Difference between revisions of "Hormone" - New World Encyclopedia
| Line 1: | Line 1: | ||
{{Claimed}} | {{Claimed}} | ||
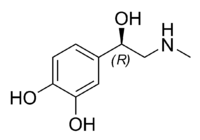
[[Image:Adrenaline_chemical_structure.png|right|thumb|[[Epinephrine]] (adrenaline), a [[catecholamine]]-type hormone |200px]] | [[Image:Adrenaline_chemical_structure.png|right|thumb|[[Epinephrine]] (adrenaline), a [[catecholamine]]-type hormone |200px]] | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
Hormone effects vary widely, but can include: | Hormone effects vary widely, but can include: | ||
| Line 21: | Line 15: | ||
Many of the responses to hormone signals can be described as serving to [[homeostasis|regulate]] metabolic activity of an organ or tissue. | Many of the responses to hormone signals can be described as serving to [[homeostasis|regulate]] metabolic activity of an organ or tissue. | ||
| − | |||
Hormonal signaling across this hierarchy involves the following: | Hormonal signaling across this hierarchy involves the following: | ||
| Line 32: | Line 25: | ||
As can be inferred from the hierarchical diagram, hormone biosynthetic cells are typically of a specialized cell type, residing within a particular [[endocrine system | endocrine gland]] (e.g. the [[thyroid gland]], [[ovary|ovaries]] or [[testes]]). Hormones may exit their cell of origin via [[exocytosis]] or another means of [[cell membrane|membrane transport]]. | As can be inferred from the hierarchical diagram, hormone biosynthetic cells are typically of a specialized cell type, residing within a particular [[endocrine system | endocrine gland]] (e.g. the [[thyroid gland]], [[ovary|ovaries]] or [[testes]]). Hormones may exit their cell of origin via [[exocytosis]] or another means of [[cell membrane|membrane transport]]. | ||
| + | |||
| + | ==Types of signalling== | ||
| + | In animals, there are three types of signaling by extracellular, secreted molecules—[[endocrine]], [[paracrine]], or [[autocrine]]—based on the distance over which the signal acts. | ||
| + | |||
| + | Hormones belong to the first type: they act on target cells distant from their site of synthesis by cells of the endocrine organs. In animals, an endocrine hormone is usually carried by the blood from its site of release to the target cell. | ||
| + | |||
| + | Paracrine signaling molecules only affect target cells in close proximity (an example is the conduction of an impulse), while autocrine cells respond to substances that they themselves release. | ||
| + | |||
| + | However, the designations above are not so clear cut, as some compounds can act in two or even three types of signaling. For example, certain small peptides function both as neurotransmitters (paracrine signaling) and as hormones (endocrine signaling) that operate over longer distances. These neurohormones – definition TK. | ||
| + | |||
| + | A '''neurohormone''' is any [[hormone]] produced by [[neurosecretory]] [[cells]], usually in the [[brain]]. Neurohormonal activity is distinguished from that of classical [[neurotransmitters]] as it can have effects on cells distant from the source of the hormone. | ||
| + | |||
| + | '''Neuroendocrine''' cells are a specialized group of nerve cells ([[neurons]]) that produce [[hormones]]. These hormones may be [[amines]], [[neuropeptides]], or specialized [[amino acids]]. They package the hormones in [[vesicle (biology)|vesicles]] and send these packages via long processes ([[axon|axons]]) to blood vessels. When stimulated (by [[hormones]] from the blood stream or other neurons) the neuroendocrine cells secrete the hormones into the blood stream. The hormones then travel to their target cells and may stimulate, inhibit or maintain function of these cells. The [[target cells]] may feed back information to these neurons that regulates further secretion. | ||
| + | |||
| + | Specialized groups of neuroendocrine cells can be found at the base of the [[third ventricle]] in the brain (in a region called the [[hypothalamus]]). This area controls most anterior [[pituitary]] cells and thereby regulates functions in the entire body, like responses to stress, cold, sleep, and the reproductive system. The neurons send processes to a region connecting to the pituitary stalk and the hormones (called releasing or [[inhibiting hormones]]) are released into the blood stream. They are carried by portal vessels to the pituitary cells where they may stimulate, inhibit, or maintain the function of a particular cell type. Many of the projects in the neuroendocrine group focus on the regulatory circuitry in this pathway. | ||
