Cancer
| Cancer | |
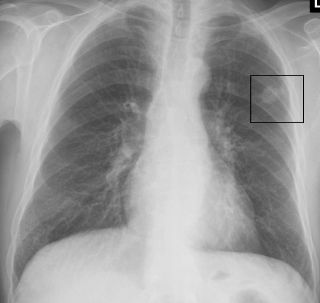 Chest x-ray showing lung cancer in the left lung. | |
| DiseasesDB | 28843 |
|---|---|
| MedlinePlus | 001289 |
| MeSH | D009369 |
Cancer, or "malignant neoplasm," is a large category of almost one hundred diseases, characterized by uncontrolled growth of cells and the ability of these abnormally dividing cells to spread from the original site, whether to adjacent tissues or, in some cases, even to distant sites in the body. Known as "a disease of the genes," some cancers have an hereditary basis whereby an individual inherits faulty DNA from his or her parents, perhaps due to an error in replication of the DNA. However, most types of cancers originate from changes to a cell's DNA (mutations) due to environmental factors (carcinogens), such as tobacco smoke, UV radiation, chemicals, or infectious agents.
If the spread of cancer is not controlled, it can result in death, and cancer is one of the leading causes of death worldwide. The risk of cancer increases with age, with most cases occurring in people older than 65 years of age. Among well-known cancers are skin cancer, breast cancer (in women), prostate cancer (in men), colon cancer, and lung cancer. The branch of medicine concerned with the study, diagnosis, treatment, and prevention of cancer is oncology.
The terms cancer and tumor are not synonymous. In modern medicine, the term cancer is interchangeable with the term malignant neoplasm. A neoplasm is an abnormal overgrowth of cells; a tumor is a neoplasm that has formed a lump. However, neoplasms and tumors may be benign or they may be malignant. A benign tumor or benign neoplasm does not spread or migrate to surrounding tissues; thus, it is not considered cancer. The malignant versions do involve the invasion of surrounding tissues and perhaps the spreading to other parts of the body; thus, a malignant tumor or malignant neoplasm is cancer. Some cancers, however, do not form a tumor, such as leukemia.
The development of abnormalities in the genetic material of a dividing cell is not uncommon, but a healthy immune system can generally recognize the neoplastic cells and destroy them before they proliferate. This fact, and the reality that many cancers are predominately caused by environmental rather than hereditary factors, suggests a component of personal and social responsibility in the control of cancer. On a personal basis, in addition to behaviors supporting a healthy immune system, various risky behaviors can be avoided, such as smoking, excessive consumption of alcohol, excessive exposure to UV radiation, excessive intake of dietary fat, and risky sexual practices. On a social level, identification and removal of carcinogens from the environment, such as harmful chemicals from pollution or exposure to occupational hazards such as asbestos, is important. More than 30 percent of cancer is preventable via avoiding such risk factors as tobacco, alcohol, overweight or obesity, low fruit and vegetable intake, physical inactivity, sexually transmitted infections, and air pollution.
Overview
A disease of the genes
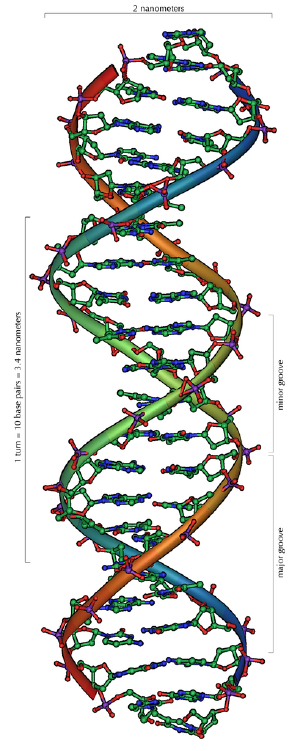
By definition, cancer is a disease of the genes.[1] A gene is the unit of inheritance in living organisms. A gene is essentially a region of DNA that cells transcribe into RNA, which can then be translated to produce proteins. In molecular biology, a gene is considered to comprise both a coding sequence—that region of the DNA that determines the structure of a protein—and any regulatory sequence—that region of the DNA that controls when and where the protein will be produced.
During cell division, the cell makes a copy of the DNA. In eukaryotes, cells undergo a particular process during cell division, known as mitosis, in which the DNA is replicated and then separated so that the mother and daughter cells have (ideally) identical copies of the original DNA. If the parent cell is diploid (two sets of chromosomes), the daughter cells are diploid. Meiosis, on the other hand, produces daughter cells (germ cells) with just half of the chromosomes; that is, in diploid organisms, the germ cells (eggs and sperm) that are produced are haploid (one complete set of chromosomes).
Sometimes, mutations occur in the genetic material, whereby there is a change in the base pair sequence of the DNA. For example, during DNA replication during mitosis, an incorrect or damaged base may be placed into the DNA, such as a thymine rather than adenine, or perhaps UV light causes a thymine dimer whereby adjacent thymine bases form a covalent linkage rather than the thymine bases link to the adenine bases on the opposite strand of DNA. There are many mechanisms to repair damaged DNA. Other errors can occur in mitosis or in meiosis that lead to faulty DNA material in daughter cells, such as non-disjunction of chromosomes or part of a chromosome attaching to another chromosome during separation.
Cancers essentially are caused by abnormalities in the genetic material of the transformed cells leading to uncontrolled cell growth and invasion of other tissues.[2] These abnormalities may be due to the effects of carcinogens, such as tobacco smoke, radiation, chemicals, or infectious agents. Some cancer-promoting genetic abnormalities are inherited, and thus present in all cells from birth, having occurred through errors in DNA replication. The heritability of cancers is usually affected by complex interactions between carcinogens and the host's genome.
Less than ten percent of all cancers are considered to purely hereditary. Those with an hereditary link include breast cancer, colon cancer, uterine cancer, and ovarian cancer. However, there also are physiological traits that could be inherited that contribute to cancer, since those inheriting fair skin are more predisposed to developing skin cancer, although only if exposed to intensive sunlight.[1]
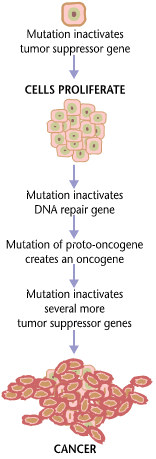
Genetic abnormalities found in cancer typically affect two general classes of genes. Cancer-promoting oncogenes are typically activated in cancer cells, giving those cells new properties, such as hyperactive growth and division, protection against programmed cell death, loss of respect for normal tissue boundaries, and the ability to become established in diverse tissue environments. Tumor suppressor genes are then inactivated in cancer cells, resulting in the loss of normal functions in those cells, such as accurate DNA replication, control over the cell cycle, orientation and adhesion within tissues, and interaction with protective cells of the immune system.
Three properties of cancer
Cancer is a class of diseases in which a group of cells display uncontrolled growth (division beyond the normal limits), invasion (intrusion on and destruction of adjacent tissues), and sometimes metastasis (spread to other locations in the body via lymph or blood).
Cancer has been called "a disease of cell division—a failure of cell division control."[3] Cancerous cells undergo uncontrolled cell division.
For example, the p53 protein, produced by the gene dubbed p53, monitors the integrity of DNA during cell division. If the DNA is damaged, then p53 halts cell division until the DNA can be repaired by special enzymes, or, if the damage is not repairable, it directs the cell to kill itself. If the damage is repaired, the cell division is allowed to continue. However, if the p53 gene is nonfunctional (damaged or missing entirely), such as from a mutation, then cancerous cells are allowed to repeatedly undergo cell division without being halted.[3]
Cancers, tumors, and neoplasms
The three properties of cancers (uncontrolled growth, invasion, and metastasis) differentiate them from benign tumors and benign neoplasms.
Neoplasm is a medical term that refers to a new growth of cells. Whereas "neo" means new and "plasm" refers to cells, the word neoplasm refers to an abnormal overgrowth of cells rather than healthy new cell growth. Neoplasm is an abnormal mass of tissue as a result of neoplasia (the abnormal proliferation of cells). The growth of the cells exceeds, and is uncoordinated with that of the normal tissues around it. The growth persists in the same excessive manner even after cessation of the stimuli. It usually causes a lump or tumor.
Neoplasm is often used interchangeably with words such as tumor and cancer. However, neoplasms may be benign, pre-malignant or malignant. Likewise, tumors—a neoplasm that has formed a lump—may be benign, pre-malignant, or malignant. Cancer, whether forming or tumor or not, is malignant. Cancer involves both "uncontrolled growth" and "invasion," and sometimes "metastasis," whereas a benign neoplasm or benign tumor is self-limited, and does not invade or metastasize. Furthermore, the removal of a benign tumor usually prevents the re-occurrence of the condition, whereas if the cancer has spread to surrounding tissues, the removal of a malignant tumor does not prevent the re-occurrence of the cancer.[1] The main use of the term neoplasm is in medical statistics that categorize deaths or other events, in which case neoplasm is typically the category that includes cancer statistics.
Prevalence and diagnosis
Cancer affects people at all ages, with the risk for most types increasing with age. Cancer is the second leading cause of death globally, and was responsible for 8.8 million deaths in 2015.[4] In the United States, more than 500,000 die annually, with about 1.2 million diagnosed with the disease; the most common deaths are from lung cancer (160,000 per year), followed by colon and rectum cancer (56,500), breast cancer (43,900), and prostate cancer (39,200).[1]
Definitive diagnosis requires the histologic examination of a biopsy specimen, although the initial indication of malignancy can be symptomatic or radiographic imaging abnormalities. Most cancers can be treated and some forced into remission, depending on the specific type, location, and stage. Once diagnosed, cancer is usually treated with a combination of surgery, chemotherapy, and radiotherapy. As research develops, treatments are becoming more specific for different varieties of cancer. There has been significant progress in the development of targeted therapy drugs that act specifically on detectable molecular abnormalities in certain tumors, and which minimize damage to normal cells. The prognosis of cancer patients is most influenced by the type of cancer, as well as the stage, or extent of the disease. In addition, histologic grading and the presence of specific molecular markers can also be useful in establishing prognosis, as well as in determining individual treatments.
