used in the U.S. are given to food animals (e.g. chickens, pigs and cattle) in the absence of disease.<ref>Mellon, M ''et al''. (2001) ''Hogging It!: Estimates of Antimicrobial Abuse in Livestock'', 1st ed. Cambridge, MA: | + | Currently, it is estimated that greater than 50% of the antibiotics used in the U.S. are given to food animals (e.g. chickens, pigs and cattle) in the absence of disease.<ref>Mellon, M ''et al''. (2001) ''Hogging It!: Estimates of Antimicrobial Abuse in Livestock'', 1st ed. Cambridge, MA: Union of Concerned Scientists.</ref> Antibiotic use in food animal production has been associated with the emergence of antibiotic resistant strains of bacteria including Salmonella, Campylobacter, Escherichia coli and Enterococcus among others. There is substantial evidence from the US and the EU that these resistant bacteria cause antibiotic resistant infections in humans. The American Society for Microbiology (ASM), the American Public Health Association (APHA) and the American Medical Association (AMA) have called for substantial restrictions on antibiotic use in food animal production including an end to all non-therapeutic uses. The food animal and pharmaceutical industries have fought hard to prevent new regulations that would limit the use of antibiotics in food animal production. For example, in 2000 the US Food and Drug Administration (FDA) announced their intention to rescind approval for fluoroquinolone use in poultry production because of substantial evidence linking it to the emergence of fluoroquinolone resistant Campylobacter infections in humans. The final decision to ban fluoroquinolones from use in poultry production was not made until 5 years later because of challenges from the food animal and pharmaceutical industries. Today, there are two federal bills (S.742 and H.R. 2562) aimed at phasing out non-therapeutic antibiotics in US food animal production. These bills are endorsed by many public health and medical organizations including the American Nurses Association (ANA), the American Academy of Pediatrics (AAP), and the American Public Health Association (APHA). |
Excessive use of prophylactic antibiotics in travelers may also be classified as misuse. | Excessive use of prophylactic antibiotics in travelers may also be classified as misuse. | ||
| Line 314: | Line 314: | ||
== Antibiotic resistance == | == Antibiotic resistance == | ||
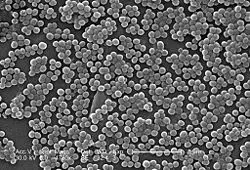
| − | + | [[Image:MRSA7820.jpg|right|thumb|250px|SEM depicting methicillin-resistant ''Staphylococcus aureus'' bacteria.]] | |
| − | + | Use or misuse of antibiotics may result in the development of ''antibiotic resistance'' by the infecting organisms, similar to the development of pesticide resistance in insects. Evolutionary theory of genetic selection requires that as close as possible to 100% of the infecting organisms be killed off to avoid selection of resistance; if a small subset of the population survives the treatment and is allowed to multiply, the average susceptibility of this new population to the compound will be much less than that of the original population, since they have descended from those few organisms which survived the original treatment. This survival often results from an inheritable resistance to the compound which was infrequent in the original population but is now much more frequent in the descendants thus selected entirely from those originally infrequent resistant organisms. | |
| − | + | [[Image:Cutaneous abscess MRSA staphylococcus aureus 7826 lores.jpg|right|thumb|250px|An abscess caused by methicillin-resistant ''Staphylococcus aureus'' bacteria (MRSA).]] | |
| − | [[ | + | Antibiotic resistance has become a serious problem in both the developed and underdeveloped nations. By 1984 half of the people with active [[tuberculosis]] in the [[United States]] had a strain that resisted at least one antibiotic. In certain settings, such as hospitals and some child-care locations, the rate of antibiotic resistance is so high that the normal, low cost antibiotics are virtually useless for treatment of frequently seen infections. This leads to more frequent use of newer and more expensive compounds, which in turn leads inexorably to the rise of resistance to those drugs, and a never-ending ever-spiraling race to discover new and different antibiotics ensues, just to keep us from losing ground in the battle against infection. The fear is that we will eventually fail to keep up in this race, and the time when people did not fear life-threatening bacterial infections will be just a memory of a golden era. |