| + | |||
| + | The endocrine system works in close relation with the nervous system. It links the brain to the organs that control various aspects of the body. In addition, neurohormones are released by specialized groups of neurons in the brain. These function similarly to hormones and are often categorized into three major groups: catecholamines; hypothalamic neurohormones that monitor hormone release from the anterior pituitary; and hypothalamic neurohormones that monitor hormone release from the posterior pituitary. Neuroendocrinology is an area of medicine that focuses on the overlapping fields between the nervous and endocrine systems. | ||
| + | |||
| + | ==Overview== | ||
| + | what goes here? | ||
| + | |||
| + | Communication usually involves six steps | ||
| + | 1. synthesis | ||
| + | 2. release of the sig mol by the sig cell | ||
| + | 3. transport to target cell | ||
| + | 4. detection of signal by a specific receptor protein | ||
| + | 5. change in cellular metabolism or gene expression triggered by receptor-signaling complex | ||
| + | 6. removal of the signal, often terminating the cellular response | ||
| + | |||
| + | ==Hormones in action== | ||
| + | detail mechanisms | ||
| + | |||
| + | technical term for the signaling molecule (whether a hormone, neurotransmitter, or what have you) is ‘’ligand,’’ which binds to, or “fits” a site on the receptor protein, which is located on the surface of a target cell or in its nucleus or cytosol; binding causes a conformational change that initiates a sequence of reactions leading to a change in cellular function | ||
| + | |||
| + | diff cells respond differently to the same ligand, and diff receptor-ligand complexes can induce the same response in some cell types (ex of glucagons and epinephrine in liver cells, p 856) | ||
| + | |||
| + | a word on role of second messengers (intracellular signaling molecules) | ||
==Classification== | ==Classification== | ||
| Line 78: | Line 108: | ||
Peptide hormones are made and stored in vesicles within cells until they receive a signal for secretion. Initially, peptide hormones are made as preprohormones, which are inactive, and then are converted into prohormones. These prohormones are then cut into active hormones and peptide pieces, which are all secreted together. Because of their hydrophilic (water loving) nature, peptide hormones travel freely in the blood as they dissolve. They experience short half lives and tend to bind to surface cell receptors to initiate quick cellular responses. Peptide hormones can cause the synthesis of new proteins. | Peptide hormones are made and stored in vesicles within cells until they receive a signal for secretion. Initially, peptide hormones are made as preprohormones, which are inactive, and then are converted into prohormones. These prohormones are then cut into active hormones and peptide pieces, which are all secreted together. Because of their hydrophilic (water loving) nature, peptide hormones travel freely in the blood as they dissolve. They experience short half lives and tend to bind to surface cell receptors to initiate quick cellular responses. Peptide hormones can cause the synthesis of new proteins. | ||
Steroid hormones, on the other hand, are made on demand. Because they are derived from cholesterol, they are hydrophobic (water fearing) and tend to travel in the blood with protein carriers. Consequently, they have a longer half life. Receptors for steroid hormones are traditionally found inside the target cell. Responses include the turning on and off of genes and the direct synthesis of fresh proteins. Overall, the cell responses with steroid hormones are slower than those with peptide hormones. | Steroid hormones, on the other hand, are made on demand. Because they are derived from cholesterol, they are hydrophobic (water fearing) and tend to travel in the blood with protein carriers. Consequently, they have a longer half life. Receptors for steroid hormones are traditionally found inside the target cell. Responses include the turning on and off of genes and the direct synthesis of fresh proteins. Overall, the cell responses with steroid hormones are slower than those with peptide hormones. | ||
| + | |||
| + | ===By rate of synthesis=== | ||