Classification
Cancers are classified according to the tissue presumed to be the origin of the tumor, based on the resemblance of the tumorous cells to the normal cells in the tissue and the location. Examples of general categories include:
- Carcinoma: Malignant tumors derived from epithelial cells. The epithelium is the tissue that covers internal organs and various glands, as well as the surfaces of the bodies of animals, including both outside surfaces (the skin) and inside cavities and lumen. This group represents the most common cancers, including the common forms of breast, prostate, lung and colon cancer. This category encompasses ninety percent of all cancers. These can be further divided into:[1]
- Adenocarcinomas: cancers that develop in an organ or gland; and
- Squamous cell carcinomas: Cancers that originate in the skin.
- Sarcoma: Malignant tumors derived from connective tissue, or mesenchymal cells (such as bone, muscle, and blood vessels).
- Lymphoma and leukemia: Malignancies derived from hematopoietic (blood-forming) cells (cancers of the lymph glands and blood, respectively).
- Germ cell tumor: Tumors derived from totipotent cells. In adults, these are most often found in the testicle and ovary; in fetuses, babies, and young children, these are most often found on the body midline, particularly at the tip of the tailbone; in horses most often found at the poll (base of the skull).
- Blastic tumor or blastoma: A tumor (usually malignant) which resembles an immature or embryonic tissue. Many of these tumors are most common in children.
- Melanoma:Like squamous cell carcinomas, these also originate in the skin, usually in the melanocytes (pigment cells).
- Glioma: Cancer of the nerve tissue.
Malignant tumors (cancers) are usually named using -carcinoma, -sarcoma or -blastoma as a suffix, with the Latin or Greek word for the organ of origin as the root. For instance, a cancer of the liver is called hepatocarcinoma; a cancer of the fat cells is called liposarcoma. For common cancers, the English organ name is used. For instance, the most common type of breast cancer is called ductal carcinoma of the breast or mammary ductal carcinoma. Here, the adjective ductal refers to the appearance of the cancer under the microscope, resembling normal breast ducts.
Benign tumors (which are not cancers) are named using -oma as a suffix with the organ name as the root. For instance, a benign tumor of the smooth muscle of the uterus is called leiomyoma (the common name of this frequent tumor is fibroid). Unfortunately, some cancers also use the -oma suffix, examples being melanoma and seminoma.
History

The oldest known description and surgical treatment of cancer can be found in the Edwin Smith Papyrus, a preserved medical document from ancient Egypt that traces to about the sixteenth to seventeenth century B.C.E. (but appears to be the only surviving copy of part of a much older treatise on trauma surgery from about 3000 to 2500 B.C.E.). This document, the world's oldest known surgical document, describes 8 cases of tumors or ulcers of the breast, which were treated by cauterization, with a tool called "the fire drill." The writing states, however, "There is no treatment."[5]
Hippocrates (ca. 460 B.C.E.–ca. 370 B.C.E.) described several kinds of cancers. He called benign tumors oncos, Greek for "swelling," and malignant tumors carcinos, Greek for "crab" or "crayfish." This later name comes from the appearance of the cut surface of a solid, malignant tumor, with "the veins stretched on all sides as the animal the crab has its feet, whence it derives its name".[6] Hippocrates later added the suffix -oma, Greek for "swelling," giving the name carcinoma.
Since it was against Greek tradition to open the body, Hippocrates only described and made drawings of outwardly visible tumors on the skin, nose, and breasts. Treatment was based on the humor theory of four bodily fluids (black and yellow bile, blood, and phlegm). According to the patient's humor, treatment consisted of diet, blood-letting, and/or laxatives. Through the centuries it was discovered that cancer could occur anywhere in the body, but humor-theory based treatment remained popular until the nineteenth century and the discovery of cells.
Today, the Greek term carcinoma is the medical term for a malignant tumor derived from epithelial cells. It is Celsus (ca 25 B.C.E.—ca 50) who translated carcinos into the Latin cancer, also meaning crab. Galen used "oncos" to describe all tumors, the root for the modern word oncology.[7]
Eleventh to Seventeenth centuries
In the 1020s, Avicenna (Ibn Sina) described a surgical treatment for cancer in The Canon of Medicine. He stated that the excision should be radical and that all diseased tissue should be removed, which included the use of amputation or the removal of veins running in the direction of the tumor. He also recommended the use of cauterization for the area treated if necessary.[8]
In the sixteenth and seventeenth centuries, it became more acceptable for doctors to dissect bodies to discover the cause of death. The German professor Wilhelm Fabry believed that breast cancer was caused by a milk clot in a mammary duct. The Dutch professor Francois de la Boe Sylvius, a follower of Descartes, believed that all disease was the outcome of chemical processes, and that acidic lymph fluid was the cause of cancer. His contemporary Nicolaes Tulp believed that cancer was a poison that slowly spreads, and concluded that it was contagious.[9]
Eighteenth and Nineteenth centuries
The first cause of cancer was identified by British surgeon Percivall Pott, who discovered in 1775 that cancer of the scrotum was a common disease among chimney sweeps.
With the widespread use of the microscope in the eighteenth century, it was discovered that the 'cancer poison' spread from the primary tumor through the lymph nodes to other sites ("metastasis"). This view of the disease was first formulated by the English surgeon Campbell De Morgan between 1871 and 1874.[10]
The use of surgery to treat cancer had poor results due to problems with hygiene. The renowned Scottish surgeon Alexander Monro saw only two breast tumor patients out of 60 surviving surgery for two years. In the nineteenth century, asepsis improved surgical hygiene and as the survival statistics went up, surgical removal of the tumor became the primary treatment for cancer. With the exception of William Coley, who in the late 1800s felt that the rate of cure after surgery had been higher before asepsis (and who injected [[bacteria] into tumors with mixed results), cancer treatment became dependent on the individual art of the surgeon at removing a tumor. During the same period, the idea that the body was made up of various tissues, that in turn were made up of millions of cells, laid rest the humor-theories about chemical imbalances in the body. The age of cellular pathology was born.
Modern era
The genetic basis of cancer was recognized in 1902 by the German zoologist Theodor Boveri, professor of zoology at Munich and later in Würzburg.[11] He discovered a method to generate cells with multiple copies of the centrosome, a structure he discovered and named. He postulated that chromosomes were distinct and transmitted different inheritance factors. He suggested that mutations of the chromosomes could generate a cell with unlimited growth potential which could be passed onto its descendants. He proposed the existence of cell cycle check points (points during mitosis when the cell pauses to check the replicated DNA or division process and can fix errors or keep the cell from dividing), tumor suppressor genes, and oncogenes. He speculated that cancers might be caused or promoted by radiation, physical or chemical insults, or by pathogenic microorganisms.
When Marie Curie (1867–1934) and Pierre Curie (1859–1906) advanced the study of radiation at the end of the nineteenth century and beginning of the twentieth century, they stumbled upon the first effective non-surgical cancer treatment, conducting the world's first studies into the treatment of neoplasms using radioactive isotopes.
With radiation also came the first signs of multi-disciplinary approaches to cancer treatment. The surgeon was no longer operating in isolation, but worked together with hospital radiologists to help patients. The complications in communication this brought, along with the necessity of the patient's treatment in a hospital facility rather than at home, also created a parallel process of compiling patient data into hospital files, which in turn led to the first statistical patient studies.
A founding paper of cancer epidemiology was the work of Janet Lane-Claypon, who published a comparative study in 1926 of 500 breast cancer cases and 500 control patients of the same background and lifestyle for the British Ministry of Health. Her ground-breaking work on cancer epidemiology was carried on by Richard Doll and Austin Bradford Hill, who published "Lung Cancer and Other Causes of Death In Relation to Smoking. A Second Report on the Mortality of British Doctors" followed in 1956 (otherwise known as the British doctors study). Richard Doll left the London Medical Research Center (MRC), to start the Oxford unit for cancer epidemiology in 1968. With the use of computers, the unit was the first to compile large amounts of cancer data. Modern epidemiological methods are closely linked to current concepts of disease and public health policy. Over the past 50 years, great efforts have been spent on gathering data across medical practice, hospital, provincial, state, and even country boundaries to study the interdependence of environmental and cultural factors on cancer incidence.
Cancer patient treatment and studies were restricted to individual physicians' practices until World War II, when medical research centers discovered that there were large international differences in disease incidence. This insight drove national public health bodies to make it possible to compile health data across practices and hospitals, a process that many countries do today. The Japanese medical community observed that the bone marrow of victims of the atomic bombings of Hiroshima and Nagasaki was completely destroyed. They concluded that diseased bone marrow could also be destroyed with radiation, and this led to the discovery of bone marrow transplants for leukemia. Since World War II, much research has been devoted to cancer research and treatment, including improvement and standardization of existing treatment methods and efforts to find cures through epidemiology and international partnerships.