| − | + | Another example of selection is ''Staphylococcus aureus'', which could be treated successfully with [[penicillin]] in the 1940s and 1950s. At present, nearly all strains are resistant to penicillin, and many are resistant to nafcillin, leaving only a narrow selection of drugs such as vancomycin useful for treatment. The situation is worsened by the fact that genes coding for antibiotic resistance can be transferred between bacteria, making it possible for bacteria never exposed to an antibiotic to acquire resistance from those which have. The problem of antibiotic resistance is worsened when antibiotics are used to treat disorders in which they have no efficacy, such as the common cold or other viral complaints, and when they are used widely as prophylaxis rather than treatment (as in, for example, animal feeds), because this exposes more bacteria to selection for resistance. | |
| − | |||
| − | Another example of selection is '' | ||
== Beyond antibiotics == | == Beyond antibiotics == | ||
| Line 332: | Line 330: | ||
Research into [[bacteriophage]]s is ongoing at the moment. Bacteriophages are a specific type of virus that only targets bacteria. Research suggests that nature has evolved several types of bacteriophage for each type of bacteria. While research into bacteriophages is only in its infancy the results are promising and have already lead to major advances in microscopic imaging.<ref>Purdue University "Biologists build better software, beat path to viral knowledge", see Imaging of Epsilon 15, a virus that infects the bacterium Salmonella [http://news.uns.purdue.edu/UNS/html4ever/2006/060201.Jiang.salmonella.html News report]</ref> While bacteriophages provide a possible solution to the problem of antibacterial resistance there is as of yet no proof that we will actually be able to deploy these microscopic killers in humans, we can only continue the research and see where it leads. | Research into [[bacteriophage]]s is ongoing at the moment. Bacteriophages are a specific type of virus that only targets bacteria. Research suggests that nature has evolved several types of bacteriophage for each type of bacteria. While research into bacteriophages is only in its infancy the results are promising and have already lead to major advances in microscopic imaging.<ref>Purdue University "Biologists build better software, beat path to viral knowledge", see Imaging of Epsilon 15, a virus that infects the bacterium Salmonella [http://news.uns.purdue.edu/UNS/html4ever/2006/060201.Jiang.salmonella.html News report]</ref> While bacteriophages provide a possible solution to the problem of antibacterial resistance there is as of yet no proof that we will actually be able to deploy these microscopic killers in humans, we can only continue the research and see where it leads. | ||
| − | + | Phage therapy has been used in the past on humans in the US and Europe during the 1920s and 1930s, however due to not fully understanding the mechanism by which phage therapy worked, these treatments had mixed results. With the discovery of penicillin in the 1940s, Europe and the US changed to using antibiotics. However, in the former Soviet Union phage therapies continued to be studied. In the Republic of Georgia, the Eliava Institute of Bacteriophage, Microbiology & Virology continues to research the use of phage therapy. Various companies and foundations in North America and Europe are currently researching phage therapies. | |
== References == | == References == | ||
| Line 343: | Line 341: | ||
* {{cite book | author=Baron, Samuel | title=Medical Microbiology, 4th ed. | publisher=The University of Texas Medical Branch at Galveston | year=1996 | id=ISBN 0-9631172-1-1 | url=http://www.ncbi.nlm.nih.gov/books/bv.fcgi?call=bv.View..ShowTOC&rid=mmed.TOC&depth=10 }} | * {{cite book | author=Baron, Samuel | title=Medical Microbiology, 4th ed. | publisher=The University of Texas Medical Branch at Galveston | year=1996 | id=ISBN 0-9631172-1-1 | url=http://www.ncbi.nlm.nih.gov/books/bv.fcgi?call=bv.View..ShowTOC&rid=mmed.TOC&depth=10 }} | ||
* {{cite book | author=Madigan, Michael; Martinko, John (editors)| title=Brock Biology of Microorganisms (11th ed.)| publisher=Prentice Hall | year=2005 | id=ISBN 0-13-144329-1}} | * {{cite book | author=Madigan, Michael; Martinko, John (editors)| title=Brock Biology of Microorganisms (11th ed.)| publisher=Prentice Hall | year=2005 | id=ISBN 0-13-144329-1}} | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
== External links == | == External links == | ||
Revision as of 18:02, 3 January 2007
An antibiotic is a drug that kills or prevents the growth of bacteria. They have no effect against viruses, fungi, or parasites. Antibiotics are one class of antimicrobials, a larger group which also includes anti-viral, anti-fungal, and anti-parasitic drugs. They are relatively harmless to the host, and therefore can be used to treat infections. The term, coined by Selman Waksman, originally described only those formulations derived from living organisms, in contrast to "chemotherapeutic agents", which are purely synthetic. Nowadays the term "antibiotic" is also applied to synthetic antimicrobials, such as the sulfa drugs. Antibiotics are generally small molecules with a molecular weight less than 2000. They are not enzymes. Some antibiotics have been derived from mold, for example the penicillin class.