| + | Orgs must be able to respond instantly to many changes in their internal or external environment; such rapid responses are mediated primarily by peptide hormones and catecholamines; signaling cells that produce them store them in secretory vesicles just under the plasma membrane; all peptide hormones, including insulin, are synthesized as part of a longer propolypeptide, which is cleaved (def) by specific enzymes to generate the active molecule just after it is transported to a secretory vesicle. Peptide hormones mediate short responses that are terminated by their own degradation. | ||
| + | |||
| + | In contrast, steroid-producing cells, like those in the adrenal cortex, store a small supply of hormone precursor; when stim’d, converted to active hormone, which then diffuses across the cell membrane into the blood (thyroxine has a diff type of storage cell. Because cells store little of the active hormone, release takes from hours to days; transported by carrier proteins, and are not rapidly degraded; thus, responses to thyroxine and steroid hormones take awhile to occur but effects last much longer (hrs to days). | ||
| + | |||
| + | ===By feedback control=== | ||
| + | feedback control of hormone levels: feedback circuits, in which changes in the level of one hormone affects the levels of other hormones (esp important in coordinating the complex processes of cell growth and differentiation); ex of estrogen and progesterone? | ||
==Hormone effects== | ==Hormone effects== | ||
| Line 102: | Line 140: | ||
*[http://www.plant-hormones.info/ Excellent plant hormone site on the Web.] | *[http://www.plant-hormones.info/ Excellent plant hormone site on the Web.] | ||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
| − | |||
==Pharmacology and cell bio research== | ==Pharmacology and cell bio research== | ||
Revision as of 17:51, 13 June 2007
Hormone effects vary widely, but can include:
- stimulation or inhibition of growth,
- induction or suppression of apoptosis (programmed cell death)
- activation or inhibition of the immune system
- regulating metabolism
- preparation for a new activity (e.g., fighting, fleeing, mating)
- preparation for a new phase of life (e.g., puberty, caring for offspring, menopause)
- controlling the reproductive cycle
In many cases, one hormone may regulate the production and release of other hormones
Many of the responses to hormone signals can be described as serving to regulate metabolic activity of an organ or tissue.
Hormonal signaling across this hierarchy involves the following:
- Biosynthesis of a particular hormone in a particular tissue.
- Storage and secretion of the hormone.
- Transport of the hormone to the target cell(s).
- Recognition of the hormone by an associated cell membrane or intracellular receptor protein.
- Relay and amplification of the received hormonal signal via a signal transduction process. This then leads to a cellular response. The reaction of the target cells may then be recognized by the original hormone-producing cells, leading to a down-regulation in hormone production. This is an example of a homeostatic negative feedback loop.
- Degradation of the hormone.
As can be inferred from the hierarchical diagram, hormone biosynthetic cells are typically of a specialized cell type, residing within a particular endocrine gland (e.g. the thyroid gland, ovaries or testes). Hormones may exit their cell of origin via exocytosis or another means of membrane transport.
Types of signalling
In animals, there are three types of signaling by extracellular, secreted molecules—endocrine, paracrine, or autocrine—based on the distance over which the signal acts.
Hormones belong to the first type: they act on target cells distant from their site of synthesis by cells of the endocrine organs. In animals, an endocrine hormone is usually carried by the blood from its site of release to the target cell.
Paracrine signaling molecules only affect target cells in close proximity (an example is the conduction of an impulse), while autocrine cells respond to substances that they themselves release.
However, the designations above are not so clear cut, as some compounds can act in two or even three types of signaling. For example, certain small peptides function both as neurotransmitters (paracrine signaling) and as hormones (endocrine signaling) that operate over longer distances. These neurohormones – definition TK.
A neurohormone is any hormone produced by neurosecretory cells, usually in the brain. Neurohormonal activity is distinguished from that of classical neurotransmitters as it can have effects on cells distant from the source of the hormone.