Epidemiology
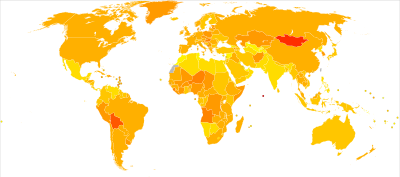
As noted above, about 13 percent (7.4 million) of all deaths worldwide in 2004 were attributed to cancer as a cause. In the United States, about one out of every four deaths is attributed to cancer, with only heart disease exceeding cancer as a cause of death.[1]
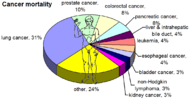
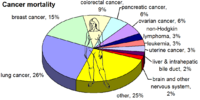
Lung cancer was the leading cause of death in the United States (160,100), followed by colon and rectum cancer (56,500), breast cancer (43,900), prostate cancer (39,200), pancreas cancer (28,900), lymphoma (26,300), and brain cancer (17,400), with stomach the ninth most frequent (13,700) and liver the 10th most frequent (13,000).[1]
Cancer can occur in children and adolescents, but it is uncommon (about 150 cases per million in the U.S.), with leukemia the most common.[12] In the first year of life, the incidence is about 230 cases per million in the United States, with the most common being neuroblastoma.[13]
In the United States, men have a lifetime risk of developing cancer of one in five, while women have a one in three lifetime risk. African-Americans are more likely to develop cancer and die of cancer than whites.[1]
In the developed world, one in three people will develop cancer during their lifetimes. If all cancer patients survived and cancer occurred randomly, the lifetime odds of developing an second primary cancer would be one in nine.[14] However, cancer survivors have an increased risk of developing a second primary cancer, and the odds are about two in nine. About half of these second primaries can be attributed to the normal one-in-nine risk associated with random chance. The increased risk is believed to be primarily due to the same risk factors that produced the first cancer, such as the person's genetic profile, alcohol and tobacco use, obesity, and environmental exposures, and partly due, to the treatment for the first cancer, which typically includes mutagenic chemotherapeutic drugs or radiation. Cancer survivors may also be more likely to comply with recommended screening, and thus may be more likely than average to detect cancers.[14]
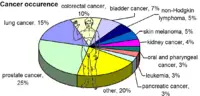
Most common cancers in males, by occurrence[12]
In females, by occurrence[12]
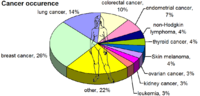
In males, by mortality[12]
In females, by mortality[12]
Causes and risk factors
Overview of causes
Cancer is a diverse class of diseases, which differ widely in their causes and biology. Any multicellular organism with diverse tissues, even plants, can acquire cancer. Nearly all known cancers arise gradually, as errors build up in the cancer cell and its progeny (see mechanisms section for common types of errors).
All living cells have the potential for their genetic material to suffer from mutations, as well as diverse other errors that can occur during replication, such as non-disjunction of chromosomes. Unless error recognition and correction is properly carried out, the errors will survive, and might be passed along to daughter cells, unless cell division is halted or the cell is terminated. Normally, the body safeguards against cancer via numerous methods. For example, there are checkpoints during mitosis when cell division is halted until any errors found are corrected, such as via repair of damaged DNA. A cell may undergo apoptosis (cell death) if errors cannot be repaired. However these error-correction methods often fail in small ways, especially in environments that make errors more likely to arise and propagate. For example, such environments can include the presence of disruptive substances called carcinogens, or periodic injury (physical, heat, etc.), or environments that cells did not evolve to withstand, such as hypoxia[15] (see subsections). Cancer is thus a progressive disease, and these progressive errors slowly accumulate until a cell begins to act contrary to its function in the organism.
The errors which cause cancer are often self-amplifying, eventually compounding at an exponential rate. For example:
- A mutation in the error-correcting machinery of a cell might cause that cell and its daughter cells to accumulate errors more rapidly
- A mutation in signaling (endocrine) machinery of the cell can send error-causing signals to nearby cells
- A mutation might cause cells to become neoplastic, causing them to migrate and disrupt more healthy cells
- A mutation may cause the cell to become immortal (see telomeres), causing them to disrupt healthy cells forever
Thus cancer often explodes in something akin to a chain reaction caused by a few errors, which compound into more severe errors. Errors that produce more errors are effectively the root cause of cancer, and also the reason that cancer is so hard to treat: even if there were 10,000,000,000 cancerous cells and one killed all but 10 of those cells, those cells (and other error-prone precancerous cells) could still self-replicate or send error-causing signals to other cells, starting the process over again. This rebellion-like scenario is an undesirable survival of the fittest, working against the body's design and enforcement of order. In fact, once cancer has begun to develop, this same force continues to drive the progression of cancer towards more invasive stages, and is called clonal evolution.[16]
Research about cancer causes often falls into the following categories:
- Agents (e.g. viruses) and events (e.g. mutations) that cause or facilitate genetic changes in cells destined to become cancer.
- The precise nature of the genetic damage, and the genes that are affected by it.
- The consequences of those genetic changes on the biology of the cell, both in generating the defining properties of a cancer cell, and in facilitating additional genetic events that lead to further progression of the cancer.
Pathophysiology
Cancer is fundamentally a disease of regulation of tissue growth. In order for a normal cell to transform into a cancer cell, gene that regulate cell growth and differentiation must be altered.[17] Genetic changes can occur at many levels, from gain or loss of entire chromosomes to a mutation affecting a single DNA nucleotide.
There are two broad categories of genes that are affected by these changes. Oncogenes may be normal genes that are expressed at inappropriately high levels, or altered genes that have novel properties. In either case, expression of these genes promotes the malignant phenotype of cancer cells. Tumor suppressor genes are genes that inhibit cell division, survival, or other properties of cancer cells. Tumor suppressor genes are often disabled by cancer-promoting genetic changes. Typically, changes in many genes are required to transform a normal cell into a cancer cell.[18]
There is a diverse classification scheme for the various genomic changes that may contribute to the generation of cancer cells. Most of these changes are mutations, or changes in the nucleotide sequence of genomic DNA. Aneuploidy, the presence of an abnormal number of chromosomes, is one genomic change that is not a mutation, and may involve either gain or loss of one or more chromosome through errors in mitosis.
Large-scale mutations involve the deletion or gain of a portion of a chromosome. Genomic amplification occurs when a cell gains many copies (often 20 or more) of a small chromosomal locus, usually containing one or more oncogenes and adjacent genetic material. Translocation occurs when two separate chromosomal regions become abnormally fused, often at a characteristic location. A well-known example of this is the Philadelphia chromosome, or translocation of chromosomes 9 and 22, which occurs in chronic myelogenous leukemia, and results in production of the BCR-abl fusion protein, an oncogenic tyrosine kinase.
Small-scale mutations include point mutations, deletions, and insertions, which may occur in the promoter of a gene and affect its expression, or may occur in the gene's coding sequence and alter the function or stability of its protein product. Disruption of a single gene may also result from integration of genomic material from a DNA virus or retrovirus, and such an event may also result in the expression of viral oncogenes in the affected cell and its descendants.
Risk factors
Greater than 30 percent of cancer is preventable via avoiding risk factors including: tobacco, overweight, or obesity, low fruit and vegetable intake, physical inactivity, alcohol, sexually transmitted infections, and air pollution.[4] The American Cancer Society estimates that approximately 40 percent of cancer deaths in 1998 were due to tobacco and excessive alcohol use and another one-third of deaths were related to diet and nutrition.[1]
Chemicals
- Further information: Carcinogen
Among chemicals traced to cancer are those related to personal behavior (tobacco, alcohol), occupational hazards (working with asbestos, dyes, rubber, gas, arsenic, gold mining, smelting, glue, varnish, PVC, uranium mining, radiology), and environmental sources (pollution, chlorination, asbestos).
Cancer pathogenesis is traceable back to DNA mutations that impact cell growth and metastasis. Substances that cause DNA mutations are known as mutagens, and mutagens that cause cancers are known as carcinogens. Particular substances have been linked to specific types of cancer.
While many mutagens are also carcinogens, some carcinogens are not mutagens. Alcohol is an example of a chemical carcinogen that is not a mutagen.[19] Such chemicals may promote cancers through stimulating the rate of cell division rather than mutation. Faster rates of replication leaves less time for repair enzymes to repair damaged DNA during DNA replication, increasing the likelihood of a mutation.
Tobacco. Tobacco smoking is associated with many forms of cancer,[20] and causes eighty to ninety percent of lung cancer cases.[21][1]
Smoking also has been linked, via decades of research, to cancers of the upper respiratory tract, larynx, head, neck, stomach, bladder, kidney, esophagus and pancreas.[22] Tobacco smoke contains over fifty known carcinogens, including nitrosamines and polycyclic aromatic hydrocarbons.[23] Tobacco is responsible for about one in three of all cancer deaths in the developed world,[20] and about one in five worldwide.[23] Indeed, lung cancer death rates in the United States have mirrored smoking patterns, with increases in smoking followed by dramatic increases in lung cancer death rates and decreases in smoking followed by decreases in lung cancer death rates in men. However, the numbers of smokers worldwide is still rising, leading to what some organizations have described as the tobacco epidemic.[24]
Asbestos. Prolonged exposure to asbestos fibers is associated with mesothelioma, a rare form of cancer that develops from the protective lining that covers many of the body's internal organs, the mesothelium, and in particular the outer lining of the lung and internal chest wall.[25] Most people who develop mesothelioma have worked on jobs where they inhaled asbestos particles, or they have been exposed to asbestos dust and fiber in other ways. Unlike lung cancer, there is no association between mesothelioma and smoking, but smoking greatly increases the risk of other asbestos-induced cancers.[26]
Alcohol. Excessive alcohol consumption is a risk factor in contracting liver cancer, and in combination with tobacco increases the likelihood of developing mouth, larynx, pharynx, and esophageal cancers.[1]
Other chemicals. Working with dye, rubber, and gas has been linked to a higher likelihood of getting cancer of the bladder, while lung and skin cancer is linked to smelters, gold mining, and working with arsenic. Glue and varnish workers have an increased incidence of leukemia; PVC manufacturing is linked to liver cancer; and uranium mining and radiology is linked to bone and bone marrow cancer, as well as lung cancer. Industrial waste pollution is linked to cancer and there may be a small increased risk of cancer form chlorination of water. Overall, about one percent of cancer deaths are estimated to be linked to air, water, and land pollution.[1]
Ionizing radiation
Sources of ionizing radiation, such as radon gas, x rays, and sunlight, can cause cancer, with about one to two percent of all cancer deaths linked to radiation. Prolonged exposure to ultraviolet radiation from the sun can lead to melanoma and other skin malignancies, with the majority of melanoma deaths linked to UV radiation.[27] It is estimated that 2 percent of future cancers will be due to current CT scans.[28] Ionizing radiation from nuclear material is another source of cancer.