Unlike previous treatments for infections, which included poisons such as strychnine and arsenic, antibiotics were labelled "magic bullets": drugs which targeted disease without harming the host. Conventional antibiotics are not effective in viral, fungal and other nonbacterial infections, and individual antibiotics vary widely in their effectiveness on various types of bacteria. Antibiotics can be categorized based on their target specificity: "narrow-spectrum" antibiotics target particular types of bacteria, such as Gram-negative or Gram-positive bacteria, while broad-spectrum antibiotics affect a larger range of bacteria.
The effectiveness of individual antibiotics varies with the location of the infection, the ability of the antibiotic to reach the site of infection, and the ability of the bacteria to resist or inactivate the antibiotic. Some antibiotics actually kill the bacteria (bactericidal), whereas others merely prevent the bacteria from multiplying (bacteriostatic) so that the host's immune system can overcome them.
Oral antibiotics are the simplest approach when effective, with intravenous antibiotics reserved for more serious cases. Antibiotics may sometimes be administered topically, as with eye drops or ointments.
Antibiotics can also be classified by the organisms against which they are effective, and by the type of infection in which they are useful, which depends on the sensitivities of the organisms that most commonly cause the infection and the concentration of antibiotic obtainable in the affected tissue.
History
Many ancient cultures, including the ancient Egyptians, ancient Greeks and ancient Chinese, already used molds and plants to treat infections. This worked because some moulds produce antibiotic substances. However, they couldn't distinguish or distill the active component in the moulds.
Modern research on antibiotics began in Britain with the discovery of Penicillin in 1928 by Alexander Fleming. More than ten years later, Ernst Chain and Howard Florey became interested in his work, and came up with the purified form of penicillin. The three shared the 1945 Nobel Prize in Medicine. "Antibiotic" was originally used to refer only to substances extracted from a fungus or other microorganism, but has come to include also the many synthetic and semi-synthetic drugs that have antibacterial effects.
Classes of antibiotics
At the highest level, antibiotics can be classified as either bactericidal or bacteriostatic. Bactericidals kill bacteria directly where bacteriostatics prevent them dividing. However, these classifications are based on laboratory behaviour; in practice, both of these will end a bacterial infection.
| Generic Name | Brand Names | Common Uses | Side Effects |
|---|---|---|---|
| Aminoglycosides | |||
| Amikacin | Amikin | Infections caused by Gram-negative bacteria, such as Escherichia coli and Klebsiella |
|
| Gentamicin | Garamycin | ||
| Kanamycin | |||
| Neomycin | |||
| Netilmicin | |||
| Streptomycin | |||
| Tobramycin | Nebcin | ||
| Carbacephem | |||
| Loracarbef | Lorabid | ||
| Carbapenems | |||
| Ertapenem | |||
| Imipenem/Cilastatin | Primaxin | ||
| Meropenem | |||
| Cephalosporins (First generation) | |||
| Cefadroxil | Duricef |
| |
| Cefazolin | Ancef | ||
| Cephalexin | Keflex | ||
| Cephalosporins (Second generation) | |||
| Cefaclor | Ceclor |
| |
| Cefamandole | Mandole | ||
| Cefoxitin | |||
| Cefprozil | Cefzil | ||
| Cefuroxime | Ceftin | ||
| Cephalosporins (Third generation) | |||
| Cefixime |
| ||
| Cefdinir | Omnicef | ||
| Cefditoren | |||
| Cefoperazone | Cefobid | ||
| Cefotaxime | Claforan | ||
| Cefpodoxime | |||
| Ceftazidime | Fortum | ||
| Ceftibuten | |||
| Ceftizoxime | |||
| Ceftriaxone | Rocephin | ||
| Cephalosporins (Fourth generation) | |||
| Cefepime | Maxipime |
| |
| Glycopeptides | |||
| Teicoplanin | |||
| Vancomycin | Vancocin | ||
| Macrolides | |||
| Azithromycin | Zithromax, Sumamed | Streptococcal infections, syphilis, respiratory infections, mycoplasmal infections, Lyme disease |
|
| Clarithromycin | Biaxin | ||
| Dirithromycin | |||
| Erythromycin | |||
| Roxithromycin | |||
| Troleandomycin | |||
| Monobactam | |||
| Aztreonam | |||
| Penicillins | |||
| Amoxicillin | Novamox | Wide range of infections; penicillin used for streptococcal infections, syphilis, and Lyme disease |