Neuroendocrine cells are a specialized group of nerve cells (neurons) that produce hormones. These hormones may be amines, neuropeptides, or specialized amino acids. They package the hormones in vesicles and send these packages via long processes (axons) to blood vessels. When stimulated (by hormones from the blood stream or other neurons) the neuroendocrine cells secrete the hormones into the blood stream. The hormones then travel to their target cells and may stimulate, inhibit or maintain function of these cells. The target cells may feed back information to these neurons that regulates further secretion.
Specialized groups of neuroendocrine cells can be found at the base of the third ventricle in the brain (in a region called the hypothalamus). This area controls most anterior pituitary cells and thereby regulates functions in the entire body, like responses to stress, cold, sleep, and the reproductive system. The neurons send processes to a region connecting to the pituitary stalk and the hormones (called releasing or inhibiting hormones) are released into the blood stream. They are carried by portal vessels to the pituitary cells where they may stimulate, inhibit, or maintain the function of a particular cell type. Many of the projects in the neuroendocrine group focus on the regulatory circuitry in this pathway.
The endocrine system works in close relation with the nervous system. It links the brain to the organs that control various aspects of the body. In addition, neurohormones are released by specialized groups of neurons in the brain. These function similarly to hormones and are often categorized into three major groups: catecholamines; hypothalamic neurohormones that monitor hormone release from the anterior pituitary; and hypothalamic neurohormones that monitor hormone release from the posterior pituitary. Neuroendocrinology is an area of medicine that focuses on the overlapping fields between the nervous and endocrine systems.
Overview
what goes here?
Communication usually involves six steps 1. synthesis 2. release of the sig mol by the sig cell 3. transport to target cell 4. detection of signal by a specific receptor protein 5. change in cellular metabolism or gene expression triggered by receptor-signaling complex 6. removal of the signal, often terminating the cellular response
Hormones in action
detail mechanisms
technical term for the signaling molecule (whether a hormone, neurotransmitter, or what have you) is ‘’ligand,’’ which binds to, or “fits” a site on the receptor protein, which is located on the surface of a target cell or in its nucleus or cytosol; binding causes a conformational change that initiates a sequence of reactions leading to a change in cellular function
diff cells respond differently to the same ligand, and diff receptor-ligand complexes can induce the same response in some cell types (ex of glucagons and epinephrine in liver cells, p 856)
a word on role of second messengers (intracellular signaling molecules)
Classification
Most hormones initiate a cellular response by initially combining with either a specific intracellular or cell membrane associated receptor protein. A cell may have several different receptors that recognize the same hormone and activate different signal transduction pathways, or alternatively different hormones and their receptors may invoke the same biochemical pathway.
For many hormones, including most protein hormones, the receptor is membrane associated and embedded in the plasma membrane at the surface of the cell. The interaction of hormone and receptor typically triggers a cascade of secondary effects within the cytoplasm of the cell, often involving phosphorylation or dephosphorylation of various other cytoplasmic proteins, changes in ion channel permeability, or increased concentrations of intracellular molecules that may act as secondary messengers (e.g. cyclic AMP). Some protein hormones also interact with intracellular receptors located in the cytoplasm or nucleus by an intracrine mechanism.
For hormones such as steroid or thyroid hormones, their receptors are located intracellularly within the cytoplasm of their target cell. In order to bind their receptors these hormones must cross the cell membrane. The combined hormone-receptor complex then moves across the nuclear membrane into the nucleus of the cell, where it binds to specific DNA sequences, effectively amplifying or suppressing the action of certain genes, and affecting protein synthesis.[1] However, it has been shown that not all steriod receptors are located intracellularly, some are plasma membrane associated.[2]
Vertebrate hormones fall into three chemical classes:
- Amine-derived hormones are derivatives of the amino acids tyrosine and tryptophan. Examples are catecholamines and thyroxine.
- Peptide hormones consist of chains of amino acids. Examples of small peptide hormones are TRH and vasopressin. Peptides composed of scores or hundreds of amino acids are referred to as proteins. Examples of protein hormones include insulin and growth hormone. More complex protein hormones bear carbohydrate side chains and are called glycoprotein hormones. Luteinizing hormone, follicle-stimulating hormone and thyroid-stimulating hormone are glycoprotein hormones.