Non-ionizing radio frequency radiation from mobile phones and other similar RF sources has also been proposed as a cause of cancer. However, research has not revealed a consistent link between cancer and cell phone use.[29][30]
Infection
Some cancers can be caused by infection, from viruses, bacteria, and parasites. This is especially true in animals such as birds, but also in humans, with viruses responsible for up to twenty percent of human cancers worldwide. These include human papillomavirus (cervical carcinoma), human polyomaviruses (mesothelioma, brain tumors), Epstein-Barr virus (B-cell lymphoproliferative disease and nasopharyngeal carcinoma), Kaposi's sarcoma herpesvirus (Kaposi's Sarcoma and primary effusion lymphomas), hepatitis B and hepatitis C viruses (hepatocellular carcinoma), Human T-cell leukemia virus-1 (T-cell leukemias), and Helicobacter pylori (gastric carcinoma).[31]
Experimental and epidemiological data imply a causative role for viruses and they appear to be the second most important risk factor for cancer development in humans, exceeded only by tobacco usage.[32] The mode of virally induced tumors can be divided into two, acutely transforming or slowly transforming. In acutely transforming viruses, the virus carries an overactive oncogene called viral-oncogene (v-onc), and the infected cell is transformed as soon as v-onc is expressed. In contrast, in slowly transforming viruses, the virus genome is inserted near a proto-oncogene in the host genome. The viral promoter or other transcription regulation elements then cause over expression of that proto-oncogene. This induces uncontrolled cell division. Because the site of insertion is not specific to proto-oncogenes, and the chance of insertion near any proto-oncogene is low, slowly transforming viruses will cause tumors much longer after infection than the acutely transforming viruses.
Hepatitis viruses, including hepatitis B and hepatitis C, can induce a chronic viral infection that leads to liver cancer in 0.47% of hepatitis B patients per year (especially in Asia, less so in North America), and in 1.4% of hepatitis C carriers per year. Liver cirrhosis, whether from chronic viral hepatitis infection or alcoholism, is associated with the development of liver cancer, and the combination of cirrhosis and viral hepatitis presents the highest risk of liver cancer development. Worldwide, liver cancer is one of the most common, and most deadly, cancers due to a huge burden of viral hepatitis transmission and disease.
Advances in cancer research have made a vaccine designed to prevent cancer available. In 2006, the U.S. Food and Drug Administration approved a human papilloma virus vaccine, called Gardasil. The vaccine protects against four HPV types, which together cause 70% of cervical cancers and 90% of genital warts. In March 2007, the US Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) officially recommended that females aged 11–12 receive the vaccine, and indicated that females as young as age 9 and as old as age 26 are also candidates for immunization.
In addition to viruses, researchers have noted a connection between bacteria and certain cancers. The most prominent example is the link between chronic infection of the wall of the stomach with Helicobacter pylori and gastric cancer.[33][34] Although only a minority of those infected with Helicobacter go on to develop cancer, since this pathogen is quite common it is probably responsible for most of these cancers.[35]
Sexual and reproductive behavior risk factors
Several sexual and reproductive behaviors correlated with increased risk of cancer.
The human papilloma virus, noted above as an infectious cause of cervical cancer, is sexually transmitted disease. There is increased likelihood of getting this disease when one has too many sexual partners and is sexually active at an early age.
There is evidence that men are more likely to develop prostate cancer if they are very sexually active in their twenties and thirties, particularly if they masturbate frequently, with the correlation particularly linked to the latter.[36] The same correlation study of 800 men also found higher incidences of prostate cancer among those with more sexual partners and sexually transmitted diseases, whereas there was decreased correlations with cancer among those sexually active in their fifties.[36][37] However, there are earlier studies that have presented contrasting results.[38]
There is an increased risk for both ovarian cancer and breast cancer among women who do not undergo childbirth or have children later in life.[1]
Dietary causes
There is a link between cancer and diet. The American Cancer Society reports that over one-third (35 percent) of all cancer deaths in the United States are related to diet and nutrition. The excessive consumption of fat, leading to obesity, is linked to cancers of the colon, rectum, pancreas, breast, prostate, ovaries, uterus, and gall bladder.[1]
Immune system dysfunction
HIV is associated with a number of malignancies, including Kaposi's sarcoma, non-Hodgkin's lymphoma, and HPV-associated malignancies such as anal cancer and cervical cancer. AIDS-defining illnesses have long included these diagnoses. The increased incidence of malignancies in HIV patients points to the breakdown of immune surveillance as a possible etiology of cancer.[39] Certain other immune deficiency states (e.g. common variable immunodeficiency and IgA deficiency) are also associated with increased risk of malignancy.[40]
Heredity
Most forms of cancer are sporadic, meaning that there is no inherited cause of the cancer. There are, however, a number of recognized syndromes where there is an inherited predisposition to cancer, often due to a defect in a gene that protects against tumor formation. Famous examples are:
- certain inherited mutations in the genes BRCA1 and BRCA2 are associated with an elevated risk of breast cancer and ovarian cancer
- tumors of various endocrine organs in multiple endocrine neoplasia (MEN types 1, 2a, 2b)
- Li-Fraumeni syndrome (various tumors such as osteosarcoma, breast cancer, soft tissue sarcoma, brain tumors) due to mutations of p53
- Turcot syndrome (brain tumors and colonic polyposis)
- Familial adenomatous polyposis an inherited mutation of the APC gene that leads to early onset of colon carcinoma.
- Hereditary nonpolyposis colorectal cancer (HNPCC, also known as Lynch syndrome) can include familial cases of colon cancer, uterine cancer, gastric cancer, and ovarian cancer, without a preponderance of colon polyps.
- Retinoblastoma (eye cancer), when occurring in young children, is due to a hereditary mutation in the retinoblastoma gene.
- Down syndrome patients, who have an extra chromosome 21, are known to develop malignancies such as leukemia and testicular cancer, though the reasons for this difference are not well understood.
Cancers such as the eye cancer retinoblastoma, the breast cancer type known as "early-onset breast cancer," and a type of colon cancer are among those known to be linked to certain genes that can be tracked within a family, showing that the inheritance of certain genes make make a person susceptible to certain cancers.[1]
Other causes
Excepting the rare transmissions that occur with pregnancies and only a marginal few organ donors, cancer is generally not a transmissible disease. The main reason for this reality is the tissue graft rejection caused by MHC incompatibility.[41] In humans and other vertebrates, the immune system uses MHC antigens to differentiate between "self" and "non-self" cells because these antigens are different from person to person. When non-self antigens are encountered, the immune system reacts against the appropriate cell. Such reactions may protect against tumor cell engraftment by eliminating implanted cells. In the United States, approximately 3,500 pregnant women have a malignancy annually, and transplacental transmission of acute leukaemia, lymphoma, melanoma, and carcinoma from mother to fetus has been observed.[41] The development of donor-derived tumors from organ transplants is exceedingly rare. The main cause of organ transplant associated tumors seems to be malignant melanoma that was undetected at the time of organ harvest.[42] though other cases exist.
In non-humans, a few types of transmissible cancer have been described, wherein the cancer spreads between animals by transmission of the tumor cells themselves. This phenomenon is seen in dogs with Sticker's sarcoma, also known as canine transmissible venereal tumor,[43] as well as Devil facial tumor disease in Tasmanian devils.
Signs and symptoms
Roughly, cancer symptoms can be divided into three groups:
- Local symptoms: unusual lumps or swelling (tumor), hemorrhage (bleeding), pain, and/or ulceration. Compression of surrounding tissues may cause symptoms such as jaundice (yellowing of the eyes and skin).
- Symptoms of metastasis (spreading): enlarged lymph nodes, cough and hemoptysis, hepatomegaly (enlarged liver), bone pain, fracture of affected bones, and neurological symptoms. Although advanced cancer may cause pain, it is often not the first symptom.
- Systemic symptoms: weight loss, poor appetite, fatigue and cachexia (wasting), excessive sweating (night sweats), anemia and specific paraneoplastic phenomena, i.e. specific conditions that are due to an active cancer, such as thrombosis or hormonal changes.
Every symptom in the above list can be caused by a variety of conditions (a list of which is referred to as the differential diagnosis). Cancer may be a common or uncommon cause of each item.
A progressive disease, cancer goes through several stages and each stage may express a number of symptoms. Although the numerous types of cancer produce a diversity of symptoms, the American Cancer Society has established seven symptoms as possible warning signs (although these can be produced by many other diseases as well):[1]
- change in size, shape, or color of a mole or wart
- a sore that fails to heal
- persistent sore throat, cough, or hoarseness
- lump, or thickening, in the breast or other location
- unusually discharge or bleeding
- chronic difficulty in swallowing or indigestion
- change in bladder or bowel habits
Many cancers may not exhibit any early symptoms, including breast cancer, showing the importance of routine screening.