|
| Ampicillin | |||
| Azlocillin | |||
| Carbenicillin | |||
| Cloxacillin | |||
| Dicloxacillin | |||
| Flucloxacillin | |||
| Mezlocillin | |||
| Nafcillin | |||
| Penicillin | |||
| Piperacillin | |||
| Ticarcillin | |||
| Polypeptides | |||
| Bacitracin | Eye, ear or bladder infections; usually applied directly to the eye or inhaled into the lungs; rarely given by injection | Kidney and nerve damage (when given by injection) | |
| Colistin | |||
| Polymyxin B | |||
| Quinolones | |||
| Ciprofloxacin | Ciproxin, Ciplox | Urinary tract infections, bacterial prostatitis, bacterial diarrhea, gonorrhea | Nausea (rare) |
| Enoxacin | |||
| Gatifloxacin | Tequin | ||
| Levofloxacin | Levaquin | ||
| Lomefloxacin | |||
| Moxifloxacin | Avelox | ||
| Norfloxacin | |||
| Ofloxacin | Ocuflox | ||
| Trovafloxacin | Trovan | ||
| Sulfonamides | |||
| Mafenide | Urinary tract infections (except sulfacetamide and mafenide); mafenide is used topically for burns |
| |
| Prontosil (archaic) | |||
| Sulfacetamide | |||
| Sulfamethizole | |||
| Sulfanilimide (archaic) | |||
| Sulfasalazine | |||
| Sulfisoxazole | |||
| Trimethoprim | |||
| Trimethoprim-Sulfamethoxazole (Co-trimoxazole) (TMP-SMX) | Bactrim | ||
| Tetracyclines | |||
| Demeclocycline | Syphilis, chlamydial infections, Lyme disease, mycoplasmal infections, acne, rickettsial infections |
| |
| Doxycycline | Vibramycin | ||
| Minocycline | |||
| Oxytetracycline | |||
| Tetracycline | Sumycin | ||
| Others | |||
| Chloramphenicol | Chloromycetin | ||
| Clindamycin | Cleocin | ||
| Ethambutol | |||
| Fosfomycin | |||
| Furazolidone | |||
| Isoniazid | |||
| Linezolid | Zyvox | ||
| Metronidazole | Flagyl | ||
| Mupirocin | |||
| Nitrofurantoin | Macrodantin | ||
| Platensimycin | |||
| Pyrazinamide | |||
| Quinupristin/Dalfopristin | Syncercide | ||
| Rifampin | |||
| Spectinomycin | |||
| Generic Name | Brand Names | Common Uses | Side Effects |
Production
The production of antibiotics has been widespread since the pioneering efforts of Howard Walter Florey and Ernst Boris Chain in 1939. The importance of antibiotics to medicine has led to much research into discovering and producing them.
Identifying useful antibiotics
Despite the wide variety of known antibiotics, less than 1% of antimicrobial agents have any medical or commercial value. The most commonly known antibiotic, Penicillin has a highly selective toxicity and therapeutic index (as eukaryotic animal cells do not contain peptidoglycan, they are usually unaffected by it). This is not so for many antibiotics. Others simply lack advantage over the antibiotics already in use, or have no other practical applications.
In order to identify the useful antibiotics, a process of screening is often employed. Using this method, isolates of a large number of microorganisms are cultured and then tested for production of diffusible products which inhibit the growth of test organisms. However, the majority of the resulting antibiotics are already known and must therefore be disregarded. The remainders must be tested for their selective toxicities and therapeutic activities, and the best candidates can be examined and possibly modified.
A more modern version of this approach is a rational design program. This involves screening being directed towards finding new natural products that inhibit specific targets (e.g. a particular step of a metabolic pathway) on microorganisms, rather than tests to show general inhibition of a culture.
Industrial production techniques
Antibiotics are produced industrially by a process of fermentation, where the source microorganism is grown in large containers (100,000–150,000 liters or more) containing a liquid growth medium. Oxygen concentration, temperature, pH and nutrient levels must be optimal, and are closely monitored and adjusted if necessary. As antibiotics are secondary metabolites, the population size must be controlled very carefully to ensure that maximum yield is obtained before the cells die. Once the process is complete, the antibiotic must be extracted and purified to a crystalline product. This is simpler to achieve if the antibiotic is soluble in organic solvent. Otherwise it must first be removed by ion exchange, adsorption or chemical precipitation.