- Lipid and phospholipid-derived hormones derive from lipids such as linoleic acid and arachidonic acid and phospholipids. The main classes are the steroid hormones that derive from cholesterol and the eicosanoids. Examples of steroid hormones are testosterone and cortisol. Sterol hormones such as calcitriol are a homologous system. The adrenal cortex and the gonads are primary sources of steroid hormones. Examples of eicosanoids are the widely studied prostaglandins.
An important consideration, dictating the level at which cellular signal transduction pathways are activated in response to a hormonal signal is the effective concentration of hormone-receptor complexes that are formed. Hormone-receptor complex concentrations are effectively determined by three factors:
- The number of hormone molecules available for complex formation
- The number of receptor molecules available for complex formation and
- The binding affinity between hormone and receptor.
The number of hormone molecules available for complex formation is usually the key factor in determining the level at which signal transduction pathways are activated. The number of hormone molecules available being determined by the concentration of circulating hormone, which is in turn influenced by the level and rate at which they are secreted by biosynthetic cells. The number of receptors at the cell surface of the receiving cell can also be varied as can the affinity between the hormone and its receptor.
Regulation
Hormonal regulation of some physiological activities involves a hierarchy of cell types acting on each other either to stimulate or modulate the release and action of a particular hormone. The secretion of hormones from successive levels of endocrine cells is stimulated by chemical signals originating from cells higher up the hierarchical system. The master coordinator of hormonal activity in mammals is the hypothalamus acting on input it receives from the central nervous system.
Other hormone secretion occurs in response to local conditions, such as the rate of secretion of parathyroid hormone by the parathyroid cells in response to fluctuations of ionized calcium levels in extracellular fluid.
However, the hierarchical model is an over simplification of the hormonal signaling process. Typically cellular recipients of a particular hormonal signal may be one of several cell types that reside within a number of different tissues, as is the case for insulin, which triggers a diverse range of systemic physiological effects. Different tissue types may also respond differently to the same hormonal signal. Because of this, hormonal signaling is elaborate and hard to dissect.
Most cells are capable of producing one or more molecules, which act as signaling molecules to other cells, altering their growth, function, or metabolism. The classical hormones produced by endocrine glands mentioned so far in this article are cellular products, specialized to serve as regulators at the overall organism level. However, they may also exert their effects solely within the tissue in which they are produced and originally released.
The rate of hormone biosynthesis and secretion is often regulated by a homeostatic negative feedback control mechanism. Such a mechanism depends on factors which influence the metabolism and excretion of hormones. Thus, higher hormome concentration alone cannot trigger the negative feedback mechanism. Negative feedback must be triggered by overproduction of an "effect" of the hormone.
Hormone secretion can be stimulated and inhibited by:
- Other hormones (stimulating- or releasing-hormones)
- Plasma concentrations of ions or nutrients, as well as binding globulins
- Neurons and mental activity
- Environmental changes, e.g., of light or temperature
In order to release active hormones quickly into the circulation, hormone biosynthetic cells may produce and store biologically inactive hormones in the form of pre- or prohormones. These can then be quickly converted into their active hormone form in response to a particular stimulus.
After a hormone has been secreted and has exerted its effect, its action must be terminated. This is accomplished by enzymes, which degrade, or breakdown, the hormone into metabolites. The metabolites are excreted along with bile and/or urine. Enzymes may be present in the blood or within the cell itself. Endocytosis of the receptor-hormone complex can also terminate hormone action. As noted above, the rate at which a hormone is broken down in the bloodstream is called the half life of the hormone. It is the amount of time needed to reduce the hormone concentration by one-half. This rate gives a measure of the period of time a hormone is active in the body. The endocrine system regulates hormone release and concentration through the negative feedback loop. Increases in hormone activity decrease the production and secretion of that hormone. Similarly, a decrease in activity of a hormone prompts an increase in the production and release of that hormone. The immune system as well as other factors contribute as control factors of hormone secretion. Together, these various mechanisms of control regulate the levels of hormones within the body.