Diagnosis
Most cancers are initially recognized either because signs or symptoms appear or through screening, such as via mammography (for breast cancer), pap smear (for cervical cancer), PSA test (for prostate cancer), sigmoidoscopy (for colorectal cancer), and self-examinations. None of these leads to a definitive diagnosis, which usually requires the opinion of a pathologist, a type of physician (medical doctor) who specializes in the diagnosis of cancer and other diseases. People with suspected cancer are investigated via a complete medical history and with medical tests. These medical tests commonly include blood tests, X-rays, CT scans, MRIs, and endoscopy, with the most definitive being removal of a piece of tissue to be examined microscopically. Initially, a doctor may also feel and apply pressure to various parts of the body to see any variations from normal size and feel and inspect areas such as the oral cavity or mouth, looking for abnormalities in color, texture, or moisture or look for sores and thickenings, etc.
Pathology
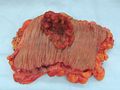
A cancer may be suspected for a variety of reasons, but the definitive diagnosis of most malignancies must be confirmed by histological examination of the cancerous cells by a pathologist. Tissue can be obtained from a biopsy or surgery. Many biopsies (such as those of the skin, breast or liver) can be done in a doctor's office. Biopsies of other organs are performed under anesthesia and require surgery in an operating room.
The tissue diagnosis given by the pathologist indicates the type of cell that is proliferating, its histological grade, genetic abnormalities, and other features of the tumor. Together, this information is useful to evaluate the prognosis of the patient and to choose the best treatment. Cytogenetics and immunohistochemistry are other types of testing that the pathologist may perform on the tissue specimen. These tests may provide information about the molecular changes (such as mutations, fusion genes, and numerical chromosome changes) that has happened in the cancer cells, and may thus also indicate the future behavior of the cancer (prognosis) and best treatment.
Treatment and management
Many treatment/management options for cancer exist including: chemotherapy, radiation therapy, surgery, immunotherapy, monoclonal antibody therapy, hormone therapy, and other methods. Which are used depends upon the location and grade of the tumor and the stage of the disease, as well as the general state of a person's health. Experimental cancer treatments are also under development. Complete removal of the cancer without damage to the rest of the body is the goal of treatment.
Surgery is used to remove the visible tumor and is effective when the cancer is small and confined. However, the propensity of cancers to invade adjacent tissue or to spread to distant sites by microscopic metastasis often limits its effectiveness. Surgery often required the removal of a wide surgical margin or a free margin. The width of the free margin depends on the type of the cancer, the method of removal (CCPDMA, Mohs surgery, POMA, etc.). The margin can be as little as 1 mm for basal cell cancer using CCPDMA or Mohs surgery, to several centimeters for aggressive cancers.
Chemotherapy—the use of drugs to kill cancer cells—can be used to destroy cancer cells that are hard to detect and that have spread. The effectiveness of chemotherapy is often limited by toxicity to other tissues in the body.
Radiation, designed to kill cancer cells, can be applied externally or internally. It also can cause damage to normal tissue.
Immunotherapy uses substances produced the body's own immune system to destroy cancer cells, such as the use of interferons nd interleukins, and monoclonal antibodies. Vaccines are used to boost the bodies immune system and help the immune cells to identify and specifically destroy the cancer cells.
Hormone therapy is used to block the product of hormones that may increase the growth of certain cancers, like breast and prostate cancer.
There are also alternative treatments that are available and can be used in conjunction with traditional forms to help the cancer patient, and sometimes are recommended for alleviating some of the side effects of treatments such as chemotherapy and radiation. Among these are acupuncture, massage, reflexology, homeopathy, herbal remedies, and Moxa treatment.
Because "cancer" refers to a class of diseases, it is unlikely that there will ever be a single "cure for cancer" any more than there will be a single treatment for all infectious diseases.[44]
Prognosis
If detected and treated during their early stages, most cancers are curable. Although cancer has a reputation as a deadly disease, and this certainly applies to certain types, advances in medical care have resulted in a good prognosis for many cancer types. For some cancers, the prognosis is substantially better than nonmalignant diseases such as heart failure and stroke.
A person prognosis is impacted by such factors as the type of cancer, the stage of the cancer, the extent to which it has spread (metastasized), the age and general health of the patient, and the type of treatment.[1]
Progressive and disseminated malignant disease has a substantial impact on a cancer patient's quality of life, and many cancer treatments (such as chemotherapy) may have severe side-effects. In the advanced stages of cancer, many patients need extensive care, affecting family members and friends. Palliative care solutions may include permanent or "respite" hospice nursing.
Many governmental and charitable organizations have been established to help patients cope with cancer. These organizations are often involved in cancer prevention, cancer treatment, and cancer research.
Local organizations may offer a variety of practical and support services to people with cancer. Support can take the form of support groups, counseling, advice, financial assistance, transportation to and from treatment, films or information about cancer. Neighborhood organizations, local health care providers, or area hospitals may have resources or services available. Counseling can provide emotional support to cancer patients and help them better understand their illness. Different types of counseling include individual, group, family, peer counseling, bereavement, and patient-to-patient.
Prevention
Cancer prevention, which is defined as active measures to decrease the incidence of cancer,[45] can have considerable success. The World Health Organization reports that more than 30 percent of cancer is preventable by avoiding such key risk factors as tobacco, overweight or obesity, low fruit and vegetable intake, physical inactivity, alcohol, sexually transmitted infection, and air pollution.[4] This avoids known carcinogens or altering their metabolism and advances a lifestyle or diet that modifies cancer-causing factors, while medical intervention (chemoprevention, treatment of pre-malignant lesions) also addresses the disease. The epidemiological concept of "prevention" is usually defined as either primary prevention, for people who have not been diagnosed with a particular disease, or secondary prevention, aimed at reducing recurrence or complications of a previously diagnosed illness.
Modifiable factors
The vast majority of cancer risk factors are environmental or lifestyle-related, leading to the claim that cancer is a largely preventable disease.[46] Examples of modifiable cancer risk factors include alcohol consumption (associated with increased risk of oral, esophageal, breast, and other cancers), smoking (80-85% of individuals with lung cancer have smoked in the past), physical inactivity (associated with increased risk of colon, breast, and possibly other cancers), and being overweight / obese (associated with colon, breast, endometrial, and possibly other cancers). Other lifestyle and environmental factors known to affect cancer risk (either beneficially or detrimentally) include certain sexually transmitted diseases (such as those conveyed by the human papillomavirus), the use of exogenous hormones, exposure to ionizing radiation and ultraviolet radiation from the sun or from tanning beds, and certain occupational and chemical exposures.
Every year, at least 200,000 people die worldwide from cancer related to their workplace.[47] Millions of workers run the risk of developing cancers such as lung cancer and mesothelioma from inhaling asbestos fibers and tobacco smoke, or leukemia from exposure to benzene at their workplaces.[47]
Diet
The consensus on diet and cancer is that obesity increases the risk of developing cancer. A low-fat diet and exercise, which help to control weight, are considered to reduce the risk of breast, colon, and endometrial cancer.[1]
Particular dietary practices often explain differences in cancer incidence in different countries (e.g. gastric cancer is more common in Japan, while colon cancer is more common in the United States.). Studies have shown that immigrants develop the risk of their new country, often within one generation, suggesting a substantial link between diet and cancer.[48]
Certain foods are believed to protect against various cancers. In particular, fruits, vegetables, and grains are believed to offer some protection. Studies have shown, for example, that the fiber in fruits and vegetables correlates with reduction in the risk of colon cancer. In laboratory studies, some compounds found in broccoli, cauliflower, and cabbage (isothiocyanates and dithiolthiones) and in carrots (beta-carotene) are shown to protect against cancer, as do such vitamins as A, C, and E.[1] On the other hand, the EPIC study published in 2010, tracking the eating habits of 478,000 Europeans, suggested that consuming lots of fruits and vegetables may have little if any effect on preventing cancer.[49]
Despite frequent reports of particular substances and foods having a beneficial or detrimental effect on cancer risk, few of these have an established link to cancer. These reports are often based on studies in cultured cell media or animals. Public health recommendations cannot be made based on these studies until they have been validated in an observational (or occasionally a prospective interventional) trial in humans.
Proposed dietary interventions for primary cancer risk reduction generally gain support from epidemiological association studies. Examples of such studies include reports that reduced meat consumption is associated with decreased risk of colon cancer,[50] and reports that consumption of coffee is associated with a reduced risk of liver cancer.[51] Studies have linked consumption of grilled meat to an increased risk of stomach cancer,[52] colon cancer,[53] breast cancer,[54] and pancreatic cancer,[55] a phenomenon that could be due to the presence of carcinogens such as benzopyrene in foods cooked at high temperatures.