Strains used for production
Microorganisms used in fermentation are rarely identical to the wild type. This is because species are often genetically modified to yield the maximum amounts of antibiotics. Mutation is often used, and is encouraged by introducing mutagens such as ultraviolet radiation, x-rays or certain chemicals. Selection and further reproduction of the higher yielding strains over many generations can raise yields by 20-fold or more. Another technique used to increase yields is gene amplification, where copies of genes coding for proteins involved in the antibiotic production can be inserted back into a cell, via vectors such as plasmids. This process must be closely linked with retesting of antibiotic production and effectiveness.
Side effects
Possible side effects are varied, and range from fever and nausea to major allergic reactions. One of the more common side effects is diarrhea, sometimes caused by the anaerobic bacterium Clostridium difficile, which results from the antibiotic disrupting the normal balance of intestinal flora[2], (which some people believe may be re-balanced by taking probiotics). Other side effects can result from interaction with other drugs, such as elevated risk of tendon damage from administration of a quinolone antibiotic with a systemic corticosteroid.
It is a common assertion that some antibiotics can interfere with the efficiency of birth control pills. Although there remain few known cases of complication, the majority of antibiotics do not interfere with oral contraception, despite widespread misinformation to the contrary.[3]
Antibiotic misuse
Common forms of antibiotic misuse include failure to take the entire prescribed course of the antibiotic, usually because the patient feels better, but before the infecting organism is completely eradicated. In addition to treatment failure, these practices can result in antibiotic resistance in which the bacteria survive the abbreviated treatment. Taking antibiotics in inappropriate situations is another common form of antibiotic misuse. Common examples of this would be the use of antibacterials for viral infections such as the common cold.
Currently, it is estimated that greater than 50% of the antibiotics used in the U.S. are given to food animals (e.g. chickens, pigs and cattle) in the absence of disease.[4] Antibiotic use in food animal production has been associated with the emergence of antibiotic resistant strains of bacteria including Salmonella, Campylobacter, Escherichia coli and Enterococcus among others. There is substantial evidence from the US and the EU that these resistant bacteria cause antibiotic resistant infections in humans. The American Society for Microbiology (ASM), the American Public Health Association (APHA) and the American Medical Association (AMA) have called for substantial restrictions on antibiotic use in food animal production including an end to all non-therapeutic uses. The food animal and pharmaceutical industries have fought hard to prevent new regulations that would limit the use of antibiotics in food animal production. For example, in 2000 the US Food and Drug Administration (FDA) announced their intention to rescind approval for fluoroquinolone use in poultry production because of substantial evidence linking it to the emergence of fluoroquinolone resistant Campylobacter infections in humans. The final decision to ban fluoroquinolones from use in poultry production was not made until 5 years later because of challenges from the food animal and pharmaceutical industries. Today, there are two federal bills (S.742 and H.R. 2562) aimed at phasing out non-therapeutic antibiotics in US food animal production. These bills are endorsed by many public health and medical organizations including the American Nurses Association (ANA), the American Academy of Pediatrics (AAP), and the American Public Health Association (APHA).
Excessive use of prophylactic antibiotics in travelers may also be classified as misuse.
Antibiotic resistance
Use or misuse of antibiotics may result in the development of antibiotic resistance by the infecting organisms, similar to the development of pesticide resistance in insects. Evolutionary theory of genetic selection requires that as close as possible to 100% of the infecting organisms be killed off to avoid selection of resistance; if a small subset of the population survives the treatment and is allowed to multiply, the average susceptibility of this new population to the compound will be much less than that of the original population, since they have descended from those few organisms which survived the original treatment. This survival often results from an inheritable resistance to the compound which was infrequent in the original population but is now much more frequent in the descendants thus selected entirely from those originally infrequent resistant organisms.
Antibiotic resistance has become a serious problem in both the developed and underdeveloped nations. By 1984 half of the people with active tuberculosis in the United States had a strain that resisted at least one antibiotic. In certain settings, such as hospitals and some child-care locations, the rate of antibiotic resistance is so high that the normal, low cost antibiotics are virtually useless for treatment of frequently seen infections. This leads to more frequent use of newer and more expensive compounds, which in turn leads inexorably to the rise of resistance to those drugs, and a never-ending ever-spiraling race to discover new and different antibiotics ensues, just to keep us from losing ground in the battle against infection. The fear is that we will eventually fail to keep up in this race, and the time when people did not fear life-threatening bacterial infections will be just a memory of a golden era.