Peptide hormones are made and stored in vesicles within cells until they receive a signal for secretion. Initially, peptide hormones are made as preprohormones, which are inactive, and then are converted into prohormones. These prohormones are then cut into active hormones and peptide pieces, which are all secreted together. Because of their hydrophilic (water loving) nature, peptide hormones travel freely in the blood as they dissolve. They experience short half lives and tend to bind to surface cell receptors to initiate quick cellular responses. Peptide hormones can cause the synthesis of new proteins. Steroid hormones, on the other hand, are made on demand. Because they are derived from cholesterol, they are hydrophobic (water fearing) and tend to travel in the blood with protein carriers. Consequently, they have a longer half life. Receptors for steroid hormones are traditionally found inside the target cell. Responses include the turning on and off of genes and the direct synthesis of fresh proteins. Overall, the cell responses with steroid hormones are slower than those with peptide hormones.
By rate of synthesis
Orgs must be able to respond instantly to many changes in their internal or external environment; such rapid responses are mediated primarily by peptide hormones and catecholamines; signaling cells that produce them store them in secretory vesicles just under the plasma membrane; all peptide hormones, including insulin, are synthesized as part of a longer propolypeptide, which is cleaved (def) by specific enzymes to generate the active molecule just after it is transported to a secretory vesicle. Peptide hormones mediate short responses that are terminated by their own degradation.
In contrast, steroid-producing cells, like those in the adrenal cortex, store a small supply of hormone precursor; when stim’d, converted to active hormone, which then diffuses across the cell membrane into the blood (thyroxine has a diff type of storage cell. Because cells store little of the active hormone, release takes from hours to days; transported by carrier proteins, and are not rapidly degraded; thus, responses to thyroxine and steroid hormones take awhile to occur but effects last much longer (hrs to days).
By feedback control
feedback control of hormone levels: feedback circuits, in which changes in the level of one hormone affects the levels of other hormones (esp important in coordinating the complex processes of cell growth and differentiation); ex of estrogen and progesterone?
Hormone effects
One special group of hormones is the trophic hormones that stimulate the hormone production of other endocrine glands. For example, thyroid-stimulating hormone (TSH) causes growth and increased activity of another endocrine gland, the thyroid, which increases output of thyroid hormones.
A recently-identified class of hormones is that of the "hunger hormones" - ghrelin, orexin and PYY 3-36 - and "satiety hormones" - e.g., leptin, obestatin, nesfatin-1.
Plant hormones
Plant hormones (or plant growth regulators, or PGRs) are internally-secreted chemicals in plants that are used for regulating the plants' growth. According to a standard definition, plant hormones are signal molecules produced at specific locations, that occur in very low concentrations, and cause altered processes in target cells at other locations.
It is accepted that there are five major classes of plant hormones:
Non-traditional plant hormones include
- salicylic acid
- jasmonates
- oligosaccharins
- brassinolides
- small extracellular signalling peptides
Pharmacology and cell bio research
Many hormones and their analogues are used as medication. The most commonly-prescribed hormones are estrogens and progestagens (as methods of hormonal contraception and as HRT), thyroxine (as levothyroxine, for hypothyroidism) and steroids (for autoimmune diseases and several respiratory disorders). Insulin is used by many diabetics. Local preparations for use in otolaryngology often contain pharmacologic equivalents of adrenaline, while steroid and vitamin D creams are used extensively in dermatological practice.
A "pharmacologic dose" of a hormone is a medical usage referring to an amount of a hormone far greater than naturally occurs in a healthy body. The effects of pharmacologic doses of hormones may be different from responses to naturally occurring amounts and may be therapeutically useful. An example is the ability of pharmacologic doses of glucocorticoid to suppress inflammation.