A 2005 secondary prevention study showed that consumption of a plant-based diet and lifestyle changes resulted in a reduction in cancer markers in a group of men with prostate cancer who were using no conventional treatments at the time.[56] These results were amplified by a 2006 study. Over 2,400 women were studied, half randomly assigned to a normal diet, the other half assigned to a diet containing less than 20% calories from fat. The women on the low fat diet were found to have a markedly lower risk of breast cancer recurrence, in the interim report of December, 2006.[57]
Some studies have also demonstrated potential links between some forms of cancer and high consumption of refined sugars and other simple carbohydrates.[58][59] Although the degree of correlation and the degree of causality is still debated,[60][61] some organizations have in fact begun to recommend reducing intake of refined sugars and starches as part of their cancer prevention regimens.[62]
In November 2007, the American Institute for Cancer Research (AICR), in conjunction with the World Cancer Research Fund (WCRF), published Food, Nutrition, Physical Activity and the Prevention of Cancer: A Global Perspective, "the most current and comprehensive analysis of the literature on diet, physical activity and cancer".[63] The WCRF/AICR Expert Report lists 10 recommendations that people can follow to help reduce their risk of developing cancer, including the following dietary guidelines: (1) reducing intake of foods and drinks that promote weight gain, namely energy-dense foods and sugary drinks; (2) eating mostly foods of plant origin; (3) limiting intake of red meat and avoiding processed meat; (4) limiting consumption of alcoholic beverages; and (5) reducing intake of salt and avoiding moldy cereals (grains) or pulses (legumes).
Some mushrooms offer an anti-cancer effect, which is thought to be linked to their ability to up-regulate the immune system. Some mushrooms known for this effect include, Reishi,[64][65] Agaricus blazei,[66] Maitake,[67] and Trametes versicolor[68]. Research suggests the compounds in medicinal mushrooms most responsible for up-regulating the immune system and providing an anti-cancer effect, are a diverse collection of polysaccharide compounds, particularly beta-glucans. Beta-glucans are known as "biological response modifiers", and their ability to activate the immune system is well documented. Specifically, beta-glucans stimulate the innate branch of the immune system. Research has shown beta-glucans have the ability to stimulate macrophage, NK cells, T cells, and immune system cytokines.
Vitamins
While effective in some laboratory studies,[1] vitamin supplementation has not been proven effective in the prevention of cancer in actual trials with human beings. The components of food are also proving to be more numerous and varied than previously understood, so patients are increasingly advised to consume fruits and vegetables for maximal health benefits.[69]
Vitamin D. Low levels of vitamin D is correlated with increased cancer risk.[70] Whether this relationship is causal is yet to be determined.[71]
Folic acid. Folic acid supplementation has not been found effective in preventing colon cancer and may increase colon polyps.[72]
Chemoprevention
The concept that medications could be used to prevent cancer is an attractive one, and many high-quality clinical trials support the use of such chemoprevention in defined circumstances.
Daily use of tamoxifen, a selective estrogen receptor modulator (SERM), typically for 5 years, has been demonstrated to reduce the risk of developing breast cancer in high-risk women by about fifty percent. In 2006, a research study was published in which it was noted that the selective estrogen receptor modulator raloxifene has similar benefits to tamoxifen in preventing breast cancer in high-risk women, with a more favorable side effect profile.[73] In this trial, which studied almost 20,000 women, raloxifene had fewer side effects than tamoxifen, though it did permit more DCIS to form.[73]
Finasteride, a 5-alpha-reductase inhibitor, has been shown to lower the risk of prostate cancer, though it seems to mostly prevent low-grade tumors.[74]
The effect of COX-2 inhibitors such as rofecoxib and celecoxib upon the risk of colon polyps have been studied in familial adenomatous polyposis patients[75] and in the general population.[76][77] In both groups, there were significant reductions in colon polyp incidence, but this came at the price of increased cardiovascular toxicity.
Genetic testing
Genetic testing for high-risk individuals is already available for certain cancer-related genetic mutations. Carriers of genetic mutations that increase risk for cancer incidence can undergo enhanced surveillance, chemoprevention, or risk-reducing surgery. Early identification of inherited genetic risk for cancer, along with cancer-preventing interventions such as surgery or enhanced surveillance, can be lifesaving for high-risk individuals.
| Gene | Cancer types | Availability |
|---|---|---|
| BRCA1, BRCA2 | Breast, ovarian, pancreatic | Commercially available for clinical specimens |
| MLH1, MSH2, MSH6, PMS1, PMS2 | Colon, uterine, small bowel, stomach, urinary tract | Commercially available for clinical specimens |
Vaccination
Prophylactic vaccines have been developed to prevent infection by oncogenic infectious agents, such as viruses, and therapeutic vaccines are in development to stimulate an immune response against cancer-specific epitopes.[78]
As reported above, a preventive human papillomavirus vaccine exists that targets certain sexually transmitted strains of human papillomavirus that are associated with the development of cervical cancer and genital warts. The only two HPV vaccines on the market as of 2009 are Gardasil and Cervarix.[78] These protect against two types of HPV (types 16 and 18) that cause about 70 percent of all cases of cervical cancer worldwide. There is also a hepatitis B vaccine, which prevents infection with the hepatitis B virus, an infectious agent that can cause liver cancer.[78] A canine melanoma vaccine has also been developed.[79]
Screening
Cancer screening is an attempt to detect unsuspected cancers in an asymptomatic population. Screening tests suitable for large numbers of healthy people must be relatively affordable, safe, noninvasive procedures with acceptably low rates of false positive results. If signs of cancer are detected, more definitive and invasive follow up tests are performed to confirm the diagnosis. Screening for cancer can lead to earlier diagnosis in specific cases.
A number of different screening tests have been developed for different malignancies, including for cancers of the breast, rectum, colon, prostate, testis, tongue, skin, and mouth at early stages. Among screening tests recommended by the American Cancer Society are mammography for breast cancer, Pap smear for cervical cancer, sigmoidoscopy for colorectal cancer, and the PSA test for prostate cancer.[1] Self-examinations can be used for cancers of the mouth, breast, skin, and testis.[1] Screening for breast cancer with mammograms has been shown to reduce the average stage of diagnosis of breast cancer in a population. Stage of diagnosis in a country has been shown to decrease within ten years of introduction of mammographic screening programs. Colorectal cancer can be detected through fecal occult blood testing and colonoscopy, which reduces both colon cancer incidence and mortality, presumably through the detection and removal of pre-malignant polyps. Similarly, cervical cytology testing (using the Pap smear) leads to the identification and excision of precancerous lesions. Over time, such testing has been followed by a dramatic reduction of cervical cancer incidence and mortality. Testicular self-examination is recommended for men beginning at the age of 15 years to detect testicular cancer. Prostate cancer can be screened using a digital rectal exam along with prostate specific antigen (PSA) blood testing, though some authorities (such as the US Preventive Services Task Force) recommend against routinely screening all men.
Screening for cancer is controversial in cases when it is not yet known if the test actually saves lives. The controversy arises when it is not clear if the benefits of screening outweigh the risks of follow-up diagnostic tests and cancer treatments. For example: when screening for prostate cancer, the PSA test may detect small cancers that would never become life threatening, but once detected will lead to treatment. This situation, called overdiagnosis, puts men at risk for complications from unnecessary treatment such as surgery or radiation. Follow up procedures used to diagnose prostate cancer (prostate biopsy) may cause side effects, including bleeding and infection. Prostate cancer treatment may cause incontinence (inability to control urine flow) and erectile dysfunction. Similarly, for breast cancer, there have been criticisms that breast screening programs in some countries may not be worthwhile overall. This is because screening of women in the general population will result in a large number of women with false positive results, which require extensive follow-up investigations to exclude cancer, leading to having a high number-to-treat (or number-to-screen) to prevent or catch a single case of breast cancer early.
Cervical cancer screening via the Pap smear has the best cost-benefit profile of all the common forms of cancer screening from a public health perspective. As a type of cancer largely caused by a virus, cervical cancer has clear risk factors (sexual contact), and the natural progression of cervical cancer is that it normally spreads slowly over a number of years, therefore giving more time for the screening program to catch it early. Moreover, the test is easy to perform and relatively cheap.
For these reasons, it is important that the benefits and risks of diagnostic procedures and treatment be taken into account when considering whether to undertake cancer screening.
Use of medical imaging to search for cancer in people without clear symptoms is similarly marred with problems. There is a significant risk of detection of what has been called an incidentaloma—a benign lesion that may be interpreted as a malignancy and be subjected to potentially dangerous investigations.
Research
Cancer research is the scientific effort to understand disease processes and discover possible therapies. The improved understanding of molecular biology and cellular biology due to cancer research has led to a number of new, effective treatments for cancer since President Nixon declared "War on Cancer" in 1971.
Leading cancer research organizations and projects include the American Association for Cancer Research, the American Cancer Society (ACS), the American Society of Clinical Oncology, the European Organisation for Research and Treatment of Cancer, the National Cancer Institute, the National Comprehensive Cancer Network, and The Cancer Genome Atlas project at the NCI.
Notes
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 R. Carson-DeWitt, "Cancer," in J. L. Longe, The Gale Encyclopedia of Medicine, 3rd edition, volume 2. (Detroit, MI: Thomson Gale, 2006, ISBN 978-1414403687), 631-638.
- ↑ K. W. Kinzler and B. Vogelstein, The Genetic Basis of Human Cancer (New York: McGraw-Hill, Medical Pub. Division, 2002, ISBN 978-0071370509).
- ↑ 3.0 3.1 P.H. Raven, G.B. Johnson, J.B. Raven, K.A. Mason, and S.R. Singer, Biology (Boston: McGraw Hill, 2008, ISBN 978-0072965810).
- ↑ 4.0 4.1 4.2 World Health Organization, "Cancer," World Health Organization. Retrieved Aigist 8, 2022.
- ↑ American Cancer Society, "The History of Cancer," American Cancer Society. Retrieved August 8, 2022.
- ↑ Stella Tsolakidou, What Ancient Greek Physicians Knew About Cancer, Greek Reporter, November 17, 2013. Retrieved August 8, 2022.
- ↑ A. Karpozilos, and N. Pavlidis, "The treatment of cancer in Greek antiquity," European Journal of Cancer 40 (2004, issue 14): 2033–2040.