Another example of selection is Staphylococcus aureus, which could be treated successfully with penicillin in the 1940s and 1950s. At present, nearly all strains are resistant to penicillin, and many are resistant to nafcillin, leaving only a narrow selection of drugs such as vancomycin useful for treatment. The situation is worsened by the fact that genes coding for antibiotic resistance can be transferred between bacteria, making it possible for bacteria never exposed to an antibiotic to acquire resistance from those which have. The problem of antibiotic resistance is worsened when antibiotics are used to treat disorders in which they have no efficacy, such as the common cold or other viral complaints, and when they are used widely as prophylaxis rather than treatment (as in, for example, animal feeds), because this exposes more bacteria to selection for resistance.
Beyond antibiotics
Unfortunately, the comparative ease of finding compounds which safely cured bacterial infections proved much harder to duplicate with respect to fungal and viral infections. Antibiotic research led to great strides in our knowledge of basic biochemistry and to the current biological revolution; but in the process it was discovered that the susceptibility of bacteria to many compounds which are safe to humans is based upon significant differences between the cellular and molecular physiology of the bacterial cell and that of the mammalian cell. In contrast, despite the seemingly huge differences between fungi and humans, the basic biochemistries of the fungal cell and the mammalian cell are much more similar; so much so that there are few therapeutic opportunities for compounds to attack a fungal cell which will not harm a human cell. Similarly, we know now that viruses represent an incredibly minimal intracellular parasite, being stripped down to a few genes worth of DNA or RNA and the minimal molecular equipment needed to enter a cell and actually take over the machinery of the cell to produce new viruses. Thus, the great bulk of viral metabolic biochemistry is not merely similar to human biochemistry, it actually is human biochemistry, and the possible targets of antiviral compounds are restricted to the relatively very few components of the actual virus itself.
Research into bacteriophages is ongoing at the moment. Bacteriophages are a specific type of virus that only targets bacteria. Research suggests that nature has evolved several types of bacteriophage for each type of bacteria. While research into bacteriophages is only in its infancy the results are promising and have already lead to major advances in microscopic imaging.[5] While bacteriophages provide a possible solution to the problem of antibacterial resistance there is as of yet no proof that we will actually be able to deploy these microscopic killers in humans, we can only continue the research and see where it leads.
Phage therapy has been used in the past on humans in the US and Europe during the 1920s and 1930s, however due to not fully understanding the mechanism by which phage therapy worked, these treatments had mixed results. With the discovery of penicillin in the 1940s, Europe and the US changed to using antibiotics. However, in the former Soviet Union phage therapies continued to be studied. In the Republic of Georgia, the Eliava Institute of Bacteriophage, Microbiology & Virology continues to research the use of phage therapy. Various companies and foundations in North America and Europe are currently researching phage therapies.
ReferencesISBN links support NWE through referral fees
- ↑ Robert Berkow (ed.) The Merck Manual of Medical Information - Home Edition. Pocket (September 1999), ISBN 0-671-02727-1.
- ↑ University of Michigan Health System: Antibiotic-Associated Diarrhea, November 26, 2006
- ↑ Planned Parenthood: Does taking antibiotics make the pill less effective?, July 15, 2004
- ↑ Mellon, M et al. (2001) Hogging It!: Estimates of Antimicrobial Abuse in Livestock, 1st ed. Cambridge, MA: Union of Concerned Scientists.
- ↑ Purdue University "Biologists build better software, beat path to viral knowledge", see Imaging of Epsilon 15, a virus that infects the bacterium Salmonella News report
- Baron, Samuel (1996). Medical Microbiology, 4th ed.. The University of Texas Medical Branch at Galveston. ISBN 0-9631172-1-1.
- Madigan, Michael; Martinko, John (editors) (2005). Brock Biology of Microorganisms (11th ed.). Prentice Hall. ISBN 0-13-144329-1.
External links
- Antibiotic News from Genome News Network (GNN)
- Bruce Sterling's Bitter Resistance
- JAAPA: New antibiotics useful in primary care
- A new method for controlling bacterial activity without antibiotics - Research conducted at the Hebrew University
Resources
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.