Important human hormones
[retain table?] Spelling is not uniform for many hormones. For example, current North American and international usage is estrogen, gonadotropin, while British usage retains the Greek diphthong in oestrogen and the unvoiced aspirant h in gonadotrophin.
| Structure | Name | Abbreviation | Tissue | Cells | Mechanism |
| amine - tryptophan | Melatonin (N-acetyl-5-methoxytryptamine) | pineal gland | pinealocyte | ||
| amine - tryptophan | Serotonin | 5-HT | CNS, GI tract | enterochromaffin cell | |
| amine - tyrosine | Thyroxine (thyroid hormone) | T4 | thyroid gland | thyroid epithelial cell | direct |
| amine - tyrosine | Triiodothyronine (thyroid hormone) | T3 | thyroid gland | thyroid epithelial cell | direct |
| amine - tyrosine (cat) | Epinephrine (or adrenaline) | EPI | adrenal medulla | chromaffin cell | |
| amine - tyrosine (cat) | Norepinephrine (or noradrenaline) | NRE | adrenal medulla | chromaffin cell | |
| amine - tyrosine (cat) | Dopamine | DPM | hypothalamus | ||
| peptide | Antimullerian hormone (or mullerian inhibiting factor or hormone) | AMH | testes | Sertoli cell | |
| peptide | Adiponectin | Acrp30 | adipose tissue | ||
| peptide | Adrenocorticotropic hormone (or corticotropin) | ACTH | anterior pituitary | corticotrope | cAMP |
| peptide | Angiotensinogen and angiotensin | AGT | liver | IP3 | |
| peptide | Antidiuretic hormone (or vasopressin, arginine vasopressin) | ADH | posterior pituitary | varies | |
| peptide | Atrial-natriuretic peptide (or atriopeptin) | ANP | heart | cGMP | |
| peptide | Calcitonin | CT | thyroid gland | parafollicular cell | cAMP |
| peptide | Cholecystokinin | CCK | duodenum | ||
| peptide | Corticotropin-releasing hormone | CRH | hypothalamus | cAMP | |
| peptide | Erythropoietin | EPO | kidney | ||
| peptide | Follicle-stimulating hormone | FSH | anterior pituitary | gonadotrope | cAMP |
| peptide | Gastrin | GRP | stomach, duodenum | G cell | |
| peptide | Ghrelin | stomach | P/D1 cell | ||
| peptide | Glucagon | GCG | pancreas | alpha cells | cAMP |
| peptide | Gonadotropin-releasing hormone | GnRH | hypothalamus | IP3 | |
| peptide | Growth hormone-releasing hormone | GHRH | hypothalamus | IP3 | |
| peptide | Human chorionic gonadotropin | hCG | placenta | syncytiotrophoblast cells | cAMP |
| peptide | Human placental lactogen | HPL | placenta | ||
| peptide | Growth hormone | GH or hGH | anterior pituitary | somatotropes | |
| peptide | Inhibin | testes | Sertoli cells | ||
| peptide | Insulin | INS | pancreas | beta cells | tyrosine kinase |
| peptide | Insulin-like growth factor (or somatomedin) | IGF | liver | tyrosine kinase | |
| peptide | Leptin | LEP | adipose tissue | ||
| peptide | Luteinizing hormone | LH | anterior pituitary | gonadotropes | cAMP |
| peptide | Melanocyte stimulating hormone | MSH or α-MSH | anterior pituitary/pars intermedia | cAMP | |
| peptide | Oxytocin | OXT | posterior pituitary | IP3 | |
| peptide | Parathyroid hormone | PTH | parathyroid gland | parathyroid chief cell | cAMP |
| peptide | Prolactin | PRL | anterior pituitary | lactotrophs | |
| peptide | Relaxin | RLN | varies | ||
| peptide | Secretin | SCT | duodenum | S cell | |
| peptide | Somatostatin | SRIF | hypothalamus, islets of Langerhans | delta cells | |