- ↑ P. Skinner, "Unani-tibbi," in K. Krapp and J. L. Longe (eds.), Encyclopedia of Alternative Medicine (Gale, 2001, ISBN 0787649996).
- ↑ M. Yalom, "A history of the breast" (New York: Alfred A. Knopf, 1997, ISBN 0679434593).
- ↑ J. M. Grange, J. L. Stanford, and C. A. Stanford, "Campbell De Morgan's 'Observations on cancer', and their relevance today," Journal of the Royal Society of Medicine 95 (2002, issue 6): 296–299.
- ↑ T. Boveri, "Concerning the origin of malignant tumours," Journal of Cell Science 121 (2008, Supplement 1):1-84.
- ↑ 12.0 12.1 12.2 12.3 12.4 A. Jemal, R. Siegel, E. Ward, et al., "Cancer statistics, 2008," CA Cancer J Clin 58(2008): 71–96.
- ↑ J. G. Gurney, M. A. Smith, and J. A. Ross, "Cancer among infants," in L. A. G. Ries, M. A. Smith, J. G. Gurney, M. Linet, T. Tamra, J. L. Young, and G. R. Bunin (eds.), Cancer Incidence and Survival among Children and Adolescents, United States SEER program 1975–1995 (Bethesda, MD: National Cancer Institute, SEER Program, 1999), 149-156. NIH Pub. No 99-4649. Retrieved August 8, 2022.
- ↑ 14.0 14.1 S. R. Rheingold, A. I. Neugut, and A. T. Meadows, "Secondary cancers: Incidence, risk factors, and management," in James F. Holland, Donald W. Kufe, Raphael E. Pollock, Ralph R. Weichselbaum, Emil Frei, and Robert C. Bast (eds.), Cancer Medicine, edition 5. (Hamilton, ON: BC Decker, 2000, ISBN 1550091131).
- ↑ D. A. Nelson, T. T. Tan, A. B. Rabson, D. Anderson, K. Degenhardt, and E. White, "Hypoxia and defective apoptosis drive genomic instability and tumorigenesis," Genes & Development 18(2004, issue 17): 2095–107.
- ↑ L. M. Merlo, J. W. Pepper, B. J. Reid, and C. C. Maley, "Cancer as an evolutionary and ecological process," Nat. Rev. Cancer 6(2006, issue 12): 924–935.
- ↑ C. M. Croce, "Oncogenes and cancer," The New England Journal of Medicine 358(2008, issue 5): 502–511. Retrieved August 8, 2022.
- ↑ A. G. Knudson, "Two genetic hits (more or less) to cancer," Nature Reviews. Cancer 1(2001, issue 2): 157–162.
- ↑ H. K. Seitz, G. Pöschl, and U. A. Simanowski, "Alcohol and cancer," Recent Developments in Alcoholism 14(1998): 67–95.
- ↑ 20.0 20.1 A. J. Sasco, M. B. Secretan, and K. Straif, "Tobacco smoking and cancer: A brief review of recent epidemiological evidence," Lung Cancer 45(2004, Suppl 2): S3–59.
- ↑ H. K. Biesalski, B. Bueno de Mesquita, A. Chesson, et al., "European Consensus Statement on Lung Cancer: Risk factors and prevention," CA Cancer J. Clin 48(1998, issue 3): 167–176.
- ↑ H. Kuper, P. Boffetta, and H. O. Adami, "Tobacco use and cancer causation: Association by tumour type," Journal of Internal Medicine 252(2002, issue 3): 206–224.
- ↑ 23.0 23.1 H. Kuper, H. O. Adami, and P. Boffetta, "Tobacco use, cancer causation and public health impact," Journal of Internal Medicine 251(2002, issue 6): 455–466.
- ↑ R. N. Proctor, "The global smoking epidemic: A history and status report," Clinical Lung Cancer 5(2004, issue 6): 371–376.
- ↑ K. M. O'Reilly, A. M. Mclaughlin, W. S. Beckett, and P. J. Sime, "Asbestos-related lung disease," American Family Physician 75(2007, issue 5): 683–688.
- ↑ J. E. Muscat, and E. L. Wynder, "Cigarette smoking, asbestos exposure, and malignant mesothelioma," Cancer Res. 51(1991, issue 9): 2263–2267. Retrieved August 8, 2022.
- ↑ D. R. English, B. K. Armstrong, A. Kricker, and C. Fleming, "Sunlight and cancer, " Cancer Causes & Control 8(1997, issue 3): 271–283.
- ↑ A. Berrington de González, M. Mahesh, K. P. Kim, et al., "Projected cancer risks from computed tomographic scans performed in the United States in 2007," Arch. Intern. Med. 169(2009, issue 22): 2071–2077.
- ↑ M. Feychting, A. Ahlbom, and L. Kheifets, "EMF and health," Annual Review of Public Health 26(2005): 165–189.
- ↑ National Cancer Institute, "Cell phones and cancer risk," National Cancer Institute, May 27, 2016. Retrieved August 8, 2022.
- ↑ J. S. Pagano, M. Blaser, M. A. Buendia, et al., "Infectious agents and cancer: Criteria for a causal relation," Semin. Cancer Biol. 14(2004, issue 6): 453–471).
- ↑ H. zur Hausen, "Viruses in human cancers," Science 254(1991, issue 5035): 1167–1173.
- ↑ S. Peter, and C. Beglinger, "Helicobacter pylori and gastric cancer: The causal relationship," Digestion 75(2007, issue 1): 25–35.
- ↑ C. Wang, Y. Yuan, and R. H. Hunt, "The association between Helicobacter pylori infection and early gastric cancer: A meta-analysis," Am. J. Gastroenterol. 102(2007, issue 8): 1789–1798.
- ↑ T. K. Cheung, H. H. Xia, and B. C. Wong, "Helicobacter pylori eradication for gastric cancer prevention," J. Gastroenterol. 42(2007, Suppl 17): 10–15.
- ↑ 36.0 36.1 Dimitropoulou et al., "Sexual activity and prostate cancer risk in men diagnosed at a younger age" BJU International 103(2009, issue 2: 178.
- ↑ Science Daily, "Frequent sex and masturbation in 20s and 30s linked to higher prostate cancer, but risks diminish with age," Science Daily, January 27, 2009. Retrieved August 8, 2022.
- ↑ S. Bhattacharya, "Frequent ejaculation may protect against cancer," New Scientist, April 6, 2004. Retrieved August 8, 2022.
- ↑ C. Wood, and W. Harrington, "AIDS and associated malignancies," Cell Res. 15(2005, issue 11-12): 947–952.
- ↑ L. Mellemkjaer, L. Hammarstrom, V. Andersen, et al., "Cancer risk among patients with IgA deficiency or common variable immunodeficiency and their relatives: A combined Danish and Swedish study," Clin. Exp. Immunol. 130(2002, issue 3): 495–500.
- ↑ 41.0 41.1 J. Tolar, and J. P. Neglia, "Transplacental and other routes of cancer transmission between individuals," J Pediatr Hematol Oncol. 25(2003, issue 6): 430–434.
- ↑ D. Dingli, and M. A. Nowak, "Cancer biology: Infectious tumor cells," Nature 443(2006, issue 7107): 35–36.
- ↑ C. Murgia, J. K. Pritchard, S. Y. Kim, A. Fassati, and R. A. Weiss, "Clonal origin and evolution of a transmissible cancer," Cell 126(2006, issue 3): 477–487.
- ↑ C. Wanjek, "Exciting new cancer treatments emerge amid persistent myths," Live Science, September 19, 2006. Retrieved August 8, 2022.
- ↑ Mayo Clinic, [hhttps://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/cancer-prevention/art-20044816 "Cancer prevention: 7 steps to reduce your risk,"] MayoClinic.com. Retrieved August 8, 2022.
- ↑ G. Danaei, S. Vander Hoorn, A. D. Lopez, C. J. Murray, and M. Ezzati, "Causes of cancer in the world: Comparative risk assessment of nine behavioural and environmental risk factors," Lancet 366(2005, issue 9499): 1784–1793.
- ↑ 47.0 47.1 World Health Organization, "WHO calls for prevention of cancer through healthy workplaces," World Health Organization (2007). Retrieved August 8, 2022.
- ↑ P. Buell, and J. E. Dunn, "Cancer mortality among Japanese Issei and Nisei of California," Cancer 18(1965): 656–664.
- ↑ P. Boffetta, E. Couto, J. Wichmann, et al., "Fruit and vegetable intake and overall cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC)," J Natl Cancer Inst 8(2010, issue 102): 529-537.
- ↑ M. L. Slattery, K. M. Boucher, B. J. Caan, J. D. Potter, and K. N. Ma, "Eating patterns and risk of colon cancer," J. Epidemiol. 148(1998, issue 1): 4–16.
- ↑ S. C. Larsson, and A. Wolk, "Coffee consumption and risk of liver cancer: A meta-analysis," Gastroenterology 132(2007, issue 5): 1740–1745.
- ↑ M. H. Ward, R. Sinha, E. F. Heineman, et. al., "Risk of adenocarcinoma of the stomach and esophagus with meat cooking method and doneness preference," Int. J. Cancer 71(1997, issue 1): 14–19.
- ↑ R. Sinha, U. Peters, A. J. Cross, et al., "Meat, meat cooking methods and preservation, and risk for colorectal adenoma," Cancer Res. 65(2005, issue 17): 8034–8041. Retrieved August 8, 2022.
- ↑ S. E. Steck, M. M. Gaudet, S. M. Eng, et al., "Cooked meat and risk of breast cancer: Lifetime versus recent dietary intake," Epidemiology 18(2007, issue 3): 373–382.
- ↑ K. E. Anderson, F. F. Kadlubar, M. Kulldorff, et al., "Dietary intake of heterocyclic amines and benzo(a)pyrene: associations with pancreatic cancer," Cancer Epidemiol. Biomarkers Prev. 14(2005, issue 9): 2261–2265.
- ↑ D. Ornish et al., "Intensive lifestyle changes may affect the progression of prostate cancer," The Journal of Urology 174(2005, issue 3): 1065–1069.
- ↑ R. T. Chlebowski, G. L. Blackburn, C. A. Thomson, et al., "Dietary fat reduction and breast cancer outcome: Interim efficacy results from the Women's Intervention Nutrition Study," J. Natl. Cancer Inst. 98(2006, issue 24): 1767–1776.
- ↑ I. Romieu, E. Lazcano-Ponce, L. M. Sanchez-Zamorano, W. Willett, and M. Hernandez-Avila, "Carbohydrates and the risk of breast cancer among Mexican women," Cancer Epidemiol Biomarkers Prev 13(2004, issue 8):1283–1289. Retrieved August 8, 2022.
- ↑ D. S. Michaud, S. Liu, E. Giovannucci, W. C. Willett, G. A. Colditz, and C. S. Fuchs, "Dietary sugar, glycemic load, and pancreatic cancer risk in a prospective study," J Natl Cancer Inst 94(2002, issue 17): 1293-1300. Retrieved August 8, 2022.
- ↑ M. Hitti, "High blood sugar linked to cancer risk," WebMD February 22, 2008. Retrieved August 8, 2022.
- ↑ T. Moynihan, "Cancer causes: Popular myths about the causes of cancer," MayoClinic.com. Retrieved August 8, 2022.
- ↑ Johns Hopkins Bloomberg School of Public Health, "High sugar levels increase cancer and mortality risk," Public Health News Center, January 11, 2005. Retrieved AAugust 8, 2022.
- ↑ World Cancer Research Fund and American Institute for Cancer Research, Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective (WCRF/AICR, 2007, ISBN 978-0972252225).
- ↑ J. W. Yuen, and M. D. Gohel, "Anticancer effects of Ganoderma lucidum: A review of scientific evidence," Nutr Cancer 53(2005, issue 1): 11–17.
- ↑ S. C. Hsu, C. C. Ou, J. W. Li, et al., "Ganoderma tsugae extracts inhibit colorectal cancer cell growth via G(2)/M cell cycle arrest," J Ethnopharmacol 120(2008, issue 3): 394.
- ↑ G. Hetland, E. Johnson, et al., "Effects of the medicinal mushroom Agaricus blazei Murill on immunity, infection and cancer," Scandinavian Journal of Immunology 68(2008, issue 4): 363-370.
- ↑ N. Kodama, K. Komuta, and H. Nanba, "Can maitake MD-fraction aid cancer patients?" Altern Med Rev. 7(2002, issue 3):236-239. Retrieved August 8, 2022.
- ↑ H. Kobayashi, K. Matsunaga, and Y. Oguchi, Antimetastatic effects of PSK (Krestin), a protein-bound polysaccharide obtained from basidiomycetes: An overview," Cancer Epidemiol Biomarkers Prev. 4(1995, issue 3):275-281. Retrieved August 8, 2022.
- ↑ M. Pollan, The Omnivore's Dilemma : A Natural History of Four Meals (New York: Penguin Press, 2006, ISBN 978-1594200823).
- ↑ E. Giovannucci, Y. Liu, E. B. Rimm, et al., "Prospective study of predictors of vitamin D status and cancer incidence and mortality in men," J. Natl. Cancer Inst. 98(2006, issue 7): 451–459.
- ↑ G. G. Schwartz, and W. J. Blot, "Vitamin D status and cancer incidence and mortality: Something new under the sun," J. Natl. Cancer Inst. 98(2006, issue 7): 428–430. Retrieved August 8, 2022.
- ↑ B. F. Cole, J. A. Baron, R. S. Sandler, et al., "Folic acid for the prevention of colorectal adenomas: A randomized clinical trial," JAMA 297(2007, issue 21): 2351–2359.
- ↑ 73.0 73.1 V. Vogel, J. Costantino, D. Wickerham, W. Cronin, R. Cecchini, J. Atkins, T. Bevers, L. Fehrenbacher, E. Pajon, J. Wade, A. Robidoux, R. Margolese, J. James, S. Lippman, C. Runowicz, P. Ganz, S. Reis, W. McCaskill-Stevens, L. Ford, V. Jordan, and N. Wolmark, "Effects of tamoxifen vs raloxifene on the risk of developing invasive breast cancer and other disease outcomes: The NSABP Study of Tamoxifen and Raloxifene (STAR) P-2 trial," JAMA 295(2006, issue 23): 2727–2741.
- ↑ I. Thompson, P. Goodman, C. Tangen, M. Lucia, G. Miller, L. Ford, M. Lieber, R. Cespedes, J. Atkins, S. Lippman, S. Carlin, A. Ryan, C. Szczepanek, J. Crowley, and C. Coltman, "The influence of finasteride on the development of prostate cancer," N Engl J Med 349(2003, issue 3): 215–224.
- ↑ A. Hallak, L. Alon-Baron, R. Shamir, et. al., "Rofecoxib reduces polyp recurrence in familial polyposis," Dig Dis Sci 48(2003, issue 10): 1998–2002.
- ↑ J. Baron, R. Sandler, R. Bresalier, et al., "A randomized trial of rofecoxib for the chemoprevention of colorectal adenomas," Gastroenterology 131(2006, issue 6): 1674–1682.
- ↑ M. Bertagnolli, C. Eagle, A. Zauber, et al., "Celecoxib for the prevention of sporadic colorectal adenomas," N Engl J Med 355(2006, issue 9): 873–884.
- ↑ 78.0 78.1 78.2 National Cancer Institute, "Cancer Treatment Vaccines" National Cancer Institute, September 24, 2019. Retrieved Augusr 8, 2022.
- ↑ J. C. Liao, P. Gregor, J. D. Wolchok, et al., "Vaccination with human tyrosinase DNA induces antibody responses in dogs with advanced melanoma," Cancer Immun. 6(2006): 8.
ReferencesISBN links support NWE through referral fees
- Holland, James F., Donald W. Kufe, Raphael E. Pollock, Ralph R. Weichselbaum, Emil Frei, and Robert C. Bast (eds.). Cancer Medicine, edition 5. Hamilton, ON: BC Decker, 2000. ISBN 1550091131
- Kinzler, K. W., and B. Vogelstein. The Genetic Basis of Human Cancer. New York: McGraw-Hill, Medical Pub. Division, 2002. ISBN 978-0071370509
- Kleinsmith, L. J. Principles of Cancer Biology. Pearson Benjamin Cummings, 2006. ISBN 0805340033
- Krapp, K., and J. L. Longe (eds.). Encyclopedia of Alternative Medicine. Gale, 2001. ISBN 0787649996
- Longe, J. L. The Gale Encyclopedia of Medicine, 3rd edition, volume 2. Detroit, MI: Thomson Gale, 2006. ISBN 978-1414403687
- Pollan, M. The Omnivore's Dilemma : A Natural History of Four Meals. New York: Penguin Press, 2006. ISBN 978-1594200823
- Raven, P.H., G B. Johnson, J.B. Raven, K.A. Mason, and S.R. Singer. Biology. Boston: McGraw Hill, 2008. ISBN 978-0072965810
- Schwab, M. (ed.). Encyclopedia of Cancer. Springer, 2009. ISBN 978-3540368472
- Tannock, I. F., R. P. Hill, et al. (eds.). The Basic Science of Oncology 4th ed. McGraw-Hill, 2005. ISBN 0071387749
- World Cancer Research Fund and American Institute for Cancer Research. Food, Nutrition, Physical Activity and the Prevention of Cancer: a Global Perspective. WCRF/AICR, 2007. ISBN 978-0972252225
External links
All links retrieved November 25, 2023.
- What You Need to Know About Preventing Cancer Through Diet and Lifestyle Life Policy Shopper.
- Alcohol and Prostate Cancer Everlast Recovery Centers
| Tumors (and related structures), Cancer, and Oncology |
| Benign - Premalignant - Carcinoma in situ - Malignant
Topography: Anus - Bladder - Bone - Brain - Breast - Cervix - Colon/rectum - Duodenum - Endometrium - Esophagus - Eye - Gallbladder - Head/Neck - Liver - Larynx - Lung - Mouth - Pancreas - Penis - Prostate - Kidney - Ovaries - Skin - Stomach - Testicles - Thyroid Morphology: Papilloma/carcinoma - Adenoma/adenocarcinoma - Soft tissue sarcoma - Melanoma - Fibroma/fibrosarcoma - Lipoma/liposarcoma - Leiomyoma/leiomyosarcoma - Rhabdomyoma/rhabdomyosarcoma - Mesothelioma - Angioma/angiosarcoma - Osteoma/osteosarcoma - Chondroma/chondrosarcoma - Glioma - Lymphoma/leukemia Treatment: Chemotherapy - Radiation therapy - Immunotherapy - Experimental cancer treatment Related structures: Cyst - Dysplasia - Hamartoma - Neoplasia - Nodule - Polyp - Pseudocyst Misc: Tumor suppressor genes/oncogenes - Staging/grading - Carcinogenesis/metastasis - Carcinogen - Research - Paraneoplastic phenomenon - ICD-O - List of oncology-related terms |
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.