| peptide | Thrombopoietin | TPO | liver, kidney | ||
| peptide | Thyroid-stimulating hormone | TSH | anterior pituitary | thyrotropes | cAMP |
| peptide | Thyrotropin-releasing hormone | TRH | hypothalamus | IP3 | |
| steroid - glu. | Cortisol | adrenal cortex (zona fasciculata) | direct | ||
| steroid - min. | Aldosterone | adrenal cortex (zona glomerulosa) | direct | ||
| steroid - sex (and) | Testosterone | testes | Leydig cells | direct | |
| steroid - sex (and) | Dehydroepiandrosterone | DHEA | multiple | direct | |
| steroid - sex (and) | Androstenedione | adrenal glands, gonads | direct | ||
| steroid - sex (and) | Dihydrotestosterone | DHT | multiple | direct | |
| steroid - sex (est) | Estradiol | E2 | ovary | granulosa cells | direct |
| steroid - sex (est) | Estrone | ovary | granulosa cells | direct | |
| steroid - sex (est) | Estriol | placenta | syncytiotrophoblast | direct | |
| steroid - sex (pro) | Progesterone | ovary, adrenal glands, placenta | granulosa cells | direct | |
| sterol | Calcitriol (Vitamin D3) | skin/proximal tubule of kidneys | direct | ||
| eicosanoid | Prostaglandins | PG | seminal vesicle | ||
| eicosanoid | Leukotrienes | LT | white blood cells | ||
| eicosanoid | Prostacyclin | PGI2 | endothelium | ||
| eicosanoid | Thromboxane | TXA2 | platelets |
ReferencesISBN links support NWE through referral fees
- Beato, M., Chavez, S., and M. Truss. 1996. Transcriptional regulation by steroid hormones. Steroids 61(4): 240-251. PMID 8733009
- Cooper, G. M., and R. E. Hausman. 2004. The Cell: A Molecular Approach, 3rd edition. Washington, D.C.: ASM Press & Sunderland, M.A.: Sinauer Associates. ISBN 0878932143
- Hammes, S.R. 2003. The further redefining of steroid-mediated signaling. Proc Natl Acad Sci 100(5): 2168-70 PMID 12606724
- Lodish, H., D. Baltimore, A. Berk, S. L. Zipursky, P. Matsudaira, and J. Darnell. 1995. Molecular Cell Biology, 3rd edition. New York, NY: Scientific American Books. ISBN 0716723808.
- Mathews, C.K. and K.E. van Holde. 1990. Biochemistry. San Francisco: Benjamin-Cummings. ISBN 0805350152
- Stryer, L. 1995. Biochemistry, 4th edition. New York: W.H. Freeman. ISBN 0716720094
See also
- Endocrinology
- Endocrine system
- Neuroendocrinology
- Plant hormones or plant growth regulators
- Autocrine signaling
- Paracrine signaling
- Intracrine
- Cytokine
- Growth factor
- Hormone disruptor
External links
- MeSH Hormones
| Hormones and endocrine glands - edit |
|---|
|
Hypothalamus: GnRH - TRH - CRH - GHRH - somatostatin - dopamine | Posterior pituitary: vasopressin - oxytocin | Anterior pituitary: GH - ACTH - TSH - LH - FSH - prolactin - MSH - endorphins - lipotropin Thyroid: T3 and T4 - calcitonin | Parathyroid: PTH | Adrenal medulla: epinephrine - norepinephrine | Adrenal cortex: aldosterone - cortisol - DHEA | Pancreas: glucagon- insulin - somatostatin | Ovary: estradiol - progesterone - inhibin - activin | Testis: testosterone - AMH - inhibin | Pineal gland: melatonin | Kidney: renin - EPO - calcitriol - prostaglandin | Heart atrium: ANP Stomach: gastrin | Duodenum: CCK - GIP - secretin - motilin - VIP | Ileum: enteroglucagon | Liver: IGF-1 Placenta: hCG - HPL - estrogen - progesterone Adipose tissue: leptin, adiponectin Target-derived NGF, BDNF, NT-3 |
